
WE SEE SAME DAY EMERGENCIES! Contact us after hours!
WE SEE SAME DAY EMERGENCIES!
Contact us after hours!


Dos and dont’s after Root Canal Treatment
- November 16, 2023
Dr. Mauricio Chavarriaga
In the aftermath of a root canal procedure, navigating the post-treatment period can be crucial for optimal recovery.
What steps should and shouldn’t be taken following a root canal? We will explore the potential challenges and Agitation that may arise, providing a comprehensive guide on post-treatment care.
From dietary recommendations to oral hygiene practices, this article will offer a detailed Solution to ensure a smooth recovery process.
By the end, you will be equipped with the knowledge needed to make informed decisions, promoting a successful and comfortable healing journey after an Orlando Root Canal .
Table of Contents
What can you do after a root canal treatment.
After undergoing a root canal, proper post-treatment care is essential to ensure a smooth recovery and the long-term success of the procedure. Knowing what to do and what to avoid can significantly impact the healing process. Here are some dos and don’ts to consider:
- Brush gently: Maintain oral hygiene by brushing your teeth gently after the root canal procedure.
- Use a soft-bristled toothbrush: Opt for a soft-bristled toothbrush to avoid irritation to the treated tooth and surrounding area.
- Follow your dentist’s recommendations: Adhere to any specific post-treatment care instructions provided by your dentist to support healing.
- Take prescribed medications: If your dentist prescribes pain relievers or antibiotics, take them as directed to manage discomfort and prevent infection.
- Use over-the-counter pain relievers as recommended: Over-the-counter pain relievers can help manage mild discomfort; however, consult with your dentist before use.
- Choose soft foods: Opt for soft, easy-to-chew foods during the initial days after the procedure to avoid putting excessive pressure on the treated tooth.
- Stay hydrated: Drink plenty of water to stay hydrated, which supports overall healing.
- Keep scheduled appointments: Attend any follow-up appointments with your dentist to monitor the healing progress and address any concerns promptly.
- Monitor for signs of infection: Keep an eye out for symptoms such as persistent pain, swelling, or unusual discharge and contact your dentist if you notice any concerning signs.
Recommended Reading: Is Root Canal Worth It in 2024
These dos provide a foundation for a healthy recovery after a root canal. However, it’s equally important to be aware of the don’ts to prevent potential complications.
Recommended Reading: Root Canal Treatment Side Effects
What can’t you do after a Root Canal therapy?
After undergoing a root canal, knowing what activities to avoid is just as crucial as understanding what actions support recovery. Here are some key don’ts to consider:
- Avoid aggressive brushing: Refrain from aggressive brushing, especially around the treated tooth, to prevent irritation.
- Delay oral hygiene practices: While gentle brushing is recommended, don’t skip oral hygiene routines. Maintain cleanliness to prevent complications.
- Neglect persistent pain: If you experience persistent or worsening pain, don’t ignore it. Contact your dentist promptly for further evaluation.
- Overlook swelling or unusual discharge: Any signs of swelling or unusual discharge should be reported to your dentist immediately.
- Avoid hard or crunchy foods: Steer clear of hard or crunchy foods that may exert excessive pressure on the treated tooth and impede the healing process.
- Avoid skipping prescribed medications: If your dentist prescribes medications, do not skip doses without consulting them. Consistent adherence to the prescribed regimen is essential for effective pain management and infection prevention.
- Skip follow-up appointments: Avoid skipping any scheduled follow-up appointments. These visits are crucial for your dentist to assess your recovery progress and address any emerging issues promptly.
Recommended Reading: Root Canal Stages
By adhering to these dos and don’ts, you contribute to a smoother recovery process after a root canal treatment.
Recommended Reading: What Food Eat and Avoid after Root Canal Treatment
Dos and Don’ts After Root Canal FAQs
Can you drive after a root canal.
Yes, you can generally drive after a root canal. The procedure itself doesn’t impair your ability to operate a vehicle. However, if you’ve been prescribed medication that may affect your alertness, it’s advisable to arrange for someone else to drive.
Recommended Reading: How Many Root Canals can you have
Can You Drink Alcohol After a Root Canal?
It’s best to avoid alcohol immediately after a root canal, especially if you are taking prescribed medications. Alcohol can interfere with the effectiveness of certain medications and may exacerbate post-treatment discomfort.
Recommended Reading: How Many Times Can a Root Canal Be Retreated
Can You Fly After a Root Canal?
Flying after a root canal is generally acceptable. However, it’s essential to consider any post-treatment discomfort and potential changes in air pressure, which could affect the treated tooth. Consult with your dentist before making travel plans.
Can You Get Dry Socket From a Root Canal?
No, dry socket is a complication typically associated with tooth extractions, not root canals. The procedure involves sealing the treated tooth, reducing the risk of complications like dry socket.
Recommended Reading: How Bad Does a Root Canal Hurt 1-10
Can You Talk After a Root Canal?
Yes, you can talk after a root canal. While some initial discomfort or swelling may affect speech, it’s generally temporary. Speaking should become more comfortable as the healing progresses.
Recommended Reading: Why Root Canals Need 2 visits?

Can You Use a Straw After a Root Canal?
It’s advisable to avoid using a straw immediately after a root canal. Suction created by a straw can disrupt the healing process and potentially dislodge the blood clot in the treated area.
Can You Workout After a Root Canal?
Gentle workouts are generally acceptable after a root canal. However, strenuous exercise should be avoided on the day of the procedure. Listen to your body, and if you experience discomfort, consider lighter activities.
Recommended Reading: Root Canal Average Age
Where to get Root Canal Treatment in Orlando?
If you’re in need of root canal treatment in Orlando ,consider visiting East Orange Endodontics. We´ve +30 years of experience and +450 positive reviews. Contact Us! We’ll be in touch with you in less than 10 minutes.

How Long After a Root Canal Can You Smoke?
It’s best to refrain from smoking for at least 48 hours after a root canal. Smoking can introduce irritants to the healing site, potentially leading to complications. Longer periods without smoking are even more beneficial.
Can You Use Mouthwash After a Root Canal?
Yes, you can use an alcohol-free, gentle mouthwash after a root canal. Avoiding alcohol-based mouthwashes during the initial healing phase helps prevent irritation and supports the recovery process.
Recommended Reading: Can You See a Failed Root Canal on X-ray
Can I Eat Pizza After a Root Canal?
Soft, non-crunchy foods are advisable immediately after a root canal. While pizza can be enjoyed, it’s wise to choose slices without hard or crunchy toppings during the initial recovery period.
Can I Wear My Retainer After a Root Canal?
Wearing your retainer is generally acceptable after a root canal. Ensure it doesn’t exert excessive pressure on the treated tooth, and if you experience discomfort, consult your dentist.
Recommended Reading: Types of Root Canal
Can I Use Listerine After Root Canal?
Yes, you can use alcohol-free Listerine or a prescribed antimicrobial mouthwash after a root canal. This helps maintain oral hygiene without causing irritation to the treated area.
Can You Brush After Root Canal?
Gentle brushing is recommended after a root canal. Use a soft-bristled toothbrush, and avoid vigorous brushing around the treated tooth to prevent irritation.
Can You Kiss After a Root Canal?
Kissing is generally acceptable after a root canal, but be mindful of any tenderness or swelling around the treated area. Gentle affection is advisable to avoid discomfort.
If you’re in need of root canal in Orlando ,consider visiting East Orange Endodontics. We´ve +30 years of experience and +450 positive reviews. Contact Us! We’ll be in touch with you in less than 10 minutes.

Top Rated Root Canal

- Root Canal Retreatment
Dental Service
Related Posts

How many visits for a root canal
The prospect of undergoing a root canal procedure can be daunting, with questions lingering about the duration and number of

Root Canal Treatment NHS vs Root Canal Treatment Private: Which Is The Better Option?
For many, facing the need for endodontics raises questions about whether to opt for NHS or private dental care. The

Root Canal vs Endodontic Treatment: Which Is The Better Option?
Facing dental problems such as severe decay or infection often leads to the consideration of treatments such as endodontics or
Let's save your tooth
We will get in touch as soon as possible!
- East Orlando 10800 Dylan Loren Cir Suite 103, Orlando, FL 32825, United States
- Lake Nona 10007 Wellness Way Suite 130, Orlando, FL 32832, United States
- [email protected]
- +1 (407) 704-7863
- Fax: (321) 248-0330
Our services
- Orlando Root Canal
- General Consultation
- CT-Scans and X rays
Opening hours
- Monday-Thursday: 7:45am to 5pm
- Friday: 7:45am to 2pm

Experiencing Tooth Pain? Book your Root Canal in Orlando, FL
Over 100,000 Root Canals Performed
30+ Years of Award-Winning Expertise
Top-Rated Endodontist
Choose proven experience !
- Skip to main content
- Skip to header right navigation
- Skip to after header navigation
- Skip to site footer

Ask the Dentist
Health Begins in the Mouth | Dr. Mark Burhenne
Every product I recommend meets my rigorous safety and testing standards. When you buy through links on my website, I may earn a small commission which helps offset the costs of running this website. Learn more →
Root Canals: Know Before You Go [Plus, Alternatives]
Get Dr. B’s Dental Health Tips
Do you need a root canal if there’s no pain , what to ask before agreeing to treatment, before the procedure, during the procedure, getting a crown or filling, antibiotics & root canal therapy, how long can i go before getting a root canal, root canal recovery, pain after a root canal, root canal cost, complications of root canal therapy, prognosis & long-term outlook, are root canals safe , pros & cons of root canal treatment, root canal prevention, root canal vs. fillings, root canal vs. extraction , root canal vs. regenerative endodontics.
A root canal is a common dental treatment for a tooth with inflamed or infected pulp, usually due to a deep cavity or trauma to the tooth.
Few dental treatments inspire fear like the root canal. But unlike what you might see in the movies , root canal treatment is associated with very little pain.
On the other hand, root canals do carry some risks. They are often prescribed when another treatment is more appropriate or should be preferred. Biological dentists, in particular, generally avoid this procedure and recommend alternatives.
Below, we discuss exactly what a root canal is, how to know if it’s right for you, what to expect, and other common questions.
IF YOU PURCHASE A PRODUCT USING A LINK BELOW, WE MAY RECEIVE A SMALL COMMISSION AT NO ADDITIONAL COST TO YOU. READ OUR AD POLICY HERE .
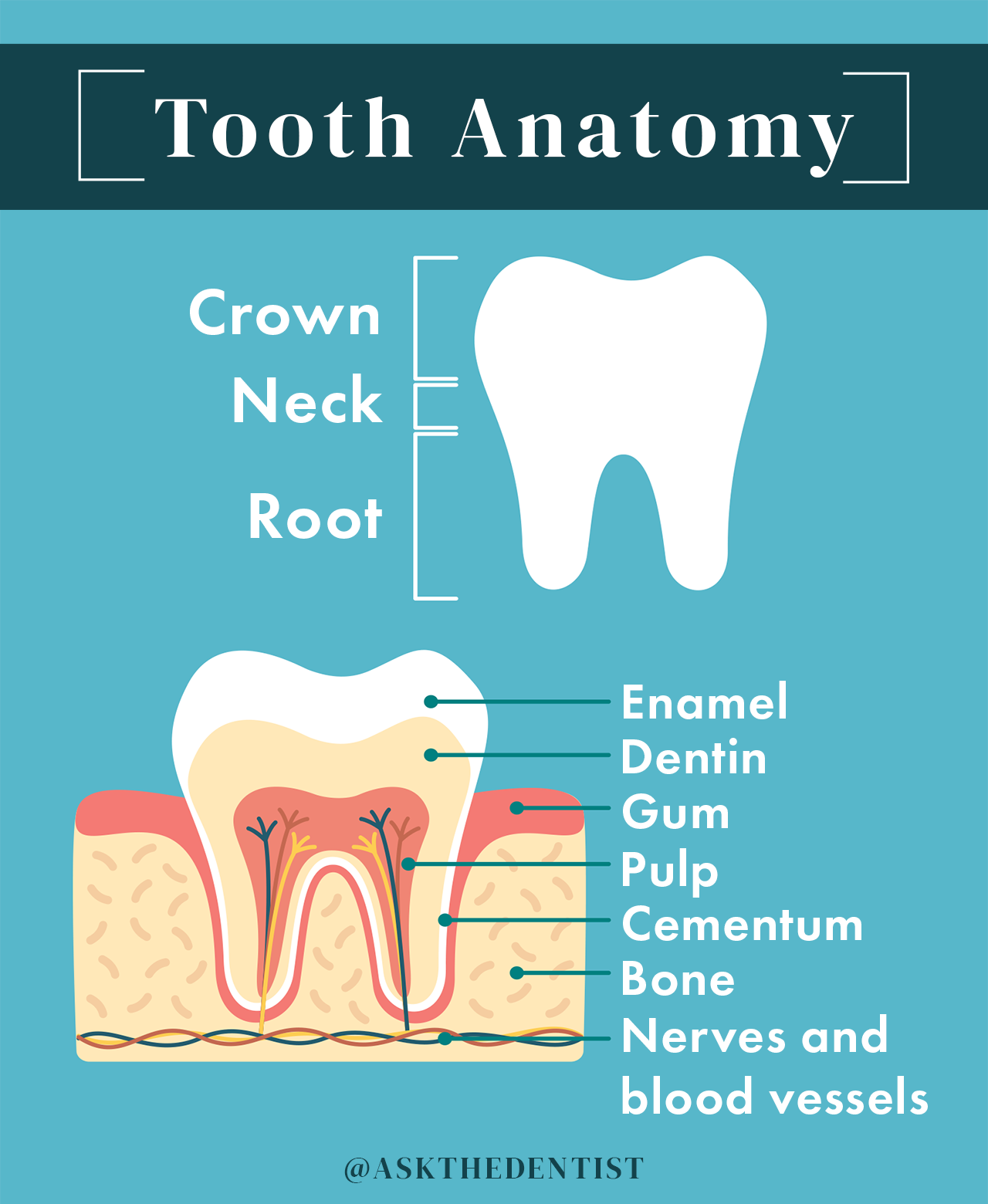
What is a root canal.
Root canal therapy is a type of dental procedure used to preserve a tooth after the pulp of the tooth has become inflamed or infected. This is typically caused by a deep cavity or physical trauma to the face or teeth.
Dental pulp is the soft tissue found inside the tooth containing connective tissue, nerves, and blood vessels.
During a root canal, a dentist or endodontist will clean out the infected tissue from your pulp chamber, then disinfect, fill, and seal the tooth. In most cases, a crown will be placed on top of the tooth structure to prevent cracking or chipping .
A root canal procedure allows your dentist to preserve (not save) an infected tooth by removing infected tissue and sealing it.
Root canal procedures may also be referred to as:
- Root canals
- Endodontic treatment
- Root canal therapy
- Root canal treatment
Root canals are an appropriate treatment for a tooth with irreversible pulpitis.
Pulpitis, or inflammation of the tooth pulp, can be reversible or irreversible. Once the nerve tissue has died as the pulp’s infection has spread, irreversible pulpitis results.
At that point, a tooth cannot be saved as a living structure.
A root canal procedure can “preserve” a tooth, but not “save” it.
By the time you need a root canal, it’s too late to save the life of the tooth because it’s already infected and dying.
Some people refer to this as “mummifying” a dead tooth.
Preserving tooth structure benefits your oral health because it won’t affect orthodontic growth or your bite. If your dentist extracts a diseased tooth without filling its space with an implant, your teeth may shift and cause orthodontic problems.
The most common risk of root canal treatment is tooth fracture. The inside of the tooth has been scraped out, leaving the outer shell of the tooth dry, brittle, and prone to breakage.
That’s why a root canal procedure almost always requires a second procedure shortly afterward: a dental crown . A root canaled tooth needs the protection of a crown because you’ve carved out the tissue inside it.
A dental crown is a rigid covering, formed to look like a natural tooth, that is stronger than enamel. It preserves the structural integrity of the tooth and reduces the risk that it will break as it weakens over time.
Free weekly dental health advice in your inbox, plus 10 Insider Secrets to Dental Care as a free download when you sign up

How do you know if you need a root canal?
What causes the need for root canal treatment ? Irreversible pulpitis (infection and inflammation of dental pulp) is what caused the need for a root canal or similar treatment option. This is usually caused by a deep cavity or injury/trauma to the tooth.
Irreversible pulpitis cannot be healed or reversed by any natural or conventional means.
In the case of tooth decay , you may be able to catch pulpitis before it becomes irreversible. To increase your chances of catching it early, practice good dental care, don’t skip dental checkups, and talk to your dentist anytime you develop a toothache .
Signs you need a root canal may include:
- Tooth pain: Pulpitis will cause pain that may be persistent or come and go. It may be worse when you eat or bite down. Lingering pain, or pain caused by hot or cold stimuli that remains for several minutes or hours, is a telltale sign of irreversible pulpitis and the need for a root canal. Positional pain that occurs when you stand up, lay down, or run in place, may indicate a tooth abscess and a root canal. Spontaneous pain that happens without warning may also indicate an inflamed pulp. It’s possible for pulpitis to cause referred tooth pain that manifests in other teeth or your ear, face, or jaw.
- Bump on the gum (fistula): A fistula is a small white, yellow, or red pimple-like bump that appears on the gum. This tells your dentist that there is an infection because pus, blood, and infectious materials are trying to get out and the body is trying to “vent” them. The problem is that a fistula can mislead a dentist as to which tooth needs a root canal — it doesn’t always appear next to the infected tooth.
- Swollen gums: As an infected tooth tries to “vent” the toxic results of infection, it may also cause gums to swell, redden, and become tender.
- Color change of the tooth or gums: A dead or dying tooth may turn grayish over time as its blood supply diminishes. This is more likely to be noticeable on a front tooth than a back one. The infection can also darken the gums around the tooth.
- Loosening tooth: As infection spreads, it may soften or degrade the bone in which the tooth sits. This can cause your tooth to become more mobile, wiggling upon contact.
- Cracked tooth: If your tooth has a crack that extends down into the tooth root, it is usually impossible to save the tooth and it must be treated with a root canal or an alternative treatment option.
- Deep cavity: A cavity can cause many of the signs above, such as pain. Your dentist may use x-rays or a cone-beam CT (CBCT) to diagnose the extent of your tooth decay.
- Tooth abscess: Also known as a periapical abscess, this pus-filled infectious area beneath the tooth root occurs as a result of irreversible pulpitis, often due to an untreated cavity. This is not the same thing as a periodontal (gum) abscess, which may not suggest the need for a root canal.
- Dark blood from the pulp: When your dentist opens your toot for a root canal, he or she may be able to identify irreversible pulpitis from visibly darker blood than usual.
- Red-yellow pus: Not all inflamed teeth bleed. Often, a sure sign of irreversible pulpitis upon opening the tooth is oozing, reddish-yellow pus.
Diagnosing a root canal is a complex process that differs between dentists. There is no cut-and-dry way to diagnose a root canal. This process is part science, part art form, to discover the degree of infection within a tooth.
If your dentist identifies irreversible pulpitis, you will need a root canal regardless of whether or not pain is present.
Your tooth nerve may die, temporarily relieving pain. Your dentist may put you on antibiotics that shrink the infection, which would also cause pain to subside.
However, irreversible pulpitis must be treated by root canal or extraction. Otherwise, it can cause serious systemic health issues.
In my practice, I’ve met many patients who were prescribed root canal therapy because a practitioner was in a hurry or looking for the “simplest” option, rather than the best option.
For instance, a dentist may suggest a root canal for a large cavity even if the pulp is not irreversibly inflamed and a filling would suffice.
Dental insurance covers it, the general dentist doesn’t have to place a filling that requires more-than-average finesse, and — I hate to say it, but it’s true — the price tag is higher.
I highly recommend asking your dentist the following questions before you say yes to a root canal to prevent unnecessary dental work:
- Is a root canal absolutely necessary?
- Is it possible the tooth will recover and not need the root canal?
- How did you come to the conclusion that I have irreversible pulpitis?
- Why did the pulp die?
- What if I don’t do the root canal?
- Should I skip the root canal and go right to the extraction and implant?
- Will my infection spread to other teeth or to my bone?
- How confident are you that a root canal will be successful?
- Should I have this done by a specialist or can you do as good of a job as a specialist can?
In general, many root canal symptoms can often be attributed to causes other than irreversible pulpitis. Until your dentist or endodontist is fairly certain that irreversible pulpitis is to blame, root canal treatment should not be prescribed .
What to Expect During a Root Canal Procedure
A root canal procedure can be done in 1 or 2 visits. For retreatments (in which a tooth has already received endodontic treatment), 3 visits may be requested. Each visit should take 90 minutes or less.
How long does a root canal take? A root canal procedure takes 30-90 minutes per visit. For simple cases of teeth with one root, each visit will probably 60 minutes or less. Complex cases take closer to 90 minutes per visit.
Why do root canals take 2 visits? Depending on the provider’s preference, root canal treatment may be done in 2 or more visits for more thorough cleaning. The number of visits for root canal therapy has no significant impact on pain levels or treatment success rates.
Should your root canal be done by your dentist or a specialist? Specialists in root canal therapy are called endodontists. An endodontist should perform your root canal procedure if you have complex canals or if your general dentist refers out root canal cases. However, all dentists are trained to perform root canals during dental school .
Before your root canal procedure, your dentist will probably take x-rays or a cone-beam CT (CBCT) and perform a physical exam to identify irreversible pulpitis.
Your dentist may prescribe antibiotics before the procedure if:
- You are immune-compromised
- You have an existing tooth abscess
- You present with a fever
- Your infection had a rapid onset
- You have developed a system-wide infection
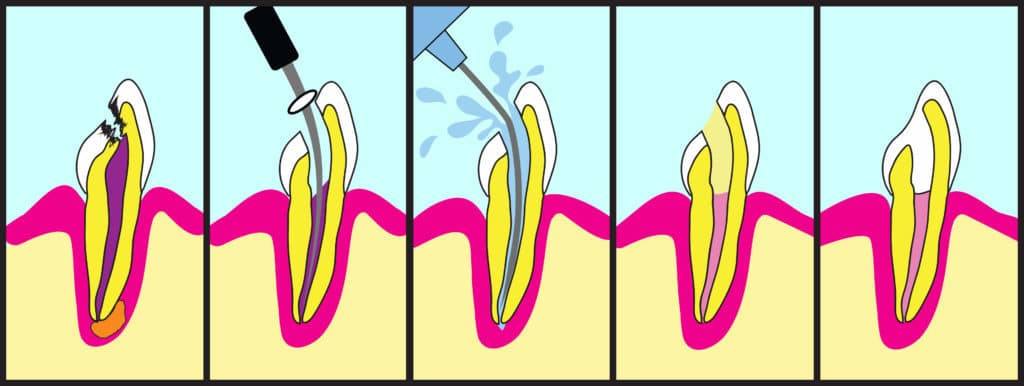
This is how a root canal procedure is performed, step-by-step:
- X-rays and exam: The dentist or endodontist will take a new set of x-rays and perform another physical exam. Many x-rays will be taken to make sure that the instruments are in the correct location to remove the infected tissue.
- Numbing : You will receive full local anesthesia to numb the tooth and surrounding area. This local anesthetic is more than what’s required for a filling because your dentist must remove the nerve. Your dentist will typically not put you under sedation (to sleep) for a root canal, but you can request sedation if you’re anxious.
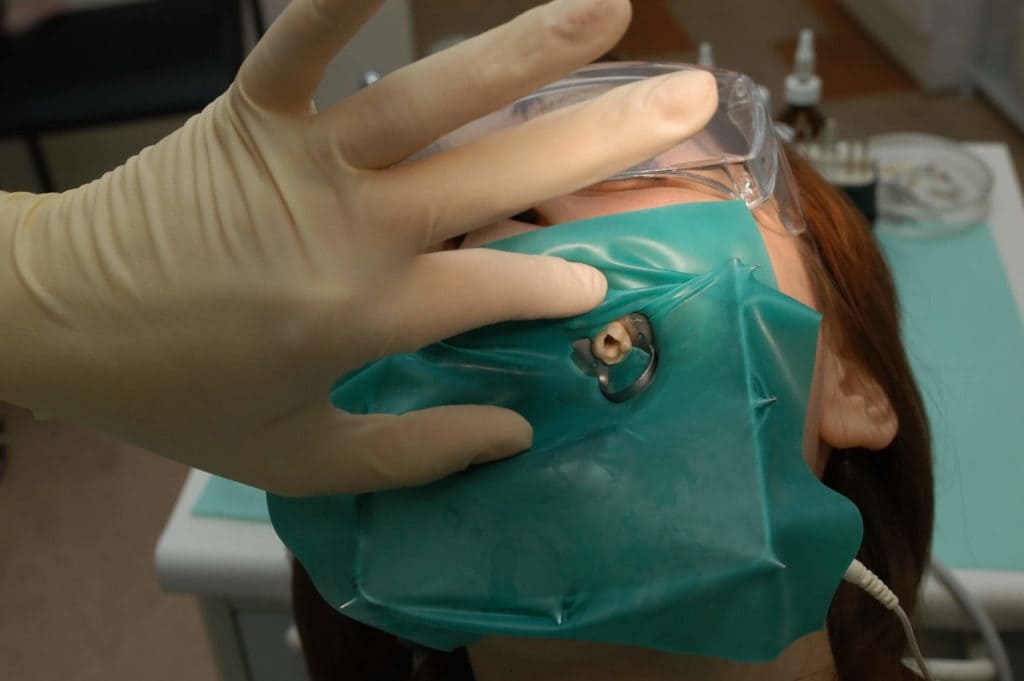
- Rubber dam : A sheet of latex, called a rubber dam, will be placed over your mouth. This prevents bacteria from the rest of your mouth from entering the tooth. The dental dam also stops medications inside the tooth from being swallowed.
- Opening: An opening will be drilled into the top of your tooth.
- Cleaning and shaping: Using very refined drills and files, your dentist will remove the inflamed or infected pulp, carefully cleaning out and shaping the inside of the tooth.
- Irrigation: The main pulp chambers will be irrigated with water and, in most cases, an antibacterial agent to eliminate any remaining bacteria. These chambers must be fully dry before moving on to the next step.
- Filling: Next, the dentist will fill and seal the tooth so it’s closed off to infection. The tooth is filled with gutta-percha, a biocompatible filling material, combined with rubber cement. A temporary filling will be placed until you get a permanent crown.
In some cases, posts will be inserted inside the tooth during the filling process. I do not recommend posts to patients, as they have a tendency to crack the teeth.
Do root canals hurt? Root canals do not hurt at all during the procedure. If the dentist is skilled at delivering the local anesthesia, you won’t feel a thing. There may be minor pain and soreness as you recover.

Sometimes, a dentist will begin the root canal and things go wrong — this can be a good thing!
If your dentist gets inside the tooth and is presented with new information that changes the chances of success of a root canal, he will stop to tell you. This gives you the choice to abort the procedure before proceeding with a root canal with lower chances of success than you both originally thought.
Reasons to stop a root canal include:
- Separated instrument : An instrument breaks off inside the tooth.
- Calcified root canal: If the root canal is calcified, your dentist won’t be able to negotiate it well. In these cases, endodontic surgery like an apicoectomy may be required.
- Fracture: Once the tooth is opened, your dentist might see a fracture not visible on the x-ray. Seepage can occur at the fracture line, which can lead to bone loss. If you lose bone around the tooth, you lose the support of the tooth. In these cases, an extraction with a dental implant will offer a much better prognosis.
- Curved root: Also called “complex canal morphology,” this kind of tooth root is hard to navigate. Complex root canal anatomy — lots of hard-to-navigate twists and turns — reduce the potential success rate.
Your dentist should only do the root canal if conditions are ideal.
You can still drive home if you’ve been given only local anesthesia.
After your root canal treatment is complete, you’ll need to go back to your dentist for a crown or a filling. Crowns or fillings should be placed within 1-4 weeks after a root canal.
Do you need a crown after a root canal? If you have a root canal done on a molar or pre-molar (your back chewing teeth), you need a crown after root canal treatment. Most incisors and canines (front teeth) do not require a crown.
Some people wait to get a crown so that they don’t max out their insurance, but this can be a dangerous risk. If the tooth fractures before a crown is placed, you lose the investment of the root canal entirely.
In some cases, your dentist will recommend only a filling to protect the tooth.
Crowns benefit teeth in the following ways:
- Better success rate: Your root canal treatment is more likely to last without repeated treatment if a crown is placed on a molar or premolar. Root canal without crown is 6 times more likely to fail, according to one study over an 11-year period. Another study found that a root canaled tooth without a crown has a 63% chance of failure within 5 years.
- Reduced chance of fracture: Without a dental crown, your tooth may become more susceptible to fracture over time. This is because the “mummified” tooth will become brittle as it no longer receives blood flow.
- Natural-looking tooth: You can get a crown to match the color of your remaining teeth to hide discoloration and appear just like a natural tooth.
- Lower risk of infection: A crown covers the inside of the treated tooth to prevent most bacteria from getting in, which could otherwise cause a new infection and require retreatment.
The procedure for placing a crown is done in these steps:
- The tooth is filed down to remove the outer layer.
- Impressions are taken of the new tooth shape. For in-office crowns, your dentist will take an optical impression.
- The impressions are sent to a lab or used to create a crown in-office.
- If your dentist doesn’t have the equipment to make a same-day crown, a temporary crown will be placed and you’ll wait several days while the crown is being manufactured.
- The crown is placed on your tooth and secured by mechanical retention. Dental cement is used to prevent saliva or any other substance from getting under the crown.
Antibiotics have been part of the standard of care for root canals for many decades. However, more recent research shows they are frequently unneeded and may contribute to antibiotic resistance .
Dentists frequently prescribe antibiotics before and after endodontic treatment for reduced chance of systemic infection, reduced pain, increased success rates, and a variety of other reasons.
The problem is that antibiotics actually have no significant impact on root canal outcomes in almost any case.
One review of antibiotic use for root canals found that dentists are most likely to prescribe antibiotics for root canals due to the placebo effect and a lack of education, not a clinical need.
A 2016 review by the American Dental Association (ADA) found that the only legitimate reasons for antibiotics before or after a root canal were a present systemic infection, fever, or both.
The European Society of Endodontology holds the position that antibiotics should be prescribed only in the following cases:
- Systemic infection caused by a tooth abscess
- Tooth abscess in an immune-compromised patient
- Rapid onset infection with outward symptoms in 24 hours or fewer
- Replantation of a tooth that has been knocked out (avulsed) due to trauma
- Trauma to the soft tissue of the mouth that requires treatment
Once your dentist has diagnosed irreversible pulpitis, you need to get a root canal (or alternative treatment) right away. Your provider may prescribe antibiotics before treatment, in which case you may need to wait to finish your round of antibiotics.
When you find out you need a root canal for irreversible pulpitis, it’s like a ticking time bomb because the infection will eventually get out of control.
Pressure, swelling, and pain are likely to get worse. You might develop a bad taste in your mouth or experience numbness. The infection could spread to more vulnerable tissues, like your heart.
Yes, a tooth infection can kill you.
In the 1600s, tooth infections made the list of the top 6 causes of death in England. As recently as 1908, tooth infections had a mortality rate of up to 40%. That’s worse than smallpox!
Complications of infections like these, such as those from a tooth abscess, are extremely dangerous. Don’t wait for treatment!
For fast root canal recovery:
- Don’t smoke for at least 7 days after the procedure
- Avoid chewing hard, crunchy, very hot, or very spicy foods/drinks or any foods with a sharp edge (like sourdough bread) for 1-2 days
- Avoid drinking alcohol for 1-2 days, as this may increase bleeding
- Don’t bite or chew on the treated tooth until a permanent crown has been placed
- Brush, floss, and maintain good oral hygiene as normal
Can you drive after a root canal? You should be able to drive immediately after a root canal procedure unless sedation was used. Root canals usually involve local anesthetic, but sedation may be requested for patients who are anxious about the procedure.
You should have a follow-up exam 6 months after your root canal. After that first follow-up, your dentist should closely examine (and, preferably, do a CBCT on) your treated tooth every 3-5 years to check for a failed root canal and reinfection.
It’s common to have a little soreness after your procedure, but extreme pain after a root canal is abnormal. One study estimates that long-term pain happens after only 12% of root canal treatments .
If you do have pain, it usually peaks 17-24 hours after the procedure. To avoid this, keep your head elevated with a wedge pillow while sleeping for the first 1-2 nights.
Soreness from keeping your mouth open for a long period of time should go away after 1-2 days. However, if you have persistent TMJ pain, this soreness and stiffness may remain for 6-8 weeks, particularly if a dental dam was used.
You may have pain in the gum or other soft tissue around the root-canaled tooth from inflammation or damage during your root canal treatment. This should clear up within a week or two.
You can use over-the-counter pain medications like ibuprofen (Motrin) or acetaminophen (Tylenol) to relieve any pain for the day or two after a procedure.
Persistent pain (3 months or more) after root canal usually happens when you bite down or palpate the treated tooth. It’s frequently associated with:
- A filling that is too high
- A severe infection before your root canal
- Previous painful dental work
- Existing chronic pain issues
More women than men tend to develop long-term root canal pain.
If you experience severe or sudden pain in the tooth weeks, months, or years after your root canal, it may be a sign of root canal failure. Contact your dentist immediately.
Before dental insurance, a root canal procedure in the United States costs anywhere from $500-$2,250. A crown after root canal ranges from $600-$2,500, depending on the material.
When performed by a general dentist, a root canal for a front tooth will cost between $500-$1,000. Molars (back teeth) cost between $1,000-$1,500 with a general dentist. Endodontists (root canal specialists) usually charge about 50% more for a root canal procedure.
A high-quality cubic zirconia (new porcelain) crown costs around $1,300, while a gold crown — which lasts longer than any other material — runs about $2,500.
Your total cost may be as little as $1,100 and as much as $4,750 for a single root canal and crown.
The cost of your treatment will also differ depending on where you live. In general, a higher cost of living will mean a higher cost for dental treatment.
How much are root canals with insurance? Root canals are almost always covered by dental insurance but the rate of coverage differs by plan. In addition, your coverage probably applies only after you’ve met your yearly deductible.
Many traditional plans cover root canals at 80% and crowns at 50% of the billed cost. However, check your insurance plan and talk to your insurance company before treatment to be sure.
And remember: Most dental plans cap yearly coverage amounts at $1,500 or less. You may be responsible for a higher percentage of the cost than you initially expect if your dental plan reaches its cap.
Are root canals worth the cost? Root canals are often worth the cost because they have a high success rate and cost less than high-quality alternatives. The price tag for extraction with a dental implant, for instance, is significantly higher than a root canal and crown (potentially 2-3 times more).
Potential complications of a root canal (not including those related to anesthesia) include:
- Reinfection: A cyst or bone infection can occur years after root canal treatment, most often from a badly done procedure. Underfilling and/or not properly disinfecting the canals, as well as the presence of a broken instrument, make this outcome more likely.
- Partial root filling: It’s possible for a dentist not to completely fill the tooth root(s) during a root canal procedure, particularly if you have a complex canal structure. This may require retreatment and should be done by an endodontist.
- Canal or tooth crown perforation: If a dentist perforates (creates a hole) in the root canals or in the crown of your tooth, you’ll probably need to have the tooth extracted.
- Instrument breakage: During 2.7-3.7% of root canals , an instrument breaks during treatment. Your dental provider should inform you if this occurs and let you choose whether or not to have them remove the broken piece. Even if the piece remains, this may or may not impact the success of your root canal treatment.
- Overfilling the canal: If the canals were overfilled and the tooth is near the sinus cavity or nerve canal, this may cause post-operative pain. The pain may subside without further treatment. However, the excess filling material may need to be removed if it causes bone inflammation or significant pain, or is near the mandibular nerve or maxillary sinus.
- Discoloration: Darkening tooth color is usually a sign of blood or a poorly done root canal. This complication can often be avoided by the use of a rubber dam, magnification device, and clean instruments.
- Sinus drainage: It’s possible to have drainage and sinus pain after a root canal. You may notice it tastes or smells like the antibacterial solution used to disinfect your tooth during the procedure. Most likely, this occurs if the space left behind after a large abscess allowed passage of the solution into your sinus cavity. This is probably not dangerous and should go away after a short period of time. However, if you experience sudden, severe pain or any facial swelling, contact your dentist right away.
The main concern of root canal therapy is that they are never 100% clean, meaning there is always bacteria left behind in the auxiliary canals off the main root canals.
This is true for every single root canal procedure, but the quality of treatment has a major impact on this. As a study in the Journal of the American Dental Association puts it :
“Endodontic procedural errors are not the direct cause of treatment failure; rather, the presence of pathogens in the incompletely treated or untreated root canal system is the primary cause of periradicular pathosis.”
In other words, a badly done root canal is far more likely to fail and cause problems in the future.
I recommend all patients get a cone-beam CT (CBCT) every 3-5 years after root canal therapy to properly check for lesions or other signs of root canal failure. CBCT is a far more reliable method to recognize failure than a traditional x-ray.
Lesions and reinfection can occur with or without pain, so don’t rely on symptoms to determine whether or not your root canal was successful.
Root canal success rate and long-term prognosis are remarkably high, particularly when a crown is placed on the treated tooth.
The overall success rate for root canal procedures is between 80.1%-86%.
The success rate decreases most significantly (below 90%) after 5 years have passed.
A patented same-day root canal treatment known as the GentleWave System boasts a success rate of 97.3% after 12 months. This is similar to the treatment outcomes of traditional root canal therapy. However, the GentleWave system does result in significantly fewer reports of postoperative pain than traditional root canals.
Factors that reduce the chance of root canal success include:
- Treatment by a general dentist, rather than an endodontist
- Necrotic pulp (dead tooth pulp) and/or irreversible pulpitis
- Periodontal (gum) disease
- Poor procedural technique (including underfilling, overfilling, or instrument breakage)
- Fracture to the treated tooth and/or crown
- New bacterial infection
- Male gender
- Hispanic/Latinx ethnicity
How long does a root canal last? On average, root canals last 10 years or more. Some root canals last a lifetime.
Root canals are safe for most people but may cause problems over time. To watch for root canal failure, get a cone-beam CT (CBCT) every 3-5 years after endodontic treatment to check for failure.
Major organizations, like the American Dental Association (ADA) and American Association of Endodontists (AAE), speak highly of the benefits of root canals. According to both the ADA and AAE, root canals pose no major danger whatsoever.
Other groups, including the International Association of Biological Dental Medicine (IABDM), do not recommend root canal therapy.
The Root Cause documentary and some alternative dental practitioners present root canals as extremely dangerous. Their theories often cite root canal treatment as a hidden cause of any number of systemic, chronic diseases.
To date, no published, peer-reviewed scientific evidence supports the majority of these hypotheses.
However, if you are at a high risk of root canal failure due to compromised immunity or other factors, you may want to opt for an alternative treatment.
Is a root canal right for you? If your dentist has identified irreversible pulpitis, a root canal is one of only a few options for treatment.
Many dentists will recommend root canal for cases of reversible pulpitis for a number of reasons. In these situations, I would ask about getting a large filling instead.
Consider the pros and cons before deciding if a root canal is the best option for your case.
Root Canal Pros:
- You don’t have to extract the tooth.
- You don’t lose the bone around the tooth.
- Your orthodontic growth, bite, and normal tooth use will remain the same.
- You will no longer experience hot or cold sensitivity in the treated tooth.
- The recovery pain and recovery time are mild and brief.
- The rate of success is very high even after 10 years (over 80%).
- It’s less expensive than extraction with an implant.
Root Canal Cons:
- There’s no such thing as a 100% clean root canal — some bacteria will always be left behind.
- If your root canal fails, you’ll need retreatment of some kind, which carries a significant additional cost.
- There are anecdotal reports that root canals are associated with systemic disease months to years after treatment. If you’re a healthy person, this is likely not an issue. But if you’re on the edge of optimal health, it’s possible your body can’t handle it. If you’re immunosuppressed or in poor health, you may want to consider other options.
- It can be hard to sit with your mouth open for a few hours during the procedure, particularly if you struggle with TMJ pain.
If possible, ask a trusted friend or family member to help with your decision if you’re already in significant pain. “Deciding under the influence,” as I call it, can lead to hasty decisions — especially if your tooth hurts a great deal.
Preventing the need for root canal therapy involves reducing your risk of untreated tooth decay and trauma to your teeth.
To reduce your risk of tooth decay:
- Practice good oral hygiene ( flossing , brushing, oil pulling , etc.)
- Use a remineralizing toothpaste like Boka or RiseWell
- Eat foods that prevent cavities
- Limit your intake of sugary, acidic, and highly processed foods
- Avoid antibacterial oral care products like regular mouthwash , which disrupt your oral microbiome
- Prevent dry mouth by mouth taping and practicing nose breathing
- See your dentist for a cleaning and exam every 6 months
To prevent tooth decay from progressing to the point of a root canal:
- Never ignore a toothache — always discuss new tooth pain with your dentist
- Don’t put off dental work for tooth decay unless you’re actively reversing cavities
- Consider regenerative endodontics , a stem cell endodontic therapy, if you have existing pulpitis
To reduce your risk of trauma to teeth:
- Always wear a mouthguard when playing sports or during athletic activity
- Use your teeth only for eating — no opening packages, chewing on pencils, etc.
- Be cautious in situations where falling is likely
- Practice safe driving — always wear a seatbelt
Root Canal Alternatives
There are risks to root canal therapy, which is one reason why many functional dentists may not frequently prescribe this dental treatment.
Depending on what kind of specialist you talk to, their recommendation for treatment may be different. Oral surgeons often prescribe an extraction with an implant, while an endodontist is more likely to recommend a root canal.
Depending on your case, there are 3 possible alternatives to root canal treatment:
- Dental fillings
- Extraction with dental restoration (implant, bridge, or dentures)
- Regenerative endodontics
For cavities that have not caused irreversible pulpitis, a large filling may be a better option than a root canal. A filling allows you to retain a living tooth, which will be more resistant to new cavities and fracture than an endodontically treated tooth.
Fillings are not an option once the tooth pulp has become irreversibly inflamed or died.
Why would a dentist recommend a root canal instead of a filling for a tooth with reversible pulpitis? Each practitioner has preferences for treatment protocols. Many dentists turn to root canal when a filling could work for a few basic reasons:
- Large fillings require great technique. Some providers aren’t confident in their ability to successfully complete this treatment, particularly if the top of the tooth must be made very thin to place the filling. This could potentially lead to the need for follow-up dental work.
- Irreversible pulpitis is difficult to diagnose. As explained, determining if a patient has reversible or irreversible pulpitis is not always straightforward. If a dentist is unsure, he or she may opt for the treatment most likely to be successful in either case — a root canal.
- Root canals cost more. The vast majority of dentists I know are excellent providers who care about their patients. However, a dental practice is a business, and it’s more profitable to bill for a root canal than a filling. Root canals are almost always covered by dental insurance, so there’s little chance that the insurance company will refuse to pay.
If you’re not confident in the prescription of a root canal and believe a filling would be better, consider getting a second opinion to be sure.
Tooth extraction followed by a restorative procedure is the only alternative option besides a root canal for irreversible pulpitis.
Restorations that can be done after an extraction include:
- Dental implant
- Dental bridge
A dental implant is the preferred option if you decide against a root canal, as it is less likely to lead to bone loss or gum problems than dentures. It’s a highly effective procedure and the implant allows for natural chewing and aesthetics.
Both a root canal and extraction with a dental implant have the same probability of long-term success. Dentists make treatment decisions in these cases based on factors like cost-benefit ratio, patient preference, systemic health issues, and the probability of root canal success.
After extraction of multiple side-by-side teeth, your dentist may suggest a bridge connected by implants on either side.
If you are missing a large number of teeth and are on a limited budget, you may opt for dentures instead of multiple dental implants and/or a bridge.
Regenerative endodontics is a relatively new method of endodontic treatment to restore inflamed dental pulp.
First introduced in 2004 , this practice involves irrigating and disinfecting root canals of a tooth with pulpitis but not removing the infected pulp. Then, the tooth is agitated to cause bleeding at the apex of the tooth roots.
This bleeding provides the inflamed pulp of the tooth with a large number of mesenchymal stem cells (MSCs) that may heal the root of the tooth. Other stem cells may be manually injected into the tooth root.
Regenerative endodontic therapy may be successful in 91% of cases at reversing pulpal inflammation. In some cases, treatment is effective even when the pulp has initially been diagnosed with irreversible pulpitis.
This may not be the best option for many people because:
- The field of regenerative endodontics is relatively new and untested
- The procedure itself requires an extensive amount of perfected technique
- It may not be easy to find a provider near you
- This procedure is less likely to be covered by dental insurance
- As a more experimental procedure, regenerative endodontics may be prohibitively expensive
However, this could be the future of what we currently know as root canal therapy.
Click here to browse clinical trials for regenerative endodontics.
What root canal irrigants are used to clear the pulp chambers and kill bacteria before the tooth is filled?
- Sodium hypochlorite (NaClO)
- Chlorhexidine
- Calcium hydroxide [Ca(OH)2]
Integrative endodontic treatment is partial to ozone treatment. More than any other bactericidal solution, ozone may effectively eliminate a significant amount of bacteria in the small canals off the main pulp chamber.
There is also no risk of antibiotic resistance with ozone , unlike other alternatives, which could lead to stronger bacterial strains. Ozone may also be used on its own or with other antimicrobial agents.
More recently, the use of antimicrobial photodynamic therapy (aPDT) has been studied as an adjunct (add-on) to these agents. aPDT can result in a significant reduction of bacteria within the pulp chamber.
What are my options for root canal sedation?
- Minimal sedation: Your dentist can use nitrous oxide to ease your fear. You may also be given a mild oral sedative about an hour before your procedure. You’ll be awake during treatment but mostly unconcerned with the sounds or sensations. The effects will wear off shortly after the procedure and you should still be able to drive home.
- Moderate sedation: Formerly dubbed “conscious sedation”, this kind of sedation can be achieved with higher doses of an oral sedative like Valium or through an IV. You may be groggy enough to sleep during the procedure but will be easy to wake up.
- Deep sedation/general anesthesia: Deep sedation puts you completely “to sleep” and you can’t be easily awakened. You will probably have no memory of the procedure or the period of time shortly after you wake up. This level of sedation requires an additional two-year certification for a dentist or the use of an in-house anesthesiologist. You’ll need someone to drive you home after undergoing deep sedation.
Can I eat before a root canal?
Do root canals cause cancer.
Scientific methodologies from the 1950s drove this theory. The science on this is correlative, not causative. Root canal methods and materials have evolved many times over since those times and have been completely different since the 1970s.
Will a root canal give me a blood infection (bacteremia)?
For context, bacteremia is very common after dental cleanings — it’s generally not something to cause great concern.
Why would my dentist not use a rubber dam for my root canal?
With a temporomandibular joint disorder (TMD), keeping your mouth open with a dental dam for up to 90 minutes during a root canal can cause significant discomfort. Some patients have TMJ pain for 6-8 weeks after the procedure.
Can I get a root canal while I’m pregnant?
The American Pregnancy Association emphasizes that, while root canals are considered safe while pregnant, it’s important to consider the risks of sedation, antibiotics, and x-rays that may be involved.
A single x-ray should not pose a risk to you or your baby. If possible, request a lower level of local anesthesia and skip other sedation. You should only take antibiotics if your dentist feels this is the only safe option, as antibiotics can affect fetal health. References
- Sigurdsson, A. (2003). Pulpal diagnosis. Endodontic Topics, 5 (1), 12-25. Abstract: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1601-1546.2003.00024.x
- Aaminabadi, N. A., Parto, M., Emamverdizadeh, P., Jamali, Z., & Shirazi, S. (2017). Pulp bleeding color is an indicator of clinical and histohematologic status of primary teeth. Clinical Oral Investigations, 21 (5), 1831-1841. Abstract: https://link.springer.com/article/10.1007/s00784-017-2098-y
- Wong, A. W. Y., Tsang, C. S. C., Zhang, S., Li, K. Y., Zhang, C., & Chu, C. H. (2015). Treatment outcomes of single-visit versus multiple-visit non-surgical endodontic therapy: a randomised clinical trial. BMC oral health, 1 5(1), 1-11. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4684923/
- Aquilino, S. A., & Caplan, D. J. (2002). Relationship between crown placement and the survival of endodontically treated teeth. The Journal of prosthetic dentistry, 87 (3), 256-263. Abstract: https://pubmed.ncbi.nlm.nih.gov/11941351/
- Nagasiri, R., & Chitmongkolsuk, S. (2005). Long-term survival of endodontically treated molars without crown coverage: a retrospective cohort study. The Journal of prosthetic dentistry, 93 (2), 164-170. Abstract: https://pubmed.ncbi.nlm.nih.gov/15674228/
- Kishen, A. (2006). Mechanisms and risk factors for fracture predilection in endodontically treated teeth. Endodontic topics, 13 (1), 57-83. Abstract: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1601-1546.2006.00201.x
- Ventola, C. L. (2015). The antibiotic resistance crisis: part 1: causes and threats. Pharmacy and therapeutics, 40 (4), 277. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4378521/
- Bansal, R., Jain, A., Goyal, M., Singh, T., Sood, H., & Malviya, H. S. (2019). Antibiotic abuse during endodontic treatment: A contributing factor to antibiotic resistance. Journal of Family Medicine and Primary Care, 8 (11), 3518. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6881914/
- Aminoshariae, A., & Kulild, J. C. (2016). Evidence-based recommendations for antibiotic usage to treat endodontic infections and pain: A systematic review of randomized controlled trials. The Journal of the American Dental Association, 147 (3), 186-191. Abstract: https://pubmed.ncbi.nlm.nih.gov/26724957/
- Gould, K., & Hakan, B. European Society of Endodontology position statement: the use of antibiotics in endodontics. Full text: https://onlinelibrary.wiley.com/doi/full/10.1111/iej.12781
- Erazo, D., & Whetstone, D. R. (2019). Dental Infections . Full text: https://www.ncbi.nlm.nih.gov/books/NBK542165/
- Polycarpou, N., Ng, Y. L., Canavan, D., Moles, D. R., & Gulabivala, K. (2005). Prevalence of persistent pain after endodontic treatment and factors affecting its occurrence in cases with complete radiographic healing. International endodontic journal, 38 (3), 169-178. Abstract: https://pubmed.ncbi.nlm.nih.gov/15743420/
- Vieira, A. R., Siqueira Jr, J. F., Ricucci, D., & Lopes, W. S. (2012). Dentinal tubule infection as the cause of recurrent disease and late endodontic treatment failure: a case report. Journal of endodontics, 38 (2), 250-254. Abstract: https://pubmed.ncbi.nlm.nih.gov/22244647/
- Simon, S., Machtou, P., Tomson, P., Adams, N., & Lumley, P. (2008). Influence of fractured instruments on the success rate of endodontic treatment. Dental update, 35 (3), 172-179. Full text: https://www.researchgate.net/profile/Phillip_Tomson/publication/5344158_Influence_of_Fractured_Instruments_on_the_Success_Rate_of_Endodontic_Treatment/links/0912f50eae53de6861000000/Influence-of-Fractured-Instruments-on-the-Success-Rate-of-Endodontic-Treatment.pdf
- Cheung, G. S. (2007). Instrument fracture: mechanisms, removal of fragments, and clinical outcomes. Endodontic Topics, 16 (1), 1-26. Abstract: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1601-1546.2009.00239.x
- Lin, L. M., Rosenberg, P. A., & Lin, J. (2005). Do procedural errors cause endodontic treatment failure?. The Journal of the American Dental Association, 136 (2), 187-193. Abstract: https://jada.ada.org/article/S0002-8177(14)64408-1/abstract
- Bernstein, S. D., Matthews, A. G., Curro, F. A., Thompson, V. P., Craig, R. G., Horowitz, A. J., … & Collie, D. (2012). Outcomes of endodontic therapy in general practice: a study by the Practitioners Engaged in Applied Research and Learning Network. The Journal of the American Dental Association, 143 (5), 478-487. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4394182/
- Burry, J. C., Stover, S., Eichmiller, F., & Bhagavatula, P. (2016). Outcomes of primary endodontic therapy provided by endodontic specialists compared with other providers. Journal of Endodontics, 42 (5), 702-705. Abstract: https://pubmed.ncbi.nlm.nih.gov/27004720/
- Sigurdsson, A., Garland, R. W., Le, K. T., & Woo, S. M. (2016). 12-month healing rates after endodontic therapy using the novel GentleWave system: a prospective multicenter clinical study. Journal of endodontics, 42 (7), 1040-1048. Abstract: https://nyuscholars.nyu.edu/en/publications/12-month-healing-rates-after-endodontic-therapy-using-the-novel-g
- Touré, B., Faye, B., Kane, A. W., Lo, C. M., Niang, B., & Boucher, Y. (2011). Analysis of reasons for extraction of endodontically treated teeth: a prospective study. Journal of endodontics, 37(11), 1512-1515. Abstract: https://pubmed.ncbi.nlm.nih.gov/22000453/
- Iqbal, M. K., & Kim, S. (2008). A review of factors influencing treatment planning decisions of single-tooth implants versus preserving natural teeth with nonsurgical endodontic therapy. Journal of endodontics, 34 (5), 519-529. Abstract: https://pubmed.ncbi.nlm.nih.gov/18436028/
- Banchs, F., & Trope, M. (2004). Revascularization of immature permanent teeth with apical periodontitis: new treatment protocol?. Journal of endodontics, 30 (4), 196-200. Abstract: https://pubmed.ncbi.nlm.nih.gov/15085044/
- Nakashima, M., Iohara, K., Murakami, M., Nakamura, H., Sato, Y., Ariji, Y., & Matsushita, K. (2017). Pulp regeneration by transplantation of dental pulp stem cells in pulpitis: a pilot clinical study. Stem cell research & therapy, 8 (1), 61. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5345141/
- Kim, S. G., Malek, M., Sigurdsson, A., Lin, L. M., & Kahler, B. (2018). Regenerative endodontics: a comprehensive review. International endodontic journal, 51 (12), 1367-1388. Full text: https://onlinelibrary.wiley.com/doi/pdf/10.1111/iej.12954
- Lin, L. M., & Kahler, B. (2017). A review of regenerative endodontics: current protocols and future directions. Journal of Istanbul University Faculty of Dentistry, 51 (3 Suppl 1), S41. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5750827/
- Rahimi, S., Janani, M., Lotfi, M., Shahi, S., Aghbali, A., Pakdel, M. V., … & Ghasemi, N. (2014). A review of antibacterial agents in endodontic treatment. Iranian endodontic journal, 9 (3), 161. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4099945/
- Domb, W. C. (2014). Ozone therapy in dentistry: a brief review for physicians. Interventional Neuroradiology, 20 (5), 632-636. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4243235/
- Ajeti, N. N., Pustina-Krasniqi, T., & Apostolska, S. (2018). The effect of gaseous ozone in infected root canal. Open access Macedonian journal of medical sciences, 6 (2), 389. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5839455/
- Chiniforush, N., Pourhajibagher, M., Shahabi, S., Kosarieh, E., & Bahador, A. (2016). Can antimicrobial photodynamic therapy (aPDT) enhance the endodontic treatment?. Journal of lasers in medical sciences, 7 (2), 76. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4909016/
- Debelian, G. J., Olsen, I., & Tronstad, L. (1995). Bacteremia in conjunction with endodontic therapy. Dental Traumatology, 11 (3), 142-149. Abstract: https://pubmed.ncbi.nlm.nih.gov/7641631/
- Brincat, M., Savarrio, L., & Saunders, W. (2006). Endodontics and infective endocarditis–is antimicrobial chemoprophylaxis required?. International Endodontic Journal, 39 (9), 671-682. Abstract: https://pubmed.ncbi.nlm.nih.gov/16916356/
- Sahebi, S., Moazami, F., Afsa, M., & Zade, M. R. N. (2010). Effect of lengthy root canal therapy sessions on temporomandibular joint and masticatory muscles. Journal of dental research, dental clinics, dental prospects, 4 (3), 95. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3429977/
- Michalowicz, B. S., DiAngelis, A. J., Novak, M. J., Buchanan, W., Papapanou, P. N., Mitchell, D. A., … & Matseoane, S. (2008). Examining the safety of dental treatment in pregnant women. The Journal of the American Dental Association, 139 (6), 685-695. Abstract: https://pubmed.ncbi.nlm.nih.gov/18519992/
About Mark Burhenne, DDS
I’m on a mission to empower people everywhere with the same evidence-based, easy-to-understand dental health advice that my patients get. You can read my story here. I have been a dentist in private practice for 35 years. I graduated from the Dugoni School of Dentistry in San Francisco, CA in 1987 and am a member of the American Academy of Dental Sleep Medicine (AADSM), Academy of General Dentistry (Chicago, IL), American Academy for Oral Systemic Health (AAOSH), and Dental Board of California.

Dr. Mark is the author of the best-selling book 8-Hour Sleep Paradox
153 Stevens Ave # 1
Mt Vernon, NY 10550
Call (914) 668-1722
WE WELCOME NEW PATIENTS,
EMERGENCIES, AND SECOND OPINIONS

We Welcome New Patients, Emergencies, and Second Opinions
Early morning, late evening, and weekend appointments available, the do's and don'ts of root canal aftercare, it's very important to follow the proper proceduresfor root canal aftercare to ensure the best results. read on to learn aboutroot canal after care..

How to Prepare and What to Expect From Dental Veneers Before and After

How to Avoid Root Canal Treatment: 9 Tips for Patients

How Long Does a Dental Bridge Last?

What to Expect During an Emergency Dentist Visit: A Step-by-Step Guide

Breaking Down the Problem: Why Teeth Chip and How to Stop It
Teeth Whitening Results: What Can You Expect After Treatment?

Invisalign or Braces: Which Option Is Best for You?

Benefits of Regular Checkups at a Dentist in Mount Vernon, NY

How to Fix My Teeth: Am I a Good Candidate for Cosmetic Dentistry?

What Are the Benefits of Visiting a Cosmetic Dentist?
For our new patients.
Are you a new patient at Sparkle Dental? Make sure you fill out our new patient forms. Make sure that you print out and complete these forms before your first appointment. This will help us to speed up the new patient registration process.
Website designed and maintained by Xpress, INC
All Rights Reserved | Sparkle Dental
914-306-8795
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What to Expect During a Root Canal
Root Canal Treatments
A root canal is a dental procedure to fix a tooth that cannot be filled or restored any other way. If the tooth is severely decayed into the nerve of the tooth and / or abscessed, root canal treatment is usually the only option to save the tooth. Your regular dentist might do the root canal, but he / she may send you to an endodontist .
What's Involved in a Root Canal?
After the dentist numbs your tooth, he / she may use a rubber dam to keep the tooth area dry and free of saliva. A rubber dam is simply a piece of rubber that fits over the tooth and isolates it from the rest of the mouth. The dentist will then prepare the tooth by drilling an opening. After the dentist removes all of the decay and bacteria, he / she will use root canal files to clean out the canals (roots) of the tooth. Root canal files are small instruments that increase in diameter and fit down into the canals enabling the dentist to remove the nerve. Some dentists like to wait a week or two before they finish a root canal, to make sure that there is no discomfort or further infection. If this is the case, the dentist will thoroughly clean the tooth and usually, put some soothing medicine inside and seal it closed with a temporary filling material.
At the final stage of a root canal treatment, the dentist will usually fill the canals with a rubber filling material called gutta percha. After the canals are filled, a regular filling will be placed in the tooth.
Facts to Consider About Root Canals
After a tooth has had a root canal, it can become dry and brittle and easy to break. A crown (cap) is usually recommended to restore the tooth properly. The cost of a root canal on a molar (back tooth) generally costs between $1,000 and $1,300, but can run higher. A crown averages around $1000. Although the cost of a root canal is extensive, the only other alternative to a root canal is the removal of the tooth. If the tooth is removed, a bridge, partial or dental implant is recommended to fill in the gap because the other teeth can become crooked by shifting around.
Root Canals have a very high success rate, but there is always the chance of a new infection, which could require another root canal or removal of the tooth.
A root canal doesn’t have to be scary if you know what to expect. Express any concerns or questions you might have with your dentist and be sure to keep up with regular check up appointments because a root canal is an investment that should be protected.
American Association of Endodontists. Root Canal Explained .
CostHelper. How Much Does a Root Canal Cost?
Elemam RF, Pretty I. Comparison of the success rate of endodontic treatment and implant treatment . ISRN Dent. 2011;2011:640509. doi:10.5402/2011/640509
By Tammy Davenport Tammy Davenport is a dental assistant with experience on the clinical and administrative side.
How Long Does It Take To Recover After A Root Canal Treatment?

Undergoing a root canal treatment can be a daunting prospect for many. It’s often associated with myths of excruciating pain and lengthy recoveries. However, the reality is quite different. Root canals are a standard dental procedure to save a tooth that is severely infected or damaged, and they can provide much-needed relief from pain. But how long does it take to recover after a root canal? This comprehensive guide will explore the ins and outs of root canal recovery. From the immediate post-procedure period to long-term care, we’ll provide you with the essential information to fully understand the recovery process. Let’s dispel the myths and uncover the facts about recovering after a root canal treatment.
The Root Canal Treatment
A root canal procedure, also known as endodontic therapy, is a dental treatment aimed at saving a tooth that is severely infected, damaged, or has extensive decay. It involves a series of steps to address issues within the tooth’s pulp chamber, which contains nerves, blood vessels, and connective tissue. During the procedure, the dentist carefully removes the infected or damaged pulp, cleans and disinfects the interior of the tooth, and then seals it to prevent further infection. This process alleviates pain and discomfort associated with the infected tooth and allows it to remain in place, function properly, and serve its purpose in the mouth. Root canals are a common and highly effective dental procedure that can save teeth that might otherwise require extraction.
The procedure for a root canal goes as follows:
- Diagnosis and X-rays : The first step in a root canal procedure is a thorough examination by the dentist. They will assess the tooth’s condition and symptoms and review X-rays to determine the extent of the damage and the need for a root canal.
- Local Anesthesia : To ensure a painless procedure, the dentist will administer local anesthesia to numb the affected tooth and the surrounding area.
- Tooth Isolation : The dentist will place a rubber dam around the tooth to keep it dry and free from saliva during the procedure, maintaining a sterile environment.
- Access Opening : Using specialized instruments, the dentist creates a small access opening in the tooth’s crown to reach the pulp chamber and root canals.
- Cleaning and Shaping : The infected or damaged pulp is carefully removed from the pulp chamber and root canals. The tooth’s interior is then cleaned, disinfected, and shaped to prepare for filling.
- Filling and Sealing : Once cleaned and shaped, the tooth’s interior is filled with a biocompatible material called gutta-percha. The access opening is sealed with a dental restoration, such as a filling or crown, to restore the tooth’s function and appearance.
- Follow-Up : After the root canal, the patient may require follow-up appointments to monitor the tooth’s healing and ensure it remains free from infection. In some cases, a crown may be placed to strengthen and protect the treated tooth.
Source: UIC College of Dentistry
Causes Of A Damaged Root Canal
- Dental Decay : One of the primary causes of a damaged root canal is dental decay, commonly known as a cavity. When tooth decay is left untreated, it can progress deep into the tooth, reaching the pulp chamber. This can lead to infection, inflammation, and damage to the pulp, necessitating a root canal procedure to save the tooth.
- Trauma or Injury : Accidents, falls, or sports-related injuries can result in trauma to the teeth. When a tooth experiences a significant impact, it may cause damage to the pulp, leading to infection and the need for a root canal. Even if the damage is not immediately apparent, it can become symptomatic.
- Deep Dental Fillings : Deep dental fillings placed close to the pulp chamber can sometimes irritate the pulp, causing inflammation and damage. This can occur if the filling is too large or if it begins to leak over time, allowing bacteria to enter the pulp.
- Cracks or Fractures : Cracks or fractures in a tooth can create pathways for bacteria to enter the pulp and cause infection. These cracks can result from various factors, including chewing on hard objects, grinding teeth, or even age-related wear and tear.
- Repeated Dental Procedures : Teeth that have undergone multiple dental procedures, such as multiple fillings or crowns, may become weakened and more susceptible to pulp damage. The cumulative effects of these procedures can compromise the tooth’s integrity and lead to the need for a root canal.
Stages Of Healing From A Root Canal Procedure
Immediate post-procedure period.
- Discomfort and Pain Management
After a root canal, it’s common to experience some discomfort or mild pain. This is usually manageable with over-the-counter pain medications like ibuprofen or acetaminophen. Your dentist may also prescribe pain relievers if necessary. It’s essential to follow your dentist’s instructions regarding medication for pain management.
- Avoid Chewing on the Treated Tooth
To minimize the risk of complications and discomfort, avoiding chewing on the tooth that underwent the root canal treatment is advisable. Stick to a soft diet for a few days, and gradually reintroduce harder foods as your dentist recommends.
- Temporary Filling
In most cases, a temporary filling is placed in the tooth to seal the access point. This filling is not as durable as a permanent restoration, so it’s crucial to follow your dentist’s advice regarding scheduling the placement of a permanent crown or filling.
- Oral Hygiene
Continue your regular oral hygiene routine, but be gentle around the treated tooth. Brush and floss as usual, but avoid vigorous brushing or flossing around the area. Your dentist may recommend a mild antiseptic mouthwash to maintain oral hygiene.
The First Few Days to Weeks
- Sensitivity and Healing
It’s common to experience some sensitivity in the days following a root canal. This sensitivity is usually a sign that your body is healing and should gradually subside. If it persists or worsens, consult your dentist.
- Follow-Up Appointments
Your dentist will schedule follow-up appointments to monitor your progress and assess the healing of the treated tooth. During these appointments, any necessary adjustments to the permanent restoration will be made.
Long-Term Recovery and Care
- Permanent Restoration
A crucial aspect of long-term recovery is the placement of a permanent crown or filling on the treated tooth. This restoration provides strength and protection to the tooth, allowing it to function like any other tooth in your mouth. Your dentist will schedule this procedure once the tooth has fully healed.
- Oral Hygiene and Maintenance
Maintaining excellent oral hygiene is essential for the long-term success of your root canal. Brush and floss regularly, and consider using fluoride toothpaste to strengthen the treated tooth. Routine dental check-ups are also crucial to monitor the health of the restored tooth and your overall oral health.
Recovering after a root canal treatment is a manageable process. Immediate discomfort is typically short-lived, and long-term recovery involves essential steps such as placing a permanent restoration and maintaining good oral hygiene . Following your dentist’s guidance and being mindful of your oral health can ensure a successful and comfortable recovery. Remember that a root canal is a valuable procedure to save a tooth and relieve pain. Don’t let misconceptions about root canal recovery deter you from seeking the dental care you need.
Q: How long does a typical root canal procedure take?
A: The duration of a root canal procedure can vary depending on several factors. These include the location of the tooth in your mouth, the complexity of the tooth’s root canal system, and the extent of infection or damage. A straightforward root canal may take approximately 90 minutes to two hours to complete. However, more complex cases may require multiple appointments to ensure thorough treatment. Your dentist will provide a more accurate estimate based on your situation.
Q: Is a root canal more painful than a tooth extraction?
A: No, a root canal is not more painful than a tooth extraction. In fact, root canals are specifically designed to relieve pain and discomfort caused by severe tooth infections or damage. During a root canal procedure, your dentist will administer local anesthesia to numb the affected tooth and the surrounding area. This ensures that you do not experience any pain during the treatment. After the procedure, it is common to experience some discomfort, but this is typically manageable with over-the-counter pain relievers like ibuprofen or acetaminophen. Tooth extractions can be more invasive and may result in more post-procedure pain and recovery time.

Q: How soon can I eat normally after a root canal?
A: You can usually resume eating soft foods shortly after a root canal procedure. However, it’s essential to avoid chewing on the treated tooth until it receives a permanent restoration. The immediate post-procedure period may involve some sensitivity or discomfort, so sticking to a soft diet for a few days is advisable. Your dentist will provide guidance on when it’s safe to reintroduce harder foods into your diet, which typically occurs after the placement of a permanent crown or filling, which can take a few weeks.
Q: Can I drive home after a root canal procedure?
A: In most cases, you can safely drive yourself home after a root canal procedure. The local anesthesia used during the treatment will not impair your ability to operate a vehicle. However, if your dentist prescribes stronger pain medication to manage post-procedure discomfort, it’s advisable to arrange for a ride home, as these medications can cause drowsiness or altered alertness.
Q: Will my tooth be as strong as before after a root canal?
A: Yes, with the placement of a permanent crown or filling, your tooth can be as strong as it was before the root canal procedure. The purpose of the crown or filling is to protect the treated tooth, restore its functionality, and ensure it can withstand the normal forces of biting and chewing. This restoration effectively reinforces the tooth’s structure, allowing it to function like any other tooth in your mouth.
Q: How long does the numbness from the anesthesia last after a root canal?
A: Numbness from local anesthesia typically lasts for a few hours after a root canal procedure. During this time, avoiding eating or drinking hot liquids is essential to prevent accidentally burning your mouth. Also, don’t bite your lip, cheek, or tongue while the numbness persists. Your ability to speak and eat will return to normal once the effects of the anesthesia wear off, usually within a few hours.
SUCCESS STORIES
Staples mill va, north side va, south side va.

Call us Now!
- STAPLES MILL (804)823-5500
- NORTH SIDE (804)264-4068
- South Side (804)335-0599
Book Online

Staples Mill Office
9195 Staples Mill Rd, Henrico, VA 23228
(804)823-5500
North Side Office
5007 Brook Rd, Richmond, VA 23227
(804)264-4068
South Side Office
9945 Hull Street Rd, Richmond, VA 23236
(804)335-0599
Chester Office
2480 Osborne Rd, Chester, VA 23831
(804) 621-0602
- Referral Form
- Staples Mill
- Search the site GO Please fill out this field.
- Newsletters
- Health Conditions A-Z
- Oral Health Conditions
What to Know About Root Canals
:max_bytes(150000):strip_icc():format(webp)/LauraSchober-LauraSchober-966c4fa3c0004a67b4fa525878316f7d.jpg)
- The Process
- Why You'd Need It
What to Expect Before and After
How long do root canal fillings last.
A root canal is a dental procedure performed on teeth that are severely damaged or infected. The procedure is necessary when the pulp, a mass of blood-supplying soft tissue inside the tooth, becomes infected or inflamed.
The purpose of a root canal is to clear out bacteria from inside the tooth, in spaces of the root known as canals, and prevent reinfection. With root canal, your natural tooth can be saved from removal.
More than 15 million root canals are performed each year in the U.S. The procedure is a relatively painless one, usually with successful results.
Design by Health
What Happens During a Root Canal?
A root canal takes one or two office visits to complete. Generally, each appointment takes approximately 90 minutes. A dentist or endodontist—a dental professional who specializes in problems inside the tooth—will perform the root canal. Here are the steps they will take during the first visit:
- A local anesthesia is applied to numb the tooth and the area around it so there is little to no pain during the procedure. Generally, the level of pain is similar to other dental procedures, such as getting a filling or wisdom tooth removed .
- An opening is made in the top of your tooth to expose the infected or inflamed tooth root.
- The nerve is removed from inside the tooth and the area of the root, or the root canal.
- The bacteria are removed from inside the tooth, and the inside of the tooth is disinfected.
- The root canal is filled with a rubber-like material to prevent reinfection.
- A temporary filling is placed on the tooth.
Because the filling you get at the end of your first appointment only a temporary protection, a follow-up appointment will be needed as soon as possible to place a permanent filling or crown. This is necessary to protect your tooth from additional damage and to prevent infections.
Why Would You Need a Root Canal?
If your tooth’s pulp—a soft mixture of nerves, blood vessels, and connective tissue inside the tooth—becomes infected or inflamed, a root canal is necessary to remove the bacteria that are causing the pain and damage to your natural tooth .
You may need a root canal if you’ve had any of the following dental problems:
- Cracked, fractured, or chipped tooth
- Injury to the tooth
- An infection in the root of the tooth (an abscess)
- Severe damage to your tooth
- A deep cavity
- Repeated dental procedures that disturb the pulp of your tooth
- A faulty crown
If an infected, inflamed, or injured tooth is left untreated, your tooth is at risk of having to be removed. Therefore, it is important to see a dentist or endodontist for diagnosis and treatment as soon as symptoms arise.
Signs You May Need a Root Canal
You may need a root canal if you experience any of the following symptoms:
- Prolonged sensitivity to hot or cold
- Darkening of the gums
- Tender or swollen gums
- Pimples on the gums
- Severe pain while chewing food
- Tooth decay
If you’re experiencing any of these symptoms, consult a dental professional for diagnosis and, if necessary, root canal treatment.
How a Root Canal Can Help
If root canal symptoms are ignored or left to linger for too long, the tissues around the root of your tooth can become infected. This causes swelling and pain, which could cause an abscess inside the tooth or in the bones around the end of the tooth’s root. If left untreated, you can lose the tooth or develop a severe infection.
In some cases, the infection in the tooth can spread to other parts of the body and become life-threatening. That’s why it’s important to see a dental professional promptly if you’re experiencing any of the signs and symptoms that signal a root canal treatment may be needed.
A root canal procedure is a safe and effective way to treat the tooth and remove the bacteria that cause the pain and swelling. A root canal helps maintain your natural smile and ensures proper oral health, which allows you to eat your favorite foods without pain or sensitivity.
A root canal treatment can improve chewing, ensure proper biting form and sensation, and improve the natural appearance of the tooth. The procedure can also protect your other teeth from excessive wear.
There are some steps you should take before and after your actual root canal treatment to ensure a successful procedure and recovery.
Preparing for Root Canal
To prepare for your root canal procedure, it is recommended to brush your teeth before your appointment.
Check with your oral healthcare provider if they want you to refrain from eating for any amount of time before your procedure. Usually you are allowed to eat up to one hour before the procedure.
What Happens After a Root Canal?
After a root canal procedure, most people are able to return to their daily routine the same day of treatment. While your mouth will be numb for two to four hours following treatment, it is safe to return to school or work afterward.
The provider may recommend waiting a few hours before eating, until the numbness wears off in your mouth. It is best to eat soft foods that require little chewing, such as eggs, yogurt, applesauce, and fish.
It is also recommended to avoid eating hard, rough, hot, or chewy foods in the area of the restored tooth, especially until the tooth is permanently filled or covered with a crown.
While the procedure itself is pretty painless, you might have some soreness in the tooth’s surrounding area for a few days after. An over-the-counter anti-inflammatory drug, such as Advil (ibuprofen), can help relieve discomfort. If you continue to feel any discomfort or sensitivity beyond that time period, speak to your dental professional, who can help recommend further options.
The provider may prescribe an antibiotic to prevent infection.
You will need to visit your dentist after the procedure for regular check-ups, including a follow-up to ensure the infection is gone. Usually, check-ups are recommended twice a year for adults.
After a root canal procedure, any pain you had felt in the tooth should be gone.
Root canal fillings can last the rest of your life if cared for properly.
Although you receive a temporary filling immediately after the root canal, you will have a follow-up appointment to receive a permanent filling or crown. Just like a normal filling, this will last with proper oral care.
To best care for your filling after a root canal, brush twice a day for two minutes with fluoride toothpaste, floss between your teeth once a day, and see your dentist regularly for check-ups.
Risks of a Root Canal
Generally, a root canal is a safe and painless procedure, but it does carry some risks of which to be mindful, including:
- Nerve damage
- Tooth fracture
- An infection in the root of your tooth
- Breaking of surgical tools inside the tooth’s root canal
- Cracked tooth
- Incomplete removal of bacteria
A Quick Review
A root canal is a safe and effective dental procedure performed on teeth that have infected or inflamed pulp. Pulp is the soft tissue inside a tooth that supplies blood to a tooth. A root canal treatment eliminates bacteria from the canals within a tooth, prevents further infection, and saves the natural tooth.
If the infected pulp of the tooth is left untreated, complications can arise that could lead to tooth loss. Therefore, it is important to be aware of symptoms that could indicate you need a root canal treatment, such as prolonged sensitivity to hot or cold and darkening of the gums. If a dentist or endodontist determines you need a root canal, the treatment typically takes two visits. Any pain from the infection or inflammation would go away, and the treatment could last for the rest of your life with proper care.
American Dental Association - MouthHealthy. Root canals .
Ghannam MG, Alameddine H, Bordoni B. Anatomy, head and neck, pulp (tooth) . In: StatPearls . StatPearls Publishing; 2023.
MedlinePlus. Root canal .
American Association of Endodontists. What is a root canal?
American Association of Endodontists. Root canal explained .
American Association of Endodontists. What’s the difference between a dentist and an endodontist?
Sanders JL, Houck RC. Dental abscess . In: StatPearls. StatPearls Publishing; 2023.
Related Articles
- (347) 708-8795
- (212) 880-2700

- Apicoectomy Procedure NYC
- Microscopic Endodontics & Dentistry In NYC

- Calcified Root Canal Treatment in NYC
- Pediatric Endodontist in NYC
- Root Canal Post-Treatment Care

- Cracked Teeth Treatment NYC
- Traumatic Tooth Injuries in Manhattan
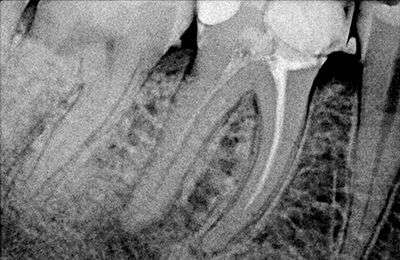
- Core Buildup Procedure After Root Canal
- Digital X-rays Of Teeth in NYC
- Gum Swelling Treatment After Root Canal
- Internal Tooth Bleaching NYC
- Patient Info
- Before/Afters
- Testimonials

Help for Before Root Canal Surgery
Posted on September 11, 2020

- How To Prepare For A Root Canal
- Do You Go Under For A Root Canal?
- Can A Root Canal And Crown Be Done In One Visit?
- Midtown Endodontist NYC
If you have a root canal surgery coming up, you may have questions about your procedure such as Can I eat before a root canal? and How do I prepare for a root canal? Use this guide to learn more, including what you should and should not do before a root canal.
How Do You Prepare for a Root Canal?
There are several ways to get ready for your procedure:
- Avoid any kind of alcohol or tobacco for at least 24 hours before the root canal to prepare your gums for the local anesthetic.
- Get a full night of sleep the evening before the procedure.
- Take an anti-inflammatory painkiller before you arrive at the endodontist’s office.
- Ask any questions about the procedure before it starts.
Can I Eat Before a Root Canal?
If you are wondering if you can eat before a root canal, yes, you can eat and drink several hours before a root canal. After the procedure , your mouth will stay numb and tender for several hours, so eating beforehand can save you from getting too hungry or thirsty after. Choose food that is gentle on your stomach and hydrate with water.
Do You Go Under for a Root Canal?
You can request unconscious sedation during your root canal. At Midtown Endodontist NYC , we can put you under for the procedure, so you do not have to stay awake as we clean out the roots of your tooth. If you are worried about the procedure, choosing to go under may make you feel more at ease. Unconscious sedation may be the right choice for someone who:
- Has a severe gag reflex.
- Does not like the sound of drilling on teeth.
- Has special needs.
Some people prefer conscious sedation as they want to know what is happening. The option you select could also depend on your comfort level with dental procedures.
Does Your Tooth Hurt Before a Root Canal?
Your tooth will probably hurt before a root canal.
Many patients experience sensitivity to heat and cold in their teeth when they need a root canal. You may also feel pain if you touch the tooth or use it to chew. Biting can be particularly painful as well. Tooth pain is often the first sign that indicates you may need a root canal.
Can a Root Canal and Crown Be Done in One Visit?
Most endodontists perform a root canal then you visit the dentist to receive your crown. In some cases, you can receive a root canal and crown in just one visit to the endodontist , eliminating the need for more endodontic appointments.
The office may use CEREC® (Chairside Economical Restoration of Esthetic Ceramics) technology to create a perfectly matching crown during your root canal procedure. It takes up to two hours to create a crown that looks like your teeth and naturally fits in your mouth. In fact, the CEREC® crown will fit into your mouth as though it has been there all along.
Book Appointment
Make an Appointment for Your Root Canal Today
The root canal procedure is simple and can be performed quickly. If you have experienced pain related to tooth decay, consider consulting with our endodontist to address the issue. Contact us today or book your appointment online . You can also give us a call at (347) 708-8795 .
You Might Also Like

When to See An Endodontist vs. An Oral Surgeon
November 02, 2022

How to Avoid Needing Root Canal Treatment
September 21, 2022

Failed Root Canal
April 19, 2022

- 212-880-2700
- Request Appointment
- Steven Lipner & Staff
- Treatment Consent Forms
- New Patient Forms
- Endodontist NYC
- Apicoectomy
- Microscopic Endodontics
- Root Canal in NYC
- Calcified Root Canal
- Emergency Root Canal
- Cracked Teeth
- Traumatic Injuries
- Root Canal Retreatment New York City
- Root Canal – Before & Afters

Returning to Work After Getting a Root Canal
by Our Endodontists Specialists | Oct 20, 2022 | Root Canal | 0 comments

Your experience after a root canal is usually relatively uneventful, but may be as unique as the circumstances that led to your need for the procedure. After your root canal, your endodontist will likely send you home with instructions for how to care for your teeth until a permanent crown can be placed. One of the most common post-procedural questions that may be at the top of your mind is returning to work after getting a root canal. The simple answer is usually, “the day after your procedure.” However, several factors can influence this time estimate. Read below to learn what the procedure involves and what to expect after the fact.
What to Expect During a Root Canal
First, your endodontist will numb the affected area with an anesthetic. After ensuring that you are numb and relaxed, your endodontist will begin the procedure by drilling a tiny hole in the top of the affected tooth. This hole will pass through the enamel and dentin layers to access the pulp chamber. Your endodontist will then use root canal files to remove infected tissue from the pulp chamber and root canals.
Your mouth will then be flushed with a microbial solution to remove any remaining bacteria. To replace the infected dental pulp, they will fill the chamber and canals with a rubber-like material called gutta-percha. The final step is to seal the tooth with dental cement and place a dental crown over the affected tooth to reduce the likelihood of bacteria re-entering the tooth.
Thankfully, with modern techniques and anesthetics, most patients report that they are comfortable during the procedure. For the first few days after treatment, your tooth may feel sensitive, especially if there was pain or infection before the procedure. This discomfort can be relieved with over-the-counter or prescription medications.
What to Expect After a Root Canal
Immediately after a root canal, your mouth may still feel numb. However, because the endodontist only uses a local numbing agent, you should be capable of driving and returning to work or school without major issues. However, you may feel some minor discomfort after this local anesthetic wears off.
Once the numbness wears off in a few hours, you can resume eating and drinking. However, be cautious about eating hard or extra chewy foods. Generally, you want to avoid biting on the treated tooth immediately after a root canal until you have your endodontist place a permanent crown on it. Until then, the treated tooth remains delicate and patients should follow basic oral care during this period of time.
Returning to Work After a Root Canal
As stated above, most root canals are relatively straightforward and easy to recuperate from in the course of the days following the procedure. There are three important factors to consider when questioning whether or not you’re prepared to return to work:
1. How Much Pain are you Experiencing?
You may experience discomfort after the root canal, but often it can be managed with over-the-counter painkillers. Serious pain can indicate that you may need to follow up with your endodontist.
2. Is Your Temporary Crown in Place?
If your temporary crown comes out for any reason, you need to contact your endodontist immediately to have it replaced. Keep in mind, you will also need to schedule your final appointment soon after to have the permanent crown installed.
3. Can you function with a sore or tender mouth at your job?
Does your line of work enable you to take it easy once a medical procedure has taken place? If not (if you can’t eat soft, cool foods or keep talking to a minimum), you might consider waiting a day or two to return to work.
As always, you should contact your endodontist if you experience the following symptoms post-procedure:
- Severe pain or pressure
- Visible swelling inside or outside your mouth
- An allergic reaction to medication (rash, hives or itching)
- Bite feels uneven
- The temporary crown or filling, if one was put in place, comes out
- Symptoms you experienced prior to treatment return
Our endodontists at Endodontic Specialists in Colorado Springs and Pueblo are wiling and ready to talk through a root canal procedure and all the implications it could have for you in returning to work after the fact. Give us a call today to learn more!
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Recent Posts
- Understanding Endodontic Treatments: How Long Do Root Canals Last?
- Understanding Interproximal Cavities and Their Treatments
- The Ultimate Dental Trauma Guide: More Than Just a Chipped Tooth
- Is Sedation Safer Than General Anesthesia?
- What is a Periodontist vs. an Endodontist?
Recent Comments
- Kim Bourgois on New Look, Same Great Advanced Endodontic Care

What is a Root Canal?
A root canal treatment is a dental procedure to remove inflamed or infected pulp on the inside of the tooth which is then carefully cleaned and disinfected, then filled and sealed. Root canal treatment is designed to eliminate bacteria from the infected root canal, prevent reinfection of the tooth and save the natural tooth.
What happens during root canal treatment? Learn more about this quick, comfortable procedure that can relieve your pain and save your natural tooth.
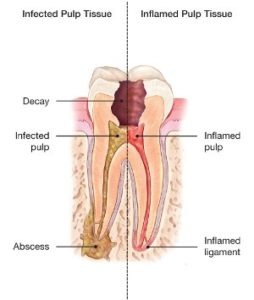
Inside your tooth, beneath the white enamel and a hard layer called dentin, is a soft tissue called pulp. This tissue contains blood vessels, nerves and connective tissue, which help grow the root of your tooth during its development. A fully developed tooth can survive without the pulp because the tooth continues to be nourished by the tissues surrounding it.
A modern root canal treatment is nothing like those old sayings! It's very similar to a routine filling and can usually be completed in one or two appointments, depending on the condition of your tooth and your personal circumstances. Getting a root canal is relatively painless and extremely effective. You'll be back to smiling, biting and chewing with ease in no time.
Saving the natural tooth with root canal treatment has many advantages:
- Efficient chewing
- Normal biting force and sensation
- Natural appearance
- Protects other teeth from excessive wear or strain
All About Root Canals
A root canal (also known as an endodontic treatment) is a serious procedure, but one that specialists handle every day. Before engaging in any type of dental work, it's important to know the facts about root canals.
Is a root canal painful?
Since patients are given anesthesia, a root canal isn't more painful than a regular dental procedure, such as a filling or getting a wisdom tooth removed. However, a root canal is generally a bit sore or numb after the procedure, and can even cause mild discomfort for a few days.
How do you know if you need a root canal?
Root canals are needed for a cracked tooth from injury or genetics , a deep cavity, or issues from a previous filling. Patients generally need a root canal when they notice their teeth are sensitive, particularly to hot and cold sensations.
There are a few symptoms that mean you might need a root canal-
- Severe pain while chewing or biting
- Pimples on the gums
- A chipped or cracked tooth
- Lingering sensitivity to hot or cold, even after the sensation has been removed
- Swollen or tender gums
- Deep decay or darkening of the gums
How long does it take to recover from a root canal?
Although you will most likely be numb for 2-4 hours following the procedure, most patients are able to return to school or work directly following a root canal. However, it is advised against eating until the numbness is completely gone.
How much does a root canal cost?
The cost varies depending on how complex the problem is and which tooth is affected. Molars are more difficult to treat; the fee is usually more. Most dental insurance policies provide some coverage for endodontic treatment.
Generally, endodontic treatment and restoration of the natural tooth are less expensive than the alternative of having the tooth extracted. An extracted tooth must be replaced with an implant or bridge to restore chewing function and prevent adjacent teeth from shifting. These procedures tend to cost more than endodontic treatment and appropriate restoration.
To learn more about what happens during root canal treatment, visit our Root Canals Explained page that walks your step-by-step through the procedure.
Recommended Educational Videos on Root Canal Treatment
Root canal treatment step by step.
Need a root canal? Don't be anxious. This informative video will walk you step-by-step through the procedure and explain how endodontists, the root canal specialists, can save your teeth.
Root Canal Safety
Concerned about the safety of root canal treatment? Watch this informative video to learn how endodontists perform millions of root canal treatments every year, safely, effectively and comfortably.
Visit the AAE YouTube Channel for more patient education videos to learn more about root canals and other endodontic procedures.
Visit the AAE YouTube Channel
How does endodontic treatment save the tooth?
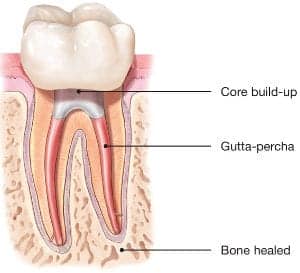
When you undergo a root canal or other endodontic treatment, the inflamed or infected pulp is removed and the inside of the tooth is carefully cleaned and disinfected, then filled and sealed with a rubber-like material called gutta-percha. Afterwards, the tooth is restored with a crown or filling for protection and will continue to function like any other tooth.
Endodontic treatment helps you maintain your natural smile, continue eating the foods you love and limits the need for ongoing dental work. With proper care, most teeth that have had root canal treatment can last a lifetime.
View endodontic treatment information in French, Japanese, Portuguese or Spanish.
FIND AN ENDODONTIST IN YOUR AREA
Overview - Root canal treatment
Root canal treatment (endodontics) is a dental procedure used to treat infection at the centre of a tooth.
Root canal treatment is not painful and can save a tooth that might otherwise have to be removed completely.
Why it's needed
The infection at the centre of a tooth (the root canal) is caused by bacteria that live in the mouth and invade the tooth.
This can happen after:
- tooth decay
- leaky fillings
- damage to teeth as a result of trauma, such as a fall
Tooth structure
A tooth is made up of 2 parts. The crown is the top part of the tooth that's visible in the mouth.
The root extends into the bone of the jaw, anchoring the tooth in position.
Teeth also consist of:
- enamel – the hard outer coating
- dentine – a softer material that supports the enamel and forms most of the tooth
- cementum – a hard material that coats the root's surface
- dental pulp – the soft tissue at the centre of the tooth
The root canal system contains the dental pulp and extends from the crown of the tooth to the end of the root.
A single tooth can have more than 1 root canal.
When root canal treatment is needed
Root canal treatment is needed when dental X-rays show that the pulp has been damaged by a bacterial infection.
The pulp may become inflamed if it's infected by bacteria, allowing the bacteria to multiply and spread.
The symptoms of a pulp infection include:
- pain when eating or drinking hot or cold food and drink
- pain when biting or chewing
- a loose tooth
As the infection progresses, these symptoms often disappear as the pulp dies.
Your tooth then appears to have healed, but the infection has in fact spread through the root canal system.
You eventually get further symptoms such as:
- pain when biting or chewing returning
- swelling of the gum near the affected tooth
- pus oozing from the affected tooth
- a swollen cheek or jaw
- the tooth becoming a darker colour
It's important to see your dentist if you develop toothache . If your tooth is infected, the pulp cannot heal by itself.
Leaving the infected tooth in your mouth may make it worse.
There may also be less chance of the root canal treatment working if the infection within your tooth becomes established.
Antibiotics , a medicine to treat bacterial infections, are not effective in treating root canal infections. They can though help to treat infection that spreads beyond the root and causes swelling.
How root canal treatment is done
To treat the infection in the root canal, the bacteria need to be removed.
This can be done by either:
- removing the bacteria from the root canal system (root canal treatment)
- removing the tooth (extraction)
But removing the tooth is not usually recommended as it's better to keep as many of your natural teeth as possible.
Before having root canal treatment, you'll usually be given a local anaesthetic .
This means the procedure should be painless and no more unpleasant than having a filling.
After the bacteria have been removed, the root canal is filled and the tooth sealed with a filling or crown.
In most cases the inflamed tissue near the tooth will heal naturally.
Root canal treatment is usually successful. In about 9 out of 10 cases a tooth can survive for up to 10 years after root canal treatment.
Find out how root canal treatment is done
Recovering from root canal treatment
It's important to look after your teeth when recovering from root canal treatment.
You should avoid biting on hard foods until your treatment is complete.
After your final treatment, your restored tooth should no longer be painful, although it may feel sore for a few days.
You can take over-the-counter painkillers, such as paracetamol or ibuprofen , to relieve any discomfort.
Return to your dentist if you still have pain or swelling after using painkillers.
In most cases it's possible to prevent the need for further root canal treatment by:
- keeping your teeth clean
- not eating too much sugary food
- giving up smoking if you smoke
Find out how to take care of your teeth and gums
Rate your dentist
You can comment on your NHS dentist and share your experience with others.
Find a dentist
Page last reviewed: 27 January 2022 Next review due: 27 January 2025

- [ May 4, 2024 ] WATCH: Brevard County Sheriff’s Office Releases ‘Join The Force’ Recruiting Video Brevard Crime News
- [ May 4, 2024 ] WATCH LIVE: Florida Tech Holds Commencement Ceremony for Spring 2024 Class Brevard News
- [ May 4, 2024 ] WATCH LIVE: UCF Holds Commencement Ceremony for Spring 2024 Class Brevard News
- [ May 4, 2024 ] ULA Atlas V to Launch Starliner Crew Flight Test from Cape Canaveral on Monday, May 6 Brevard News
- [ May 4, 2024 ] HOT OFF THE PRESS! Enjoy Space Coast Daily, Brevard County’s Best and Most Read Magazine Brevard Business News
Home » Home » Root Canal Treatment – Everything You Need to Know
Similar Stories
FEATURED STORIES
Click Here to Sign Up for Text Alerts
Or Signup Below For Email Alerts!

IMAGES
VIDEO
COMMENTS
1. Plan for Your Trip. Depending on how you travel, it's best to plan your departure date carefully. If sedation is used during your root canal, your endodontist will recommend you stay home and rest for at least 24 hours, especially if you're the one driving. You'll want the effects of the sedation to fully leave before taking off on ...
In short, yes, you can travel after getting a root canal. However, there are certain complications that may arise. For example, the changes in altitude while on an airplane can result in discomfort, sinus pain, and soreness. ... If you want to learn more about root canal aftercare or you'd like to schedule an appointment, don't hesitate to ...
Conclusion: It is generally safe to fly shortly after having a root canal provided your dentist has cleared you for air travel. However, it is important to consider all potential risks before making any decisions regarding air travel after the procedure. Additionally, following some simple tips (e.g., drinking plenty of water; avoiding alcohol ...
What can you do after a Root Canal treatment? Brush gently: Maintain oral hygiene by brushing your teeth gently after the root canal procedure. Use a soft-bristled toothbrush: Opt for a soft-bristled toothbrush to avoid irritation to the treated tooth and surrounding area. Follow your dentist's recommendations: Adhere to any specific post-treatment care instructions provided by your dentist ...
Root Canal Cost. Before dental insurance, a root canal procedure in the United States costs anywhere from $500-$2,250. A crown after root canal ranges from $600-$2,500, depending on the material. When performed by a general dentist, a root canal for a front tooth will cost between $500-$1,000.
A root canal removes the pulp from the tooth before it's sealed. It's actually a relatively painless procedure since local anesthesia will be used. You're more likely to work yourself up and suffer from anxiety than be in serious pain during the procedure. You'll be in and out of the office in about an hour and a half.
A root canal is treatment for infections in tooth pulp, the innermost layer of your teeth. Endodontists and dentists do about 15 million root canals in the United States every year. Typically, root canals are painless treatments. You can avoid needing a root canal by brushing your teeth after meals, flossing daily and having regular dental ...
Most root canals can be done in one to two appointments. The first appointment is the procedure itself when the infected pulp is removed. The second (and maybe third) appointment is when the root canal gets cleaned and filled with a crown or other filling to prevent infections. Each appointment lasts roughly 90 minutes each.
Myth 1: Root canal treatment is painful. That may have been the case decades ago, but with modern technology and anesthetics, you won't experience any more pain than if you went to have a cavity filled. The pain from a severe toothache, often caused by damaged tissues in the tooth, can be easily remedied when an endodontist removes the ...
Root Canal Recovery. After a root canal, your mouth will be numb for a couple of hours. Most people can go right back to work, school, or other activities.
Root Canals Explained. After a root canal, it's important to take special care of the affected tooth for a few weeks or until your tooth is fully restored by your endodontist or dentist recommends otherwise. You can brush and floss as usual, but make sure to be gentle around the treated area. Avoid chewing on hard foods or using the treated ...
These costs can vary according to where you live, whether you go to a specialist or a general dentist, and other factors. Root Canal Alternatives Saving your natural teeth is the best option, if ...
After these types of treatments, your body will need some time to rest and recover. Wait at least 48 hours before you hit the skies again. Tips for Traveling After Dental Work. If you tend to have teeth that are more on the sensitive side or you do not have a very high pain tolerance, traveling can be a bit uncomfortable. Here are a couple tips ...
Facts to Consider About Root Canals. After a tooth has had a root canal, it can become dry and brittle and easy to break. A crown (cap) is usually recommended to restore the tooth properly. The cost of a root canal on a molar (back tooth) generally costs between $1,000 and $1,300, but can run higher. A crown averages around $1000.
A: The duration of a root canal procedure can vary depending on several factors. These include the location of the tooth in your mouth, the complexity of the tooth's root canal system, and the extent of infection or damage. A straightforward root canal may take approximately 90 minutes to two hours to complete.
If a dentist or endodontist determines you need a root canal, the treatment typically takes two visits. Any pain from the infection or inflammation would go away, and the treatment could last for ...
Avoid any kind of alcohol or tobacco for at least 24 hours before the root canal to prepare your gums for the local anesthetic. Get a full night of sleep the evening before the procedure. Take an anti-inflammatory painkiller before you arrive at the endodontist's office. Ask any questions about the procedure before it starts.
Immediately after a root canal, your mouth may still feel numb. However, because the endodontist only uses a local numbing agent, you should be capable of driving and returning to work or school without major issues. However, you may feel some minor discomfort after this local anesthetic wears off. Once the numbness wears off in a few hours ...
A root canal treatment is a dental procedure to remove inflamed or infected pulp on the inside of the tooth which is then carefully cleaned and disinfected, then filled and sealed. Root canal treatment is designed to eliminate bacteria from the infected root canal, prevent reinfection of the tooth and save the natural tooth.
The root canal system contains the dental pulp and extends from the crown of the tooth to the end of the root. A single tooth can have more than 1 root canal. When root canal treatment is needed. Root canal treatment is needed when dental X-rays show that the pulp has been damaged by a bacterial infection.
Root canal treatment often has an unpleasant connotation, but the truth іs іt can actually be a straightforward and pain-free process. Your tooth's pulp consists оf blood vessels, nerves, and ...
The aftermath of the root canal can affect your activities for a couple of days, make it difficult to eat, and requiring pain medication. People who've needed a root canal say it's worse than ...