- Patient Care & Health Information
- Tests & Procedures
A pacemaker is a small, battery-powered device that prevents the heart from beating too slowly. You need surgery to get a pacemaker. The device is placed under the skin near the collarbone.
A pacemaker also is called a cardiac pacing device.
There are different types of pacemakers.
- Single chamber pacemaker. This type usually sends electrical signals to the lower right chamber of the heart.
- Dual chamber pacemaker. This type sends electrical signals to the upper and lower right heart chambers.
- Biventricular pacemaker. This type also is called a cardiac resynchronization pacemaker. It's for people who have heart failure and a slow heartbeat. The device stimulates both lower heart chambers. It helps make the heart muscle stronger.

Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- Cardiac resynchronization therapy
Why it's done
A pacemaker is used to control or increase the heartbeat. It stimulates the heart as needed to keep it beating regularly.
The heart's electrical system typically controls the heartbeat. Electrical signals, called impulses, move through the heart chambers. They tell the heart when to beat.
Changes in heart signaling may happen if the heart muscle is damaged. Heart signaling problems also may be caused by changes in genes before birth or by using certain medicines.
You may need a pacemaker if:
- You have a slow or irregular heartbeat that lasts for a long time, also called chronic.
- You have heart failure.
A pacemaker only works when it senses trouble with the heartbeat. For example, if the heart beats too slowly, the pacemaker sends electrical signals to correct the beat.
Some pacemakers can increase the heartbeat as needed, such as during exercise.

The heart's conduction system
The heart's conduction system also is called the heart's electrical signaling system. Electrical signals start in a group of cells at the top of the heart called the sinus node. The signals tell the heart to beat. The sinus node also is called the heart's natural pacemaker. It can become weak as a person gets older.
A pacemaker may have two parts:
- Pulse generator. This small metal box has a battery and electrical parts. It controls the rate of electrical signals sent to the heart.
- Leads. These are flexible, insulated wires. One to three wires are placed in one or more of the heart's chambers. The wires send the electrical signals needed to correct an irregular heartbeat. Some newer pacemakers don't need leads. These devices are called leadless pacemakers.
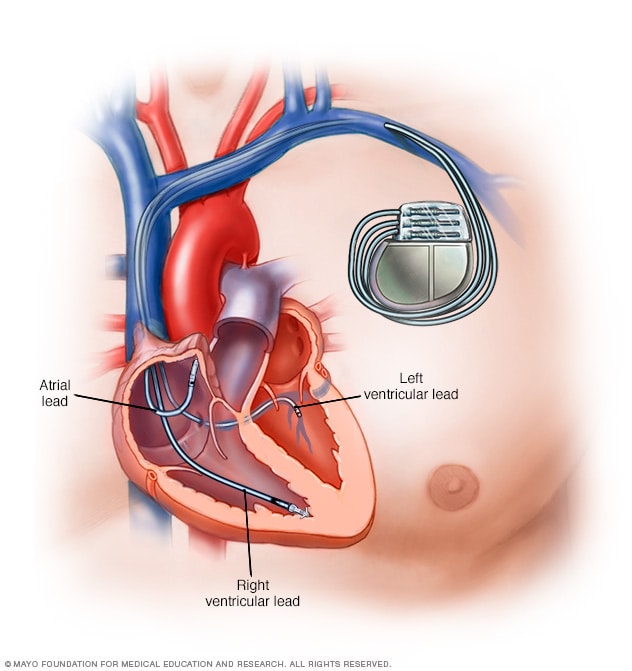
A pacemaker is a device used to control an irregular heart rhythm. A pacemaker has flexible wires called leads. The wires are placed in one or more chambers of the heart. They deliver electrical signals to fix the heart rate. Some newer pacemakers don't need wires.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Possible complications of a pacemaker device or its surgery may include:
- Infection near the site in the heart where the device is placed.
- Swelling, bruising or bleeding, especially if you take blood thinners.
- Blood clots near where the device is placed.
- Damage to blood vessels or nerves.
- Collapsed lung.
- Blood in the space between the lung and the chest wall.
- Moving or shifting of the device or leads, which could cause a hole in the heart. This complication is rare.
How you prepare
Several tests are done to determine if a pacemaker is right for you. These tests may include:
- Electrocardiogram (ECG or EKG). This quick and painless test checks the heart's electrical activity. An ECG shows how the heart is beating. Some personal devices, such as smartwatches, can check the heartbeat. Ask a member of your health care team if this is an option for you.
- Holter monitor. This portable device is worn for a day or more to record the heart's rate and rhythm during daily activities. It may be done if an ECG doesn't provide enough details about a heart problem. A Holter monitor may be able to see irregular heart rhythms that an ECG missed.
- Echocardiogram. An echocardiogram uses sound waves to create pictures of the beating heart. It shows how blood flows through the heart and heart valves.
- Stress or exercise tests. These tests often involve walking on a treadmill or riding a stationary bike while the heart's rate and rhythm are watched. Exercise tests show how the heart responds to physical activity. Sometimes, a stress test is done with other imaging tests, such as an echocardiogram.
What you can expect
Before the procedure.
Surgery is needed to place a pacemaker in the body. The surgery usually takes a few hours.
Your chest is cleaned with a special soap. A member of your health care team puts an IV into your forearm or hand. Medicine called a sedative goes through the IV. It helps you relax.
Usually, medicine is used to numb the skin where the pacemaker will be inserted. This medicine is called local anesthesia. During the pacemaker surgery, you may be fully awake or lightly sedated.
During the procedure
To place a pacemaker, a doctor inserts one or more wires into a major vein under or near the collarbone. The doctor uses X-ray images to guide the wires to the heart. One end of each wire attaches to the proper area in the heart. The other end connects to the part of the pacemaker that delivers electrical pulses. That part is called a pulse generator. It usually is placed under the skin beneath the collarbone.
A leadless pacemaker is smaller. All the parts are inside a single unit. It's placed into the heart using a thin, flexible tube called a catheter. The doctor inserts the tube into a blood vessel, usually in the groin. The leadless pacemaker goes through the tube. It's guided to the proper area in the heart.
After the procedure
You may stay in the hospital for a day after getting a pacemaker. The device is programmed to fit your heart rhythm needs before you leave. Make plans to have someone drive you home from the hospital.
For the first month after getting a pacemaker, you may be told not to do any heavy lifting or exercise that uses a lot of energy. Do not put pressure on the area where the pacemaker was placed. Your health care team tells you what medicines you safely can take if you have pain.
Special precautions
A pacemaker doesn't usually stop working because of electrical interference. But it's a good idea to follow a few safety tips if you have a pacemaker.
- Mobile phones. It's safe to talk on a mobile phone. But keep the phone at least 6 inches (15 centimeters) away from your pacemaker. Don't keep your phone in a shirt pocket. When talking on your phone, hold it to the ear opposite the side where your pacemaker was placed.
- Security systems. Passing through an airport metal detector won't interfere with a pacemaker. But the metal in the pacemaker could sound the alarm. Do not stay too long near a metal-detection system. Carry an ID card that says you have a pacemaker.
- Medical equipment. Tell all of your health care team members, including dentists, that you have a pacemaker. Some imaging tests and treatments may interfere with the device. These tests and treatments include MRI or CT scans, radiation therapy for cancer, the use of an electric current to control bleeding during surgery, and sound wave therapy to break up large kidney stones or gallstones.
- Power-generating equipment. Stand at least 2 feet (61 centimeters) from welding equipment, high-voltage transformers or motor-generator systems. If you work around such equipment, ask your health care team if a safety test can be done at your workplace. The test can check whether the equipment affects your pacemaker.
Devices that are not likely to interfere with a pacemaker include:
- Electric blankets.
- Electric razors.
- Microwave ovens.
- Personal computers.
- Televisions and remote controls.
A pacemaker should improve symptoms caused by a slow heartbeat, such as extreme tiredness, lightheadedness and fainting. Most modern pacemakers automatically change the speed of the heartbeat to match the level of physical activity. A pacemaker may let you have a more active lifestyle.
Regular health checkups are recommended after getting a pacemaker. Ask your health care team how often you need to go into a medical office for such checkups. Tell your health care team if you gain weight, if your legs or ankles get puffy, or if you faint or get dizzy.
A health care professional should check your pacemaker every 3 to 6 months. Most pacemakers can be checked remotely. This means you don't have to go into a medical office for the checkup. A pacemaker sends information about the device and your heart electronically to your doctor's office.
A pacemaker's battery typically lasts 5 to 15 years. When the battery stops working, you'll need surgery to replace it. The surgery to change a pacemaker's battery is often quicker than the first surgery to place the device. You also should have a quicker recovery.
Pacemakers and end-of-life issues
If you have a pacemaker and become sick with a life-threatening condition that can't be cured, it's possible the device could make you live longer. There are mixed opinions about turning off a pacemaker in end-of-life situations.
Talk to your health care team if you have a pacemaker and are concerned about turning it off. You also may want to talk to your family or caregivers about what you'd like to do in an end-of-life situation. You might want to write your end-of-life wishes in an advanced directive. This is a legal document that tells your family and health care team what to do if you can't communicate.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Pacemaker care at Mayo Clinic
- Pacemaker. American Heart Association. https://www.heart.org/en/health-topics/arrhythmia/prevention--treatment-of-arrhythmia/pacemaker. Accessed Dec. 13, 2022.
- Pacemakers. National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health/pacemakers. Accessed Dec. 13, 2022.
- How the healthy heart works. American Heart Association. https://www.heart.org/en/health-topics/congenital-heart-defects/about-congenital-heart-defects/how-the-healthy-heart-works. Accessed Dec. 13, 2022.
- All about heart rate (pulse). American Heart Association. https://www.heart.org/en/health-topics/high-blood-pressure/the-facts-about-high-blood-pressure/all-about-heart-rate-pulse. Accessed Dec. 19, 2022.
- Mulpuru SK, et al. Cardiac pacemakers: Function, troubleshooting, and management: Part 1 of a 2-part series. Journal of the American College of Cardiology. 2017; doi:10.1016/j.jacc.2016.10.061.
- Living with your pacemaker. American Heart Association. https://www.heart.org/en/health-topics/arrhythmia/prevention--treatment-of-arrhythmia/living-with-your-pacemaker. Accessed Dec. 13, 2022.
- Devices that may interfere with ICDs and pacemakers. American Heart Association. https://www.heart.org/en/health-topics/arrhythmia/prevention--treatment-of-arrhythmia/devices-that-may-interfere-with-icds-and-pacemakers. Accessed Dec. 13, 2022.
- Link MS. Permanent cardiac pacing: Overview of devices and indications. https://www.uptodate.com/contents/search. Accessed Dec. 13, 2022.
- Madhavan M, et al. Advances and future directions in cardiac pacemakers: Part 2 of a 2-part series. Journal of the American College of Cardiology. 2017; doi:10.1016/j.jacc.2016.10.064.
- Libby P, et al., eds. Diagnosis and management of acute heart failure. In: Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Elsevier; 2022. https://www.clinicalkey.com. Accessed Dec. 13, 2022.
- Hutchison K, et al. Ethics and the cardiac pacemaker: More than just end-of-life issues. Europace. 2018; doi:10.1093/europace/eux019.
- Ami TR. Allscripts EPSi. Mayo Clinic. Dec. 21, 2022.
- Lee JZ, et al. Leadless pacemaker: Performance and complications. Trends in Cardiovascular Medicine. 2018; doi:10.1016/j.tcm.2017.08.001.
- Noseworthy PA (expert opinion). Mayo Clinic. June 28, 2021.
- Leadless pacing systems: Risk of major complications related to cardiac perforation during implantation ⸺ Letter to health care providers. U.S. Food and Drug Administration. https://www.fda.gov/medical-devices/letters-health-care-providers/leadless-pacing-systems-risk-major-complications-related-cardiac-perforation-during-implantation. Accessed Dec. 19, 2022.
- Mankad R (expert opinion). Mayo Clinic. Nov. 22, 2021.
- Cha YM (expert opinion). Mayo Clinic. April 30, 2023.
- Stühlinger M, et al. EHRA consensus on prevention and management of interference due to medical procedures in patients with cardiac implantable electronic devices. Europace. 2022; doi:10.1093/europace/euac040.
- Atrial flutter
- Bradycardia
- Bundle branch block
- Cardiomyopathy
- Chagas disease
- Enlarged heart
- Heart arrhythmia
- Heart disease
- Heart failure
- Hypertrophic cardiomyopathy
- Long QT syndrome
- Multiple system atrophy (MSA)
- Sick sinus syndrome
- Tachycardia
- The conduction system
- Ventricular tachycardia
News from Mayo Clinic
- A heart full of gratitude Oct. 27, 2022, 11:00 a.m. CDT
- Sharing Mayo Clinic: A heart patient's fall picks up something big May 15, 2022, 11:00 a.m. CDT
Mayo Clinic in Rochester, Minnesota, has been recognized as one of the top Cardiology & Heart Surgery hospitals in the nation for 2023-2024 by U.S. News & World Report.
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
You Are Leaving the Medtronic Canada Site
You just clicked a link to go to another website. If you continue, you will leave this site and go to a site run by someone else.
Medtronic Canada does not review or control the content on the other website, and is not responsible for any business dealings or transactions you have there. Your use of the other site is subject to the terms of use and privacy statement on that site.
It is possible that some of the products on the other site not be licensed for sale in Canada.
Your browser is out of date
With an updated browser, you will have a better Medtronic website experience. Update my browser now.
Bradycardia Your Health
Living With the Therapy
Daily Living – Pacemakers
Many people with an implantable heart device resume their normal daily activities after full recovery from surgery. However, there may be certain situations that your doctor will ask you to avoid.
Your doctor or nurse will provide guidance for your particular condition, but these are some general guidelines to follow after your recovery.
You can gradually return to your normal lifestyle once your doctor says it’s safe to do so. Most individuals can resume exercising after recovery.
However, you should avoid rough physical contact that could cause you to fall or hit your implant site, as this could damage the device or leads. Talk to your doctor if you have questions about specific activities.
Most people with implanted heart devices can travel freely unless they are restricted by their underlying medical condition.
The key to travelling with confidence is to plan in advance. Before you leave on your trip, talk to your doctor about:
- Specific care or activity recommendations
- Steps to take if you experience discomfort or symptoms
- Finding a heart centre, emergency service, or doctor at your travel destination
More: Travel with Confidence
Airport Security
You may also have concerns about airport security systems. Before walking through an airport security gate, let security personnel know you have a heart device, and show your identification card. Then, walk through the archway at a normal pace and move away from the system if you feel any dizziness or rapid heartbeats.
Airport security systems are metal detectors, so the alarm may sound when it detects the metal case of your heart device. If airport security uses an electronic wand to clear passengers, ask the security attendant to avoid placing or waving the wand back and forth over your implanted heart device. More: Electromagnetic Compatibility
Medical and Dental Procedures
Before undergoing any medical procedure, always tell the doctor, dentist, or technician that you have an implanted heart device. They may need to speak with your heart doctor before performing the procedure, especially if the procedure is new or unusual.
Some procedures may potentially affect the function of your heart device, and such procedures may require precautionary measures to prevent or minimise any impact on you or your device.
Medical Procedure Warnings
People with metal implants such as an implanted heart device and accompanying leads should not receive the following medical procedures:
- Catheter microwave ablation
- Diathermy treatment (high frequency, short wave, or microwave)
- Transurethral needle ablation (TUNA)
Medical Procedure Precautions
Some medical procedures can be safely performed, if certain precautions are taken by your doctor to avoid potential device function problems or interference:
- Computerised axial tomography (CT or CAT) scan
- MRI (some pacemakers and leads are MRI conditional)
- Diagnostic ultrasound
- Electrocautery
- Electrolysis
- External defibrillation and elective cardioversion
- High-energy radiation therapy
- Hyperbaric oxygen therapy (HBOT)
- Lithotripsy
- Radio frequency ablation
- Therapeutic ultrasound
- Transcutaneous electrical nerve stimulation (TENS)
- Transmitting loop for digital hearing aid
Acceptable Medical Procedures
Many medical procedures will not affect your heart device. However, the equipment used for the procedure must be used correctly and must be maintained properly.
- Dental procedures that use drills or ultrasonic probes to clean teeth are acceptable. Dental x-rays are also acceptable.
- Diagnostic x-rays, such as chest x-rays and mammograms, are acceptable.
Talk with your doctor to weigh any potential risk against the benefits of the medical procedure.
Electromagnetic Compatibility
Fields of energy around certain types of equipment that use electricity and magnets may affect the normal operation of your implanted heart device. The energy fields created around electrical items can be strong or weak. The closer to the item you are, the stronger the energy field.
Electromagnetic compatibility means that the electrical energy field generated by an electrical item is compatible with other electrically sensitive items, such as an implanted heart device.
Most electromagnetic energy fields are small and weak and do not affect your heart device, but electrical items with a strong energy field, like welders or petrol-powered chain saws, may affect the therapy delivered by your device.
Talk to your doctor and review the electromagnetic compatibility guide below. More: Electromagnetic Compatibility
Support Groups
Some individuals find it helpful to join a support group. There are many support groups that can help with the transition to living with an implanted heart device.
Local hospitals, healthcare centres, community centres, and local newspapers may provide information about support groups for individuals and their caregivers.
Information on this site should not be used as a substitute for talking with your doctor. Always talk with your doctor about diagnosis and treatment information.
- Open share options
- Close share options
- EXPLORE Random Article
How to Travel With a Pacemaker
Last Updated: January 21, 2022 Approved
wikiHow is a “wiki,” similar to Wikipedia, which means that many of our articles are co-written by multiple authors. To create this article, 15 people, some anonymous, worked to edit and improve it over time. There are 8 references cited in this article, which can be found at the bottom of the page. wikiHow marks an article as reader-approved once it receives enough positive feedback. This article received 11 testimonials and 95% of readers who voted found it helpful, earning it our reader-approved status. This article has been viewed 236,319 times.
A pacemaker is an artificial device that is surgically placed in a patient's chest cavity in order to control abnormal heartbeat. Pacemakers are often used to treat heart conditions, like arrhythmia, where the heartbeats at an abnormal pace, too fast or too slow. The device sends an electronic pulse that regulates the beat, which then controls the blood that circulates through the patient's body. Pacemakers can be temporary or permanent, and modern versions can produce data about the patient's vital signs. Pacemakers are electronic, but some versions are covered with metal. If you plan to travel, it is important to follow protocol according to unseen disabilities. Read on to find out how to travel with a pacemaker.

- There have been some reports that metal detector gates can affect pacemakers or Implantable Cardioverter Defibrillators (ICD). For this reason, a metal detecting wand would be preferable. There is no evidence to show that the in-flight environment affects pacemakers adversely. [5] X Trustworthy Source PubMed Central Journal archive from the U.S. National Institutes of Health Go to source
- If your doctor has told you that any metal detection wands or metal detection gates may have an adverse effect, you can ask the travel security staff for a private pat-down, after showing them your pacemaker identification card.

- Never linger near large electronic devices. This could be anything from a device in a museum to a large speaker system. These devices can interfere with the pacemaker.

Expert Q&A
- Some people feel uncomfortable when they need to be taken to a separate screening area. This is the general procedure for anyone with metal implants, such as hip or knee replacements. Although it may take longer, it is not indicative of having done anything wrong. You can ask the security officer to be discreet when doing your personal metal detector wand screening. Thanks Helpful 0 Not Helpful 1
- Many travelers choose to invest in medical travel insurance. This is a good idea especially for those with chronic conditions who are traveling to countries without socialized or reciprocal medical agreements. You may need to pay more to have a plan with a pacemaker, but it ensures peace of mind during your travels. Thanks Helpful 1 Not Helpful 0
- Do not stand in an electronic metal detector gate for more than 15 seconds. Research has shown that this can interrupt a pacemaker. Most people walk through metal detector gates in less than 5 seconds. Thanks Helpful 16 Not Helpful 5
Things You'll Need
- Pacemaker identification card
- Doctor's advice
- Private security screening
- List of pacemaker treatment facilities
- Travel insurance
You Might Also Like

- ↑ https://www.tsa.gov/travel/frequently-asked-questions/what-are-procedures-if-i-have-internal-or-external-medical-device
- ↑ https://www.heart.org/en/health-topics/arrhythmia/prevention--treatment-of-arrhythmia/pacemaker-wallet-identification-card
- ↑ https://www.nhs.uk/conditions/pacemaker-implantation/recovery/
- ↑ https://www.tsa.gov/travel/special-procedures
- ↑ https://www.ncbi.nlm.nih.gov/pubmed/2462212
- ↑ https://www.ncbi.nlm.nih.gov/pubmed/9744443
- ↑ http://www.medtronic.com/traveling/
- http://www.medtronic.com/patients/bradycardia/living-with/daily-living/index.htm
About this article
Reader success stories.
John Stodgel
Apr 24, 2019
Did this article help you?
Afshan Baig
Jul 6, 2019
Kanakarao Pilli
May 5, 2016
Holly Zilafro
Sep 25, 2016
Suzie Martin
Aug 19, 2017

- About wikiHow
- Terms of Use
- Privacy Policy
- Do Not Sell or Share My Info
- Not Selling Info
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Pacemaker Implantation Surgery: Everything You Need to Know
How to prepare.
- What to Expect
A pacemaker is a device that is surgically implanted under the skin of the chest to mimic the electrical pulses that regulate heartbeats. Pacemaker surgery may be an outpatient procedure or an inpatient procedure based on your health and the cause of the rhythm disorder.
A pacemaker is used for long-term correction of a too-slow heartbeat ( arrhythmia ) or temporarily, such as after open-heart surgery . Implanting a pacemaker is considered a minimally invasive procedure.
This article discusses pacemaker implantation surgery, its purpose, and some of the risks and contraindications. It also goes over what to expect before, during, and after the procedure.
What Is Pacemaker Surgery?
Pacemaker surgery is done to implant a pacemaker device.
A pacemaker is comprised of a pulse generator that houses a battery and circuitry, as well as one to three small electrical leads that are placed in the chambers of the heart. Each electrical pulse emitted by the pacemaker stimulates a heartbeat and is timed to ensure a normal heart rhythm.
Pacemaker surgery is used to treat a wide range of heart rhythm disorders. While typically performed in adults with heart disease , it is also used in children with congenital heart conditions .
Most pacemakers are implanted using local anesthesia , although you may also receive intravenous (IV) sedation to help you relax.
There are different types of pacemakers used to treat different types of arrhythmia. They are broadly categorized as follows:
- Single-chamber pacemakers deliver the electrical impulse to a single chamber of the heart. They are most often used to pace the right ventricle in people with chronic atrial fibrillation and require pacing to maintain an adequate heart rate.
- Dual-chamber pacemakers are used when the timing of the chamber contractions is misaligned. The device corrects this by delivering synchronized pulses to the right atrium and right ventricle (lower chamber).
- Biventricular pacemakers , also called cardiac resynchronization therapy, are for people with heart failure . They work to ensure synchronous contraction of the right and left ventricles causing them to pump together and improve cardiac function.
There are also combination devices called automated implantable cardioverter-defibrillators (AICDs) that contain both a pacemaker and a defibrillator . In addition to regulating heart rhythm, AICDs deliver a jolt of electricity when needed to correct ventricular tachycardia or ventricular fibrillation (irregular heartbeats).
Most pacemakers last for about six to 10 years before they need to be replaced. AICDs often need replacement earlier—between three and six years, on average.
Contraindications
Pacemaker surgery is a common and effective procedure but one that may not be appropriate for everyone. The decision to implant the device is made on a case-by-case basis based on a review of the benefits and risks of treatment.
Pacemakers are generally contraindicated if a heart rhythm disorder is identified during a cardiac evaluation but is not causing symptoms.
People with sleep apnea may experience bradycardia during sleep ; because this can often be successfully resolved by treating the underlying condition, a pacemaker is not usually considered beneficial.
Potential Risks
In addition to the general risks of surgery and anesthesia , pacemaker surgery presents its own risks and concerns. Although the surgery is considered to be low risk, around 3% of pacemaker recipients will experience some form of complication ranging from mild and treatable to potentially life-threatening.
Risks and complications of pacemaker implantation surgery include:
- Electrode lead dislodgment
- Phlebitis (venous inflammation)
- Hemothorax (accumulation of blood between the chest wall and lungs)
- Pneumothorax (collapsed lung)
- Post-operative infection
- Cardiac perforation and tamponade
- A severe thromboembolic event in which the formation of a blood clot can lead to stroke , heart attack , pulmonary embolism , or deep vein thrombosis (DVT)
According to a 2019 study in the Journal of Clinical Medicine, pneumothorax and lead dislodgment were the two most common complications, occurring at a rate of 3.87% and 8.39%, respectively.
Severe complications, like stroke, occur in less than 2% of cases and usually in people with pre-existing risk factors.
Purpose of Pacemaker Surgery
Having a pacemaker implanted often helps you feel better so you can return to your daily routine without symptoms like dizziness, palpitations , breathlessness, difficulty exercising, and fainting.
Pacemaker implantation can improve your quality of life, though it is important to maintain communication with your healthcare team after implantation and follow up with your provider as required.
Click Play to Learn All About Pacemaker Surgery
This video has been medically reviewed by Anju Goel, MD, MPH .
In addition, your life expectancy may improve. Research has found that life expectancy in people with pacemakers who do not have significant underlying medical conditions (e.g., heart failure, atrial fibrillation, or other serious non-cardiac conditions) approaches that of the general population.
The indications for a pacemaker have increased in recent decades. According to the American College of Cardiology (ACC), the American Heart Association (AHA), and the Heart Rhythm Society (HRS), pacemakers are appropriate for the following conditions and medical needs:
- Sinus node dysfunction: Abnormally fast or slow heartbeats emanating from the atria of the heart
- Acquired atrioventricular block: Abnormal heart rhythms when the electricity generated in the atrium is not able to conduct down to the ventricles.
- Chronic bifascicular block: Heart rhythm problems caused by a block in the fascicles , which are located in the lower chambers of the heart.
- Tachycardias : Both atrial and ventricular
- Heart rhythm problems caused by myocardial infarction (heart attack)
- Heart rhythm problems caused by congenital heart disease
- Heart rhythm problems caused by hypertrophic cardiomyopathy (the abnormal thickening of a portion of the heart)
- Vasovagal syncope : Fainting caused by a neurologic overreaction to certain triggers
- Cardiac resynchronization therapy in people with severe systolic heart failure
- Post-heart transplant measures to maintain normal heart rhythms
With that said, being diagnosed with any of these conditions does not mean you will get (or should get) a pacemaker.
To determine the need, a healthcare provider will perform tests to decide if the condition is Class I (in which the benefits outweigh the risks), Class IIa (benefits may outweigh the risks), Class IIb (benefits are equal to or greater than the risks), or Class III (risks may outweigh the benefits).
To classify the severity, pre-operative tests may be performed, including:
- Electrocardiogram : A non-invasive procedure used mainly to assess the structural and hemodynamic components of the heart.
- Holter monitoring : A portable type of ECG used to monitor heart rhythms over periods of time
- Echocardiogram : A non-invasive test that measures heart rate based on echoed sound waves
- Cardiac stress test : A procedure that measures heart rate while performing exercise on a treadmill or stationary cycle
Pacemaker implantation is a common surgery but one that requires preparation. Once a pacemaker has been recommended, you will meet with a cardiologist or general surgeon to discuss the procedure, how to prepare, and what to expect.
Pacemaker surgery takes place in an operating room or cardiac catheterization lab of a hospital or specialized surgical center.
The room will be equipped with an ECG machine, a mechanical ventilator , and a "crash cart" used in the event of a cardiac emergency. It will also have a fluoroscope—a machine that uses X-rays to produce live images of the heart to guide the placement of the pacemaker leads.
What to Wear
If the surgery is performed on an outpatient basis, you should wear clothes you can get into/out of easily. You will be asked to change into a hospital gown and to remove any hairpieces, eyewear, dentures, hearing aids, and tongue or lip piercings.
If the surgery requires an overnight hospital stay for observation purposes, bring only what you need for the stay, including toiletries, daily medications, a comfortable robe and slippers, your cell phone and charger, and an extra pair of socks and underwear. Leave any valuables at home.
Food and Drink
You will need to stop eating at midnight the night before your surgery. On the day of the surgery, you are allowed a few sips of water to take your morning pills, if applicable.
Within four hours of the operation, nothing should be taken by mouth, including water, chewing gum, or sweets. Most pacemaker surgeries are performed in the morning to accommodate the prolonged fasting period.
Medications
Medications that promote bleeding must be avoided before pacemaker surgery. Some may need to be stopped a day or so beforehand, while others may need to be avoided for a week or more before and after surgery. These include:
- Anticoagulants (blood thinners) like Coumadin (warfarin)
- Antiplatelet medications , such as Plavix (clopidogrel)
- Nonsteroidal anti-inflammatory drugs (NSAIDs) like aspirin, Advil (ibuprofen) , Aleve (naproxen) , Celebrex (celecoxib), and Mobic (meloxicam)
To avoid complications and interactions, advise your healthcare provider about any drugs you are taking, whether they are prescription, over-the-counter, nutritional, herbal, and recreational.
What to Bring
You will need to bring a driver's license or some other form of government ID to register at hospital admissions. You will also be asked for your insurance card. Although most facilities will bill for their services, some may ask for the upfront payment of copay or coinsurance costs.
Call in advance to ensure that the facility accepts your insurance and that all providers, including the anesthesiologist , are in-network providers . If upfront payment is requested, ask what form of payment the office accepts.
You will also need to bring someone with you to drive you home. Even if only local anesthesia is used, your arm will be in a sling for 24 to 48 hours after the procedure. This, along with the aftereffects of IV sedation, makes driving hazardous.
What to Expect on the Day of Surgery
On the morning of the surgery, you will need to wash with an antiseptic wash provided by your healthcare provider. Avoid putting on any lotions, makeup, creams, nail polish, or fragrance.
You'll meet an anesthesiologist and an operating nurse who are part of the team accompanying the cardiologist or general surgeon performing the procedure.
Before the Surgery
When you arrive at the hospital, you will be asked to register, fill out a medical history form, and sign a consent form stating that you understand the aims and risks of the procedure.
After this, you are led to the back to change into a hospital gown. A nurse will record your height, weight, and vital signs , and perform a panel of blood tests to ensure there are no conditions that contraindicate surgery.
Other pre-operative procedures include:
- Chest shaving: If your chest is hairy, the implantation site will need to be shaved. Do not shave the area yourself.
- ECG monitoring: Adhesive electrodes are placed on various parts of your chest to connect to the ECG machine.
- Pulse oximetry: A device called a pulse oximeter is clamped onto a finger to monitor your blood oxygen levels .
- IV prep: The intravenous tube, called a catheter, is inserted into a vein in your arm or wrist to deliver medications and fluid.
During the Surgery
Once you are prepped, you are wheeled into the operating room and placed on a table in an upward-facing (supine) position under the fluoroscope.
Local anesthesia is given to numb the surgical site. A sedative may also be delivered through the IV line to help you relax and place you in a "twilight sleep" (referred to as monitored anesthesia care (MAC) . To reduce the risk of infection, an intravenous antibiotic will also be delivered.
Once the anesthesia takes effect, the chest will be swabbed with an antibacterial solution and the body covered with sterile drapes.
An incision is then made on the chest near the shoulder (usually the left) to place the pacemaker. Using the fluoroscope, the healthcare provider will implant one or more leads into the appropriate chambers of the heart. The end of leads are secured.
Once the pacemaker is properly positioned under the skin, the device is tested. The incision is closed with sutures or adhesive strips, and a sling is placed on your arm to immobilize the arm and shoulder and prevent lead dislodgment.
From start to finish, pacemaker surgery takes around 30 minutes. The implantation of an AICD can take longer (usually around an hour).
After Surgery
After surgery, you are wheeled to the recovery room. Most people wake up from anesthesia with MAC in 10 minutes or so, although the effects of the drugs can persist for four to six hours. When you awaken, the nurse will monitor your condition and may offer you a light snack and drink.
It is not unusual to feel some pain and discomfort around the implantation site immediately after surgery. Your healthcare provider will provide medications to help control these symptoms at home. If you feel sick from the anesthesia, the nurse may be able to provide you with anti-nausea medications .
Once your vital signs are stable, you will either be wheeled to your hospital room for overnight observation or allowed to leave in the care of a friend or family member if you are an outpatient.
As the local anesthesia begins to wear off, you are likely to feel more pain and pressure around the wound. This can be controlled with over-the-counter Tylenol (acetaminophen) or a short course of prescription opioid painkillers.
In addition to painkillers, your healthcare provider may prescribe a course of oral antibiotics (for less than 10 days) to help prevent infection.
Bruising in the area where the pacemaker was placed is normal and common. The device will create an area of raised skin on the chest that can be felt and/or seen; this will be permanent.
With proper care and wound management, most people who have undergone pacemaker surgery are able to return to normal activity within four weeks.
You will need to wear your arm sling for 24 to 48 hours as directed by your healthcare provider (including while you sleep).
It is important to keep the wound as dry as possible for the first five days until the wound is sufficiently healed. Avoid bathing or showering for the first day. Thereafter, take a bath instead of a shower or ask your practitioner for a disposable adhesive patch (called AquaGard) to create a watertight barrier when showering.
Your wound dressing should be changed daily for the first five to seven days using a sterile pad and alcohol-free topical antiseptic provided by your healthcare provider. Check the wound daily and call your practitioner if there are any signs of infection or abnormal healing.
When to Call a Healthcare Provider
Call your practitioner or surgeon immediately if you experience any of the following after pacemaker surgery:
- Increasing redness, pain, and swelling at the implantation site
- High fever (100.5 degrees F) with chills
- A yellowish-green discharge from the wound, often foul-smelling
- An opening wound ( incision dehiscence )
After seven to 10 days, you will need to see your healthcare provider to have the stitches removed and the wound checked.
Physical Activity
Upon your return home, you should move as little as possible, in part to prevent lead dislodgment but also to reduce pain. Even after the stitches are out, you will need to avoid raising the arm nearest to the pacemaker for the next one to two weeks.
Do not drive until the healthcare provider gives you the OK, and avoid strenuous exercises or the lifting of heavy objects. You will be given the go-ahead to resume sex once your wound site heals (around one to two weeks).
Once you're cleared to get back to your normal routine, it is important to keep physically active to improve blood circulation and maintain the normal range of motion in the shoulder. Speak with your cardiologist about an appropriate exercise plan or ask for a referral to a qualified physical therapist .
High-impact sports should be permanently avoided as heavy blows can damage the device.
Follow-Up Care
Once you have healed, you may notice a dramatic improvement in your energy levels and stamina. The pacemaker helps your heart work efficiently, reducing fatigue and allowing you to be more active.
One of the keys to sustaining good health is routine visits with your cardiologist. Most healthcare providers will want to schedule the first follow-up within six months of the implantation and then every six to 12 months thereafter, depending on the type of pacemaker used.
This helps ensure that the pacemaker is working properly and that adjustments are made when needed to prolong the life of the device.
Your cardiologist may also ask you to check and write down your pulse at home. This is done to ensure your pacemaker is working well and keeping your heart rate within an appropriate range.
Be sure you are clear on when and how to get in touch with your practitioner after taking your pulse.
How Long Do Pacemaker Batteries Last?
Pacemaker batteries last between five and 10 years. After this time, you will need surgery to replace the pulse generator. In most cases, this procedure can be done on an outpatient basis.
Lifestyle Adjustments
After your pacemaker is implanted, you will need to avoid magnetic fields, as they can interfere with the function of the device.
For example, refrain from placing small electronics, such as your cell phone, in your breast pocket and going through metal detectors.
You'll receive a medical ID card that provides details about your pacemaker including the type, manufacturer, date of implant, and the healthcare provider's name who implanted it. You should carry this with you at all times.
Alternatively, consider purchasing a custom medical ID bracelet that has the pacemaker information engraved on it.
This is helpful not only in emergency care situations in which you cannot convey your medical history, but also in situations that may expose you to magnetic fields, such as:
- When a magnetic resonance imaging (MRI) scan is recommended for any reason (alert your healthcare provider and radiologist)
- Security checks—You can show your card or bracelet to security staff at an airport so that they can check you using a manual search or a screening wand instead of a walk-through scanner.
Pacemaker implantation is a minimally invasive procedure to implant a pacemaker device, which can help treat a number of conditions that cause problems with heart rhythm. A pacemaker can help improve symptoms like palpitations, breathlessness, and trouble exercising.
The pacemaker is implanted during a procedure involving local anesthesia. You may also receive a sedative. The surgeon will make a small incision on your chest near your shoulder and implant one or more leads into your heart. Depending on your condition and overall health, you may be able to go home on the same day, or you may be kept in the hospital overnight for observation.
Kotsakou M, Kioumis I, Lazaridis G, et al. Pacemaker insertion . Ann Transl Med. 2015;3(3):42. doi:10.3978/j.issn.2305-5839.2015.02.06
American Heart Association. Implantable cardioverter defibrillator (ICD) .
De Vries LM, Leening MJG, Dijk WA, Hooijschuur CAM, Stricker BHC, Van Hemel NM. Trends in service time of pacemakers in the Netherlands: a long-term nationwide follow-up study . Neth Heart J . 2017;25(10):581-91. doi:10.1007/s12471-017-1024-x
Madhavan M, Waks JW, Friedman PA, et al. Outcomes after implantable cardioverter-defibrillator generator replacement for primary prevention of sudden cardiac death . Circ Arrhythm Electrophysiol . 2016;9(3):e003283. doi:10.1161/CIRCEP.115.003283
Sidhu S, Marine JE. Evaluating and managing bradycardia . Trends Cardiovasc Med . 2020;30(5):265-272. doi:10.1016/j.tcm.2019.07.001
Ranasinghe I, Labrosciano C, Horton D, et al. Institutional variation in quality of cardiovascular implantable electronic device implantation: A cohort study . Ann Intern Med . 2019;171(5):309-17. doi:10.7326/M18-2810
Carrión-Camacho MR, Marín-León I, Molina-Doñoro JM, González-López JR. Safety of permanent pacemaker implantation: A prospective study . J Clin Med . 2019;8(1):35. doi:10.3390/jcm8010035
Edwards SJ, Karner C, Trevor N, et al. Description of health problem . Dual-chamber pacemakers for treating symptomatic bradycardia due to sick sinus syndrome without atrioventricular block: a systematic review and economic evaluation . Southampton (UK): NIHR Journals Library; 2015.
Polikandrioti M. Patient perceptions and quality of life in pacemaker recipients . J Innov Card Rhythm Manag . 2021;12(11):4769-4779. doi:10.19102/icrm.2021.121103
Bradshaw PJ, Stobie P, Knuiman MW. Life expectancy after implantation of a first cardiac permanent pacemaker (1995-2008): A population-based study . Int J Cardiol . 2015;190:42-6. doi:10.1016/j.ijcard.2015.04.099.
Kusumoto FM, Schoenfeld MH, Barrett C, et al. 2018 ACC/AHA/HRS guideline on the evaluation and management of patients with bradycardia and cardiac conduction delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society . Circulation . 2019;140(8):e382-e482. doi:10.1161/CIR.0000000000000628
Bansal S, Chakraborty P. Cardiac pacemakers: Indications, choices and follow up .
Oo ZT, Bhavsar D, Aung TPP, Ayala-Rodriguez CE, Kyaw H. Exercise stress test-induced atrioventricular dissociation with syncope . Ochsner J . 2021;21(3):319-324. doi:10.31486/toj.20.0134
Alturki A, Proietti R, Birnie DH, Essebag V. Management of antithrombotic therapy during cardiac implantable device surgery . J Arrhythm . 2016;32(3):163-9. doi:10.1016/j.joa.2015.12.003
Sohn HM, Ryu JH. Monitored anesthesia care in and outside the operating room . Korean J Anesthesiol . 2016;69(4):319-26. doi:10.4097/kjae.2016.69.4.319
Biocic M, Vidosevic D, Boric M, et al. Anesthesia and perioperative pain management during cardiac electronic device implantation . J Pain Res . 2017;10:927-32. doi:10.2147/JPR.S132241
University of Michigan Medicine. Arrhythmias and sexual activity .
American Heart Association. Living with your pacemaker .
American Heart Association. Pacemaker identification - wallet card .
By Jennifer Whitlock, RN, MSN, FN Jennifer Whitlock, RN, MSN, FNP-C, is a board-certified family nurse practitioner. She has experience in primary care and hospital medicine.
- International eng
- Australia eng
- Germany deu
CARDIOVASCULAR
Traveling with your device.

Traveling with your device is generally easy and safe.
Here are some things to know or consider, first, consult with your doctor..
It’s important to notify your care team about your plans, so they can:
- Help you connect with a doctor at your destination, just in case you need care
- Help you plan for the right level of exercise or activity while you’re away
- Create a travel and emergency action plan for long-distance trips
- Talk with you about travel safety rules for equipment
- Help you think through how to manage any possible issues
- Provide any other relevant information
What to bring with you
- Pack any medications. Bring about a week’s more than you expect to need for the trip. If traveling by plane, pack your medication in your carry-on so it’s with you for the entire journey.
- Bring a photocopy of the prescriptions your doctor wrote, along with any related insurance or pharmacy information so you can get prescriptions filled while you’re away.
- Make sure to carry your patient ID card wherever you go.
- Ask your doctor for the last printout from your device at your most recent evaluation.
Traveling by plane? Rest easy. Air travel, including passing through airports, is safe. It’s also simple, if you know what to look for.
Security Checkpoints
When you go through security checkpoints, full body scanners that utilize millimeter technology may be preferable, if available, for your device.
If your physician has directed you otherwise, or you are uncomfortable using the metal detectors or scanners, request a full-body pat down as an alternative security screening.
Move through metal detectors at a normal walking speed . Don’t pause for more than a few seconds.
If your device sets off the detector , tell security personnel about it and present your ID.
If security personnel use a handheld wand for scanning, ask them to move it over your device or PA sensor area quickly.
For people with a HeartMate™ LVAD
Metal detectors and body scanners can interfere with your pump. Ask for a hand search .
For people with a CardioMEMS™ HF System
Bring this travel letter with you when you fly.
On your flight, stay hydrated and move around as much as possible. When you’re sitting, do simple ankle rotations and leg movements to keep the blood circulating in your body.
Car and RV Travel
If you’re traveling by car or RV, consider the following recommendations:
- Tell family or a close friend where you’ll be going and what your route will be in case any issues come up on the road.
- Keep your cell phone handy and charged if you have one, so you can be in touch any time you may need support or assistance.
If you have a HeartMate™ LVAD
Avoid riding in the front seat of cars with airbags. (The impact force during an accident could cause serious damage or bleeding.)
Your doctor will tell you whether it’s safe for you to drive an automobile when you have a pump. Usually, you need to wait at least 6-8 weeks after surgery before your doctor will approve you to drive. Some states have laws against letting people with a history of fainting, dizziness or cardiac arrest behind the wheel.
Cruise Ships
Cruise ships often have a doctor and medical services on board. Before booking your trip:
- Ask if the cruise ship provides medical resources.
- Find out if the ship offers group cruises for people with implanted devices.
Questions? Get support.
Contact us with questions about your cardiac device..

MAT-2101896 v2.0
POLICIES & ADVISORIES
- Advertising Preferences
- Consumer Health Data Privacy Policy
- Customer Service
- Privacy Policy
- Product Advisories
- Terms and Conditions
HEALTHCARE PROFESSIONALS
- Disease Management
- Education & Training
- Reimbursement
- Manuals & Technical Resources
- Investigator Sponsored Studies
- Product & Charitable Donations
- Product Performance Reports
PATIENTS & CAREGIVERS
- Treatments & Therapies
- Manage Your ID Card
- Traveling with Your Device
- Get Support
STAY CONNECTED
CAUTION: These products are intended for use by or under the direction of a physician. Prior to use, reference the Instructions for Use, inside the product carton (when available) or online for more detailed information on Indications, Contraindications, Warnings, Precautions and Adverse Events. Illustrations are artist's representations only and should not be considered as engineering drawings or photographs. Unless otherwise specified, all product names appearing in this Internet site are trademarks owned by or licensed to Abbott, its subsidiaries or affiliates. No use of any Abbott trademark, trade name, or trade dress in this site may be made without the prior written authorization of Abbott, except to identify the product or services of the company. ™ Indicates a trademark of the Abbott group of companies. ‡ Indicates a third party trademark, which is property of its respective owner. © 2024 Abbott. All Rights Reserved. MAT-1900882 v12.0

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases and Disorders Education Program
- Publications and Resources
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- Clinical Trials
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- < Back To Pacemakers
- After Getting a Pacemaker
- What Are Pacemakers?
- How They Work
- Who Needs Them
- Before Getting a Pacemaker
- What to Expect
- Living With a Pacemaker
MORE INFORMATION
Pacemakers After Getting a Pacemaker
Language switcher.
After getting a permanent pacemaker, you will recover in the hospital for a few hours or overnight. Your healthcare team will tell you about any precautions or problems to watch out for during your recovery. You will receive a card with information about the device and its settings, your doctor, and the hospital where you got it. Be sure to carry this card with you at all times.
Recovery at the hospital
If you have a permanent pacemaker, you may have to stay in the hospital overnight so your healthcare team can check your heartbeat and make sure your device is working well. Your healthcare team may help you get up and walk around.
The day after the procedure, you may get an X-ray to check that the pacemaker and wires stay in place. Your team may also suggest an electrocardiogram to look at your heart rhythm. They will check to make sure the device is programmed correctly for you before you leave. They may also make sure the device can send data remotely.
Recovery at home
Your doctor will give you instructions to follow as you heal at home, such as:
- What medicines to take
- When to return to normal activities. Your doctor will probably ask you to avoid driving or heavy lifting for at least a week. Most people return to other daily activities within a few days of having surgery.
- How to prevent wires from moving. Your doctor may ask you to use caution or avoid heavy lifting, intense physical activity, or lifting your arms above your head. These activities could shift the device or a wire out of place.
- When to make a follow-up appointment . Typically, the first appointment is one month after implant, with follow-up visits every 6 to 12 months.
Possible complications from a pacemaker
The procedure to place a pacemaker is generally safe. However, complications can happen from the procedure or the pacemaker itself. Talk with your doctor about the benefits and risks of a pacemaker.
Complications may include:
- Allergic reaction to the device or medicines used during the procedure
- Blood clots that block blood flow. Your doctor may give you blood thinners to reduce this risk.
- Device problems. The device may stimulate muscles other than the heart. Sometimes wires break, stop working, or get knocked out of place. Displaced wires can block a blood vessel or heart valve or poke through the heart muscle. Wireless pacemakers can also move out of place.
- Heart problems. Some people may develop arrhythmia, heart attack, or other heart problems after surgery or the device placement.
- Infection around the pacemaker wires or device. The infection may spread, causing problems in other parts of the body. Call your doctor right away if you develop a fever in the days and weeks after the procedure.
- Pacemaker syndrome, which is when the pacemaker stimulates only one ventricle. The upper and lower chambers don’t beat in rhythm and blood flows in the wrong direction. Symptoms include fatigue (extreme tiredness), difficulty breathing, and low blood pressure .
- Tissue scarring. Over time, tissue around the device can scar and stiffen, or tissue can grow around the wires or device. This can make it harder for your heart to work.
- Trapped fluid or air around the lungs, known as pleural disorder or possible pneumothorax, or fluid that collects around the heart, called pericarditis .

Savvy Travel Advice
Travel Health: Traveling with a Pacemaker
Last updated: August 29, 2019 - Written by Jessica Norah 42 Comments
One of our first thoughts when we heard that Ethan may have to get a pacemaker was “what are the restrictions related to traveling with a pacemaker?”.
As some of you probably know, Ethan was born with a congenital heart condition and recently had his fourth open heart surgery. While this last surgery was successful overall, a complication of the surgery led to Ethan having a prolonged stay of 3 weeks in the hospital and the insertion of an internal pacemaker. A pacemaker is essentially an implanted medical device that uses electrical impulses to regulate the beating of the heart to treat disorders that cause the heart’s rhythm to be too slow, fast, or irregular.
Interestingly a search of the Internet turned up only a handful of articles related to traveling with a pacemaker and we wanted to share what information we discovered based on our research and discussion with medical professionals about this issue. While we specifically will focus on issues related to traveling with a pacemaker, much of this information may also be helpful for those wanting to travel with other heart-related implantable devices such as cardiac resynchronization therapy (CRT) devices, implantable cardioverter defibrillators (ICDs), and insertable cardiac monitors.
We’ll share tips and advice related to travel with a pacemaker and also Ethan’s own personal experience and thoughts on flying and traveling with his new pacemaker.

Table of Contents:
Traveling with a Pacemaker
One of the great things we discovered about pacemakers is that the technology for these devices has come a long way since their initial invention. They are smaller, last longer, and cause fewer disruptions in one’s daily life than ever before. Generally, traveling with a pacemaker is safe and there are few, if any, travel-related restrictions.
The two primary concerns are generally related to either electromagnetic compatibility (electrical devices that could interfere with the functioning of the device) and activities that could potentially cause rough physical contact at your pacemaker site and damage the device. Most potential travel problems with a pacemaker can be avoided by being prepared before your trip.
** Disclaimer : Neither of us are physicians or experts in cardiac devices and these are not medical recommendations. This advice and all thoughts in this article are simply tips we discovered in our own research on travel and pacemakers. Please consult a trained health care professional for any concerns you may have about traveling with your cardiac device.**
Set Up an Appointment with your Doctor Prior to Your Trip
It is generally recommended that you set up an appointment with your doctor before you leave for a trip to have your device tested, talk about any specific care or activity recommendations, find out what to do if you do happen to experience any discomfort or symptoms, and find out how to access emergency services while at your travel destination.
If you plan to engage in any recreational activities that you might be particularly concerned about (e.g., SCUBA diving, ziplining, bungee jumping, shooting a gun), you should ask your doctor specifically about these activities to make sure they are safe. Some of these activities may not be recommended for someone with a pacemaker and/or cardiac issues.
If you will be traveling with others, you should also share any relevant information with them in case of an emergency so they know what to do.
While you may have few, if any, travel restrictions related directly to your pacemaker, there may be concerns related to your underlying heart condition, medications, or other medical conditions. If you have any concerns, ask your doctor.

Register and Gather Information about Your Pacemaker
After you get your pacemaker, you or your health care professional likely completed either a paper or online registration for your pacemaker. If you have not yet registered your device with the medical device company, do this now and make sure you get an ID card for your pacemaker.
If the manufacturer does not offer an official ID card or you don’t have time to get one before your trip, you can download this Pacemaker ID card template from the American Heart Association and fill in your information.
If traveling internationally, you might also want to get an international travel ID card, such as this one from Medtronic.

Make sure you know the pacemaker manufacturing company, device type, model and serial number, and emergency contact information of your doctor who is familiar with your pacemaker. Most of this information should be on your patient identification card along with your home contact information, but if not, find it out and keep it with your ID card.
Also, if any of the above information changes, such as you get your pacemaker replaced, you change your doctor, or your contact information changes, please be sure to get an updated ID card.
Review the Activity and Device Restrictions Related to Your Pacemaker
After your pacemaker was inserted, you likely received information from your doctor about any restricted activities and a list of devices that have electromagnetic fields that you should avoid close contact with as they may interfere with the working of your pacemaker.
You should review this information prior to traveling as while these things may not be concerns in your current daily routine, people often engage in activities and interact with devices while traveling outside of those they normally encounter.
Some common things that may interfere with pacemakers are electromagnetic devices like anti-theft metal detectors and airport security screening systems and activities like SCUBA diving.
Here are two useful lists about potential restrictions and recommendations: a list from Medtronic of items and activities that might interfere with a pacemaker and these guidelines from the American Heart Association .
However, given that all models and devices may have slightly different restrictions, you should also consult information from the patient manual for your specific device or request this information from your doctor or the device manufacturer.
Pack all Relevant Information about your Pacemaker
- Make sure you travel with your pacemaker ID card and have an emergency contact phone number to call if you have questions or issues about your device (make sure it has a number that will work internationally if traveling abroad).
- Get a list of local medical facilities at your travel destination that support your device. You may be able to find this online as we did (Medtronic lists clinics in over 120 countries that support their devices) or you might need to talk to your health care professional or device manufacturer. You can find locations that support Medtronic devices worldwide here .
- If you are concerned that airport security personnel or medical personnel at your travel destination may not speak English, you should consider getting an international pacemaker travel card (such as this one from Medtronic) or bring along a document in the local language that gives information about your condition and implanted device. Generally, this will not be necessary as most people will understand from the medical symbols on your card, but it is always good to be prepared especially for those going on extended trips.
- It is a good idea to have back-up copies of all your pacemaker information and medical contact numbers. You might consider stowing back-up copies in your luggage, giving a copy to a travel partner, leaving a copy at home with a family member or friend, and/or sending a digital copy to your e-mail.
- If you have a medical bracelet or necklace, you’ll want to make sure you are wearing it during your trip.
What You Need to Know about Airport Security Screening Procedures and Other Security Screening While Traveling
Airport security screening procedures and similar security screening you might encounter at other places when traveling (e.g., embassies, museums, government buildings, etc.) are unlikely to affect the functioning of your pacemaker.
However, do check for any signs near the screening about pacemakers or implanted heart devices such as the one below which we recently saw in a Paris museum and if you see it, be sure to follow the instructions. Normally if you see a sign like the one above, you’ll just need to tell the security person and they will do a physical screening and let you bypass the screener.

However must scanners are safe for pacemakers. Before walking through an airport security gate, you can let security personnel know you have a heart device, and show your identification card. Then, walk through the archway at a normal pace and move away from the system if you feel any dizziness or rapid heartbeats.
Similarly, if you are at an airport that uses the newer security systems where you step onto a platform and stand in a certain position, just follow the procedure and step away from the security apparatus as soon as you are screened.
Airport security systems are metal detectors, so the alarm may sound when it detects the metal case of your heart device. Don’t worry, just show your pacemaker ID card. If airport security uses an electronic wand to clear passengers, ask the security attendant to avoid placing or waving the wand back and forth over your implanted heart device. We did not come across any warnings about pacemakers and actually flying in an airplane.
Note that is you feel uncomfortable going through a security screening device, you can always ask to be patted down manually by staff rather than go through the screener. Once it is your turn, you should show them your pacemaker card and ask for a manual screening.

Ask Before Engaging in any Activity you are Unsure about While Traveling
If there is something you are planning to engage in during your travels that you are unsure about, consult a health care professional, or if that is not possible, ask the staff at that particular place. Before you go diving or ziplining, ask to make sure the activity is safe for someone with an implanted cardiac device.
Also, if you are planning to visit a science museum, physics laboratory, technology center, or some other place that might contain devices with particularly strong electromagnetic fields, you should ask at the site to find out if there are any exhibits you should avoid or activities you should not participate in that might interfere with your device.
Inform All Health Care Professionals About Your Pacemaker if you Need Medical Treatment While Traveling
If you need medical treatment, even a simple dental treatment, while traveling please make sure you inform the treating health care professionals that you have an implanted pacemaker and show them your pacemaker ID card. Certain medical procedures (e.g., therapeutic ultrasounds, electrosurgery, computerized axial tomography [CAT or CT] scans, and magnetic resonance imaging [MRIs]) may be unsafe or precautions may need to be taken in order to not cause potential damage to your pacemaker.
Each device may have different precautions and it is good to discuss these with your doctor before you travel so you are informed, but competent health professionals in any country should be aware of these precautions. You just need to make sure that they are fully informed about your device and any medical conditions.
Ethan’s Own Thoughts on His First Time Traveling with a Pacemaker
A s Jess noted, I was born with a congenital heart condition and have undergone multiple heart operations. During my most recent operation, I had a complication that resulted in me needing a pacemaker.
I really was hoping I would not get a pacemaker as I was afraid of the restrictions, but I didn’t end up having a choice. I was initially concerned about everything from having my cell phone too close to my chest, operating the microwave, and even wearing my seatbelt too tight.
I was particularly concerned about how this was going to affect traveling with Jess. We both love to travel so much and have a big trip planned in a few months to Asia. I was thinking at one point that we might need to cancel the trip as I had no idea if I would be able to get safely through airport security, let alone what would happen if my pacemaker had issues in the middle of Cambodia!
I imagine that concerns about traveling (and lots of other activities) are normal for most people getting a pacemaker for the first time. I’ll share what I’ve done so far and how my first travel experience went with my new pacemaker.

At the hospital, my Medtronic pacemaker was registered by my doctor and I later received my pacemaker ID card in the mail. We also called Medtronic Patient Registration Services (1-800-551-5544) and requested a couple of copies of their pacemaker travel cards designed for international travel.
I also read through my patient handbook, talked to my doctor about travel restrictions, and did some online research of my own. While all of this helped some, I was still nervous when I took my first flight after my surgery.
I traveled alone to visit my family in Albuquerque, NM about two months after my surgery. When I got to the airport in San Francisco, I got up to security and told the TSA agent I had a pacemaker. I was informed that the scanner machines are safe to go through with a pacemaker.
Even though I was still a bit doubtful and a little worried, this being my first time traveling with the pacemaker, I walked through and was able to get through security with no problems! I didn’t feel any strange sensations or have any complications.
Coming back home, I went through the Albuquerque airport security. Here they actually had some people going through a different type of metal detector, and I was one of those people. So needless to say I thought for sure that I was going to have problems here.
Again I informed the agent that I had a pacemaker but he, not so kindly, directed me to walk through and again I had no issues. The machine did not go off and everything went smoothly. I think that being so young, security people may or may not believe that I actually have a pacemaker.

The uneventful trip to Albuquerque and back definitely made me feel safer about traveling as the airport security detectors were the thing I was most worried about. However, another one of the fears I have while traveling overseas is the language barriers and not having good access to medical care if something went wrong. In the U.S. I don’t worry about this very much, but I do have to say that I am concerned about this for international travel.
In preparation for our upcoming trip to South Korea, Cambodia, and Vietnam, Jess has already looked up the lists of clinics that support my Medtronic pacemaker and there is only one clinic in the entire country of Cambodia. This was a bit concerning.
While it is unlikely that I will need medical services while there, it will likely remain a small worry in the back of my head during our trip. I do plan, however, to get a medical ID bracelet or necklace to feel a bit safer. But I no longer have any thoughts of wanting to cancel our trip. I look forward to a life full of future travels and I can’t let my worries keep me at home.
As I was telling my doctor recently, I am still working on trusting my pacemaker. I am slowly trusting it more and more and worrying less that it is just going to stop working. I try to remind myself that millions of people have pacemakers and many people travel with pacemakers with no troubles every day. I think it is normal to worry, and this worry can be used to make sure we are prepared to travel rather than keep us from enjoying our lives.
If you have questions about traveling with a pacemaker or want to share your own experiences, we’d love to hear from you. Just leave us a comment below!
Share this Post!
There are 42 comments on this post.
Please scroll to the end to leave a comment
Brian McLeod Post author
August 28, 2019 at 5:49 pm
Hi Jessica and Ethan I just wanted to share my experience with my pacemaker. I have had it for nearly a decade and recently had to have it changed so I can now have MRI’s (due to another medical condition – Technology has come along way!). I have had many travels abroad and short flights here in Australia. I always err on the side of caution and ask to be patted down unless they have the body scanner where you place you hands above your head). But I know that is not necessary, its just something I have made a habit of and I usually get through quicker to be honest. I have my Medtronic ID card , but was not aware of the international one , so I will contact the company and get one of those. I have never had to show the one I have now as you can see the pacemaker anyway. I just wanted to thank you both for all of this information, and assure those that are concerned about travel not to be. It has not affected my life at all. My wife and I are off the USA next year, and I have no concerns at all. It was scary at first but is one of those things you just get used to.
Jessica & Laurence Norah Post author
August 29, 2019 at 3:44 am
Thanks so much for sharing your own story about fears and traveling with your pacemaker. I am sure this will help future readers.
I do think that it is just one of those things that takes time to feel comfortable doing as it took Ethan a few flights to feel like “OK, this is OK, nothing bad is going to happen, I just need to be cautious”. I think that yes, you just need to be prepared, talked to your doctor, and be cautious when going through security.
Yes, the international card is a good one to have, especially if traveling to or through countries where you are likely to encounter security staff that may not speak your language. It is probably much easier for you since you can see the pacemaker, with Ethan it is internal and not visible. I also think for him, since he was in his late 20’s when he got it, it often surprised people that he had a cardiac medical device so the ID card and international card could be helpful.
Happy travels!! Jessica
Patricia Allen Post author
July 4, 2019 at 10:12 am
I have a pacemaker and I’ve had it for about a year with no problems. I am going from Florida to New York for about one month stay. Do I need to take the machine that is plugged into my telephone line at home. I’ve gotten various answers about this and I’m confused. Thank you for your help
July 4, 2019 at 11:53 am
Hi Patricia, I would ask your doctor since you are going for a month. It probably depends on how often you need to send your data to your doctor. If you need to send data more than once a month, then your doctor may advise you to take it along so you can continue to send along your data for your doctor to monitor. If not, I would ask your doctor to see if it is necessary as it sounds like you have not had any issues so you may be able to just leave it at home.
When going through any security metal detectors or screeners, be sure to let staff know in advance that you have a pacemaker. Most airport machines won’t interfere with a pacemaker but you want to go through them quickly. At some museums, they may have signs asking those with pacemakers to step out of security to avoid metal detectors.
Wishing you a great trip to New York.
Best, Jessica
Susan Cox Post author
February 6, 2019 at 9:45 am
Hi I had a pacemaker 14 months ago I’m hoping to go to Australia later this year or early next year but someone said that i wouldn’t be able to do a long haul flight is this true? I’m fine after having my pacemaker and haven’t had any problems with it. Thanks in advance x
February 6, 2019 at 9:50 am
Hi Susan, Normally after a successful pacemaker surgery you should be able to fly soon after surgery. The issues as noted in this article tend to be more about security screening (e.g., X-ray machines) than about the flight itself. However, you should schedule an appointment with your doctor or cardiologist to confirm that there are no health concerns and any precautions you may need to take with your device.
I would not listen too much to the “someone” unless that “someone” is a medical professional with knowledge of your condition as there is a lot of inaccurate information out there.
Hope this helps! Jessica
Ashley Turns Post author
October 11, 2017 at 3:05 pm
My father is going to have a pacemaker put into his chest soon since his heart hasn’t been doing so well. Since they will be going to Paris for their thirtieth wedding anniversary as well, my mom has been wondering what extra precautions they’ll need to make or what other items they may need to pack with them as well. So thanks so much for talking about how my dad should be sure to bring his pacemaker ID card with him along with an emergency number he can call about questions. I’ll definitely make sure that he will also be able to contact the phone number on his pacemaker card internationally since they will be in Paris.
October 12, 2017 at 2:49 am
Hi Ashley, Sorry to hear that your dad’s heart is not doing well but hopefully the pacemaker can help and provide some assurance. It is great though that you can still travel with a pacemaker and there are only a few limitations. Yes, having the ID card, numbers, and knowing the locations of clinics/hospitals that deal with his particular device are some of the key things I’d suggest. Also some of the X-ray scanners in Paris have signs not to go through if you have a pacemaker or heart implant – the airports should be fine but security lines at some attractions may have warnings posted (the image should make it obvious even if your parents don’t read French, see example in the photo in the article which is from the Musee d’Orsay). In those cases, your parents should just show their card to the security person and they will probably do a physical search and then let him bypass the scanner. Wishing your father a successful surgery and your parents a wonderful trip to Paris. Best, Jessica
Susan Post author
August 7, 2017 at 4:32 pm
Is there a problem if you lift your carry-on baggage in the overhead baggage area? I have read if you lift anything heavy and put your shoulder over your head could cause the lead to maybe get caught.
August 7, 2017 at 8:37 pm
Hi Susan, Generally after you’ve first had a pacemaker inserted (or a new placement) you will generally be asked by your doctor not to lift your arms above your shoulder for a certain amount of time (e.g., 2 to 6 weeks) and also not to lift anything too heavy (perhaps over 10 lbs) so everything can heal. Your doctor should give you specific recommendations, and I would definitely follow that advice. After the initial healing phase, there are normally not too many restrictions. Ethan was not given any restrictions to lifting after the initial healing period and I have not hear about the leads getting caught before, but everyone is different and different devices have different restrictions so I would follow whatever professional medical advice you received from your doctor. If you do need assistance when traveling, I would just ask a travel partner or airline steward to help you with your luggage. Also if your doctor advises not to lift your arms over your shoulders, you may need to tell the airport security as the newer airport screening scanners in the U.S. often has you raise your arms and they can have you walk through a traditional scanner instead. Wishing you happy and safe travels! Best, Jessica
Jill Post author
February 13, 2017 at 9:26 pm
Thank you so very much Jess for your support & advice. Jill
February 13, 2017 at 2:18 pm
Thank you very much for your prompt response. It’s very much appreciated and will seek an international Medtronic card asap. I just have to focus on being mentally positive to travel once again. Thank you once again Jessica.
February 13, 2017 at 4:19 pm
Hi Jill, Fear is a powerful thing and I think we all struggle with it keeping us from doing things we want to do. Don’t forget to also rely on those around you, like your husband as it sounds like he’ll be traveling with you and will be around if anything should happen. It took Ethan a long time to trust his pacemaker but he now travels without much fear compared to his first trip in which he was very anxious. Sometimes it just takes some time. Best wishes and happy travels, Jessica
February 13, 2017 at 5:20 am
Hello. I’m a 66year old female & had a pacemaker inserted May 2016 after having an ablation plus medication to resolve the problem being atrial fibrillation (irratic heartbeat). My husband & I are contemplating a trip to Spain, Portugal & Morocco in May. I have Medtronic ID card though not an international card at this point in time. To be honest I’m very anxious about travelling this distance (14 hour air time first leg of journey then a further 8 hour flight to Spain). I have travelled a short flight (1 /20mins) in January confidently however feel unsure about a long tiring trip. I have checked that a Medtronic facility is available in Spain but worry about the length of time it would take to receive treatment should that be the case. I so desperately wish to travel again overseas but can’t help feeling anxious. My cardiologist & GP say I’m fine to travel but I’m still concerned everything will be ok particularly at the airports etc.. your input would be gratefully appreciated. Than you
February 13, 2017 at 5:38 am
Hi Jill, Thanks for taking the time to comment and I think being anxious about such a long flight is normal for people with any medical condition. I am not a MD so I can’t provide you any medical advice, but it sounds to me that you have already sought sound medical advice from both your GP and cardiologist, so it sounds from a medical standpoint there are not any major concerns. It might also make you feel better to know that airlines (at least in the U.S.) are required to carry automated external defibrillators (AEDs) and enhanced emergency medical kits (EMKs) on all domestic and international flights and flight attendants receive basic emergency medical training. I would of course do all the preparation you can such as applying for the Medtronic International travel card, getting a check-up before you go, and documenting the Medtronic facilities in the countries you are visiting just in case. If your anxiety gets worse, you may also want to talk to a counselor or therapist to have someone to talk to about your worries; however, I think that your feelings are perfectly normal. I hope that you can work through your anxiety to continue doing the things you would like to do, such as traveling. Best of luck, Jessica
jresquival Post author
February 7, 2017 at 5:20 pm
That’s a good tip to visit your doctor before you travel. That way you can know if you’re healthy enough to travel and if there’s anything to pay attention. My family is flying to Hawaii with my grandma but first we have to make sure if she’s safe to fly.
February 7, 2017 at 7:39 pm
Hi J.R., Thanks for taking the time to comment and I hope your grandma comes away from the doctor’s visit with a clean bill of health to fly. In most cases, a pacemaker will not stop one from being able to fly. Enjoy Hawaii! Best of luck, Jessica
Jill Edin Post author
January 29, 2017 at 5:18 pm
Hi there – thank you for your interesting and useful advice. We are travelling for a 10 day holiday to Bangkok and Koh Samui – I have a pacemaker/defibrillator implant. Have you been there?
January 30, 2017 at 3:51 am
Hi Jill, I am I have not personally been to those places in Thailand (or more importantly Ethan has not), but I think the situation will be very similar to our experiences in other SE Asian countries we’ve visited. Ethan has traveled and flown a lot with his pacemaker without any issues in North America, Asia, and Africa. I think all the info from the article should apply and I would first start by consulting with your doctor, get an international pacemaker card to carry with you, and then find out where clinics/hospitals that are set up to handle your particular pacemaker/defibrillator implant will be located near the locations you are visiting (just in case of emergency). I think gathering information and being prepared is the best thing you can do and in most cases, having a pacemaker implant should not affect your holiday plans! Have a great trip Best, Jessica
Anonymous Post author
August 1, 2016 at 2:03 pm
Hello! My husband may need to have a pacemaker inserted this week, but we have a vacation planned a week from tomorrow. How was your recovery? All websites indicate a 48 hour recovery time and that flying should be no problem, but I’d love to hear first hand how you felt. Do you think you would have felt comfortable enough to go on a vacation with Jess being only a few days out of surgery? Looking forward to hearing your feedback. Thanks!!
travelcats Post author
August 2, 2016 at 4:12 am
Hi there. I was in the hospital for a number of days after the surgery (I had also just had open heart surgery) so there was no way I could have flown 48 hours later. But the main recovery time for just a pacemaker insertion surgery is only 2-3 days and normally patients are just in the hospital for 1-2 days. I flew about 2 months after my pacemaker surgery but on my last heart surgery I flew about 2 weeks after it. However, there could of course be complications and some folks do have more pain than others, and people also sometimes have more anxiety over it than others and may not feel comfortable flying so quickly. I think it is probably safe as long as your doctor says so but I would listen to whatever your husband feels on the matter after his surgery. If he feels fine going forward, then I would go ahead with it. For the trip, just be sure to have the pacemaker ID card and information on clinics at your travel destinations with you as well as any medical bracelets and medication he is taking. I would also be prepared to postpone the vacation if needed (if you can get travel insurance that would be great) as it will not be fun for him if he is feeling pain or a lot of anxiety. It make take him a bit longer to feel comfortable with flying but if you do need to cancel, I’d just be sure to reschedule the vacation. Taking some time to get comfortable and feel safe is one thing, but you don’t want a pacemaker to prevent you from living your life! I wish your husband the best and hope that the surgery (if needed) goes smoothly and wishing him a quick recovery and that you both have a great vacation (whether it is next week or next month). Happy travels, Ethan & Jessica
August 2, 2016 at 8:59 am
Thank you so much for your prompt response, much appreciated! Great idea to look for local clinics along the way–I’m sure that would alleviate some of his anxiety!
August 2, 2016 at 10:02 am
You are very welcome! Yes, you should be able to find this information through the device manufacturer. In the article we provide a link to search for those clinics that can provide support for Medtronic devices which is Ethan’s pacemaker manufacturer, but if you have a different manufacturer, you should be able to get similar information from the company. ~ Jessica
Liz Post author
May 18, 2016 at 5:03 am
Hello! I am also new to this card-carrying pacemaker club (in fact only one week ago!) The entire experience was terrifying and somewhat unexpected. I am very thankful for posts like yours, that are matter of fact, and strangely soothing. Your post helped me to feel as though maybe I don’t have to be afraid of everything, rather just how to deal and move on. Thank you!
Sincerely, Liz
May 18, 2016 at 5:40 am
Hi Liz, Thank you so much for taking the time to leave us a comment. Ethan’s pacemaker was also very unexpected as he went into heart block due to a complication of his surgery which was not expected. However, I think he has learned since that experience that it is still possible to do almost all of the things he did before. He has flown domestically and internationally, traveled through S. Korea, Cambodia, and Vietnam, did a week’s safari in Africa, and climbed to the summit of Mount Kilimanjaro. In terms of traveling, the major things we think are to talk to your doctor prior to travel, be cautious at security screenings, keep a card about your condition and pacemaker on your person (get an international travel card if you travel abroad), and know where the nearest medical clinics that work with your pacemaker are located when traveling abroad just in case there are any problems. I think that it takes time but Ethan has come to trust his pacemaker and feels much less afraid of being active and doing most of the things he did before his surgery. Best of luck to you! ~ Jessica
Blake Mills Post author
June 15, 2015 at 12:59 pm
I am 30 years old and recently had a pacemaker implanted to correct my AV block that was causing issues with normal rhythm. I still have some irregular beats, but those are PVC’s as told me by my rhythm specialist. We are getting ready to fly to BOston for few days and after reading this, I’m much more comfortable. I”m having trouble “trusting” my pacemaker as well!
June 18, 2015 at 11:36 am
Hello Blake, I am glad to hear experiences and thoughts from others with heart conditions. Yes, you can climb mountains and travel and it can be really smooth and easy as our article talks about. It is just good to be prepared before trips just in case something happens, it gives you that sense of safety. I also had trouble at first trusting my pacemaker, but now I feel much more comfortable with it and think of it as a great back-uo if nothing else. I hope you all are doing well and if you have any questions or concerns feel free to email me at ejh2323 (at) gmail.com ~Ethan
AMIT BANERJEE Post author
January 26, 2015 at 6:05 pm
I got PPI on 10th May 2010 at Apollo Hospital, Sarita Vihar, New Delhi INDIA. My birth year is 1954. I will be traveling for London on January 29th and back on February 6th. 9 day trip. Please guide me whether I can avail travel insurance or not. Amit Banerjee
January 28, 2015 at 1:23 am
Yes, you should be able to purchase international travel insurance from India that will provide medical coverage within the UK. You should carefully read the policy or talk to the insurance agents about what kinds of care are covered and what cost, if any, you would incur in different medical situations.
Good luck and safe travels, Jessica
having oxygen while traveling Post author
December 2, 2014 at 8:48 pm
Some people need also oxygen tanks when traveling which is really important for them. Special permits must be acquired for safe journey.
December 4, 2014 at 7:19 pm
Thanks, I am not very familiar with oxygen tank policies as neither of us have needed them thankfully but thanks for the tip which may apply to other readers.
Edith Bosire Post author
June 10, 2014 at 12:27 am
Hey Travel Cats,
I just came back from China last week and it was my first long haul flight since my pacemaker implant in 2012. Since that date whenever I travel I usually bypass the metal detector machines and since it has predominantly been local flights it has worked well….they let me pass on the side fo the machine in China as well but gave me a serious body search….!! I found your website while looking for something on climbing a mountain with a pacemaker….I really want to start climbing from next year and one day conquer Mt. Kenya and Mt. Killimanjaro. Your posts have been informative and inspiring…..now all I need to do is get my stamina up and excercise dilligently…while eating healthy. THANK YOU!!
June 10, 2014 at 12:45 am
Dear Edith, thank you so much for sharing your experience with us and our readers! It can be really frightening to have to worry about pacemakers and other equipment while traveling, but so far Ethan has had no problems. We recently just returned from a trip (and about 8 flights!) from the U.S. to Korea, Cambodia, and Vietnam and Ethan went through all the screenings normally with no issues. We just got a doctor’s note that says he can climb Mt. Kilimanjaro. Now I think SCUBA diving and higher elevation mountains are out (no Mt. Everest in his future, haha) for instance, but most things are still possible! If you do a mountain climb, a few suggestions would be to talk to your doctor, be aware of closest medical facilities that can service your pacemaker, have good travel health insurance, and take oxygen (our porter is bringing this). Good for you and keep us updated!
Jenna // A Mama Collective Post author
February 14, 2014 at 9:03 pm
Thank you for putting together such a thorough and important list! I know this will be so helpful to folks traveling with not only a pacemaker, but other important health issues as well. Glad to have found you through SITS 🙂 ~Jenna
February 14, 2014 at 9:56 pm
Thanks Jenna!
Meghan Post author
February 1, 2014 at 1:08 pm
It’s so easy for those of us without physical restrictions to forget about the challenges many people face while they travel. Thank you so much for sharing! It’s great to hear that advances in medicine and awareness are making it easier for everyone to travel.
February 1, 2014 at 4:09 pm
Meghan, that’s so true. Before Ethan’s last surgery neither of us really had any travel restrictions even with his heart condition. But now we have to do a bit of research into each destination we travel to know what to do if something did happen to go wrong and consult with a doctor before doing certain activities such as SCUBA diving or our upcoming charity climb of Mt. Kilimanjaro. But overall it is not a big adjustment and I think there are ways for most people with health conditions to travel, as long as they know their restrictions and plan ahead of time.
February 5, 2014 at 9:08 am
It’s so great to hear that it doesn’t significantly restrict you. With the internet, it’s so easy to research destinations in advance. Just another way technological advancements are improving travel!
Karla Smith Post author
January 22, 2014 at 7:27 pm
My husband has a pacemaker and I actually was never clear about what travel restrictions he may or may not have. Honestly, I thought it would be quite complicated for him to fly and go through airport security so it is nice to read about Ethan’s experience. This makes me feel less nervous if we need to take a flight in the future.
January 28, 2014 at 9:40 pm
Hello Karla, glad this information was helpful to you! I hope that this info will make things easier if your husband does fly in the future.
Louisa Post author
January 20, 2014 at 1:59 am
This is such an interesting post as my youngest brother was born with a hole in his heart and may end up having to have a pacemaker. He probably hasn’t thought about travel so this is potentially useful for him.
January 20, 2014 at 12:11 pm
I am sorry to hear that your brother may need a pacemaker, but it is good to know that there are generally few activity restrictions. Feel free to share this with him.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Notify me of replies to my comment (just replies to your comment, no other e-mails, we promise!)
Subscribe to our monthly Newsletter where we share our latest travel news and tips
We only ask for your e-mail so we can verify you are human and if requested notify you of a reply. To do this, we store the data as outlined in our privacy policy . Your e-mail will not be published or used for any other reason other than those outlined above.

Heart Sisters
For women living with heart disease
How soon are heart patients safely fit to fly?

by Carolyn Thomas ♥ @HeartSisters
Five months after my heart attack, I boarded a plane from the West Coast bound for Rochester, Minnesota. Considering that I’d suffered two terrifying cardiac events on another long flight just five months earlier made this trip just a wee bit scary for me.
Only the reality that I was headed to the world-famous Mayo Clinic helped to propel me onboard. I told myself that if anything happened to me and my heart during this flight, the board-certified cardiologists at the Mayo Women’s Heart Clinic would know exactly what to do for me. If I survived the flight, that is . . . . .
Like many freshly-diagnosed heart attack survivors, my fear of having a heart attack on a plane was very strong. (Note: many survivors experience a very strong fear of having another heart attack just walking down the street).
So being strapped into a metal box 35,000 feet up in the sky, hour after endless hour, inhaling stale air, in a pressurized germ-infested environment, with reduced circulating oxygen levels in my blood, risking the onset of hypobaric hypoxia , and with no guarantee at all that my seatmate would be a board-certified cardiologist seemed just plain crazy.
But apparently there is good news about heart patients and flying from the British Cardiovascular Society.
Most people with heart disease who are not critically ill can safely fly on commercial aircraft, according to a U.K. report. (1) Lead author Dr. David Smith (Royal Devon and Exeter NHS Foundation Trust) told H eartwire:
” The overwhelming conclusion is that the cabin environment poses very little threat. It’s not the flying that’s the problem for heart patients, but the stability or instability of someone’s underlying condition that indicates the probability of a spontaneous cardiac event occurring while they are in the air.”
The passengers who might feel some minor physical effects of low blood oxygen (hypoxia) include those already at risk of:
- myocardial infarction (heart attack)
- heart failure
- abnormal heart rhythms
But according to Dr. Smith, the blood oxygen levels induced by flying “ appear to have little or no adverse circulatory effects, certainly not for short- and medium-haul flights.”
However, some heart patients at high risk are advised to “ defer travel ” until their condition is stable, including those:
- having an ejection fraction <40%
- showing signs and symptoms of poorly controlled heart failure
- with unstable angina or uncontrolled arrhythmias
- awaiting further investigation, revascularization, or device therapy
And here’s how soon after a cardiac procedure you are generally safe to fly:
- After uncompl icated elective (non-emergency) cardiac catheterization (angioplasty, wi th or without stent implants), patients can fly after a few days.
- If patients suffer from stable angina with infrequent attacks, they should be able to fly. It is safe to use nitroglycerin spray in a pressurized aircraft cabin.
- Patients with pacemakers implanted can fly after a few days, unless they have suffered a pneumothorax , in which case they should wait until two weeks after it has fully healed.
- Those with ICD s (Implantable Cardioverter Defibrillators) can fly after a few days, with the added recommendation that they should not fly after the ICD has delivered a shock until the condition is considered stable again.
- Those who have experienced a heart attack (myocardial infarction) can fly after 10-14 days. If you are older than 65 or if you’ve had another heart attack in the past, you’re statistically more likely to have one again. The U.K. Civil Aviation Authority recommends that i f you have no symptoms or other heart conditions and no further cardiac treatment is planned, you’re considered to be at low-medium risk to fly. But if further cardiac treatment is planned, you’re considered to be at higher risk of another heart attack – best not to fly at this time.
- Those who have had heart valve repair or replacement surgery or coronary artery bypass grafts ( open heart surgery ) can usually fly after 4-6 weeks (longer if they have had pulmonary complications).
Generally speaking, if you can walk briskly for 100 metres on the flat without being breathless or in pain, you can fly.
But even when your physician has officially given you the green light to fly again, remember that severe fatigue can continue to be a serious issue for heart patients long after the other physical effects of cardiac procedures have healed.
Anticipating this fatigue may influence your decision, for example, to request an airport wheelchair or a ride to connecting gates on the airline golf cart, and to limit the weight and size of your carry-on bag. Please plan ahead and arrive at the airport significantly early for any flight to minimize rushing or stress.
The anxiety surrounding air travel can be debilitating even for non-heart patients. If fear of flying has ever been a serious issue even before your own cardiac event, it may indeed feel worse now. If you really must fly, ask your own doctor about managing this anxiety before your flight.
Long flights can mean crossing time zones, sleep deprivation and jet lag. Probably the most important effect of changes in sleep patterns for passengers with cardiovascular disease is the potential disruption in taking daily medications. It can be difficult to stick to a normal meds routine when that routine is altered, especially if we’re confused about what time it really is. The U.K. report warns that it’s especially important for passengers with stable heart failure, angina or arrhythmia to maintain the regularity of their medications.
If you’re planning an out-of-country flight in the near future, remember that most major insurance companies will not provide travel medical insurance earlier than 90 days after a cardiac event, or even after a change in your medical treatment. In some cases, just a doctor’s appointment in the past 90 days at which your medication dosage is changed (either increased OR decreased) can mean your condition can be considered “unstable” and thus grounds for denial when you file a travel medical insurance claim.
Each airline has its own policy for allowing flying passengers after a cardiac event – and as you’ll see from the Oregon heart patient’s experience with Alaska Airlines (described below), some of these policies appear to defy accepted medical guidelines. So call both your insurance broker and the airline before you book a flight to double-check all details relevant to your own travel and clinical circumstances.
For heart patients who sport implanted medical devices, it may be comforting to know that the amount of metal used in most implanted heart devices like pacemakers, heart valves or ICDs is very small, according to cardiologists at St. Jude Medical. It is usually not enough to set off airport security metal detectors ; if it does, simply show security personnel your patient identification card. Passing through a metal detector should not hurt your device. However, do not linger near the security system arches or poles.
Dr. Clemens Jilek and his team of researchers from the German Heart Center in Munich recently did a study on 388 heart patients, published in the journal Annals of Internal Medicine . They concluded that metal detector security screening appears safe for those with pacemakers or ICDs implanted.
What about those new full body scans at airport security gates and people with implanted pacemakers or ICDs? According to cardiologist Dr. Richard Fogoros , there are few if any controlled clinical studies or even written information about the safety of these full body scanners for heart patients:
“I called the technical support departments of two major pacemaker manufacturers. I was told that they regard the full body scanner as completely safe for those with implanted pacemakers and ICDs, and this is what they tell patients and doctors when they call for advice (which apparently they do frequently, since there is no written advice anywhere). I was told that:
- 1) their engineers have determined it is extraordinarily unlikely that these scanners are capable of negatively affecting implantable medical devices
- 2) many thousands of people with pacemakers and ICDs have used total body scanners over the past several years, and there has been no allegation of any problems.
“So, both engineering theory and a large volume of real-world experience indicates they are safe, according to them.
“There is no reason to believe that a full body scanner will effect a pacemaker or ICD, and medical device companies are willing to say that verbally (but not in writing).
“If you want to wait until some authority is willing to make a definitive written statement about this, you can opt for a pat-down instead when you go through airport security. Since this issue is in the hands of bureaucrats, however, don’t hold your breath waiting for a resolution.”
A serious health problem you may have also heard linked with air travel, particularly long flights, is deep vein thrombosis (DVT) and venous thromboembolism .
Although a long-haul flight doubles the risk of DVT, it is actually similar to that incurred during car, bus, or train travel for a similar period, the U.K. researchers state. And the absolute risk of DVT for a fit and healthy person is one in 6,000 for a flight of more than four hours, they note, pointing out that pilots are at no greater risk than the general population, a statistic that is not particularly comforting.
Now I have to worry not only about myself, but about my pilots. Why not take the advice of my heart sister Jaynie, who always harps at us to wear compression knee-high stockings while flying?
There are some recommended common sense flight precautions for those at risk of DVT:
- consume plenty of fluids
- exclude caffeine and alcohol
- wear compression stockings
- take a dose of low-molecular-weight heparin (a blood thinner)
- wear a MedicAlert bracelet or dogtag necklace at all times
- talk to your doctor to confirm that your cardiac disease is stable
- carry adequate supplies of all prescribed medicine
- carry a copy of your medical history
- carry emergency phone numbers for your doctor(s), family members and destination contacts
Having memorized these precautions, you might want to also consider the alarming case of one Oregon heart patient who describes her “very interesting flight” to Rochester, Minnesota to see cardiologist Dr. Sharonne Hayes at the Mayo Women’s Heart Clinic. Here is the transcript of her complaint against Alaska Airlines filed with the FAA:
“I mentioned to the E/C flight attendant that I carry nitroglycerin for chest pain in my pocket should I request assistance, and that it was only cautionary in nature because I was traveling alone. “The Head Flight Attendant ordered me off the flight because she ‘assumed’ that I was unhealthy. She required me to provide a doctors’ note clearing me to fly. She informed me that the FAA allows flight crew to decide who is fit to fly or not, and they can remove whomever they feel is unfit to fly. “Alaska Airlines customer services representative and flight attendant refused to speak with my cardiologist who was wakened at 6:30 a.m. on a Sunday morning because I did not have the “requested” doctor’s note. “I explained that the flight crew had no data to support their assumption that I was unfit to fly, nor did they request the other passengers to produce doctors’ notes. “Alaska Airlines discriminated against me based on the fact that I carry nitro in my pocket. They created a very stressful environment and threatened to impair my ability to seek medical care at the Mayo Clinic. They humiliated me in front of a plane full of passengers. “An air carrier may not discriminate against an otherwise qualified individual on the following grounds: 1) the individual has a physical or mental impairment that substantially limits one or more major life activities. 2) the individual has a record of such an impairment. 3) the individual is regarded as having such an impairment.”
(1) Smith D, Toff W, Joy M, et al. “ Fitness to fly for passengers with cardiovascular disease. The report of a working group of the British Cardiovascular Society “ . H eart 2010
COVID-19 UPDATE 2020: “ S hould I avoid plane travel just to be safe?”
“ Planes tend to be low humidity, but the air’s actually pretty clean. It gets re-circulated through these HEPA [high-efficiency particulate air] filters that really are very good at clearing stuff out,” said Dr. Vicki Hertzberg , a biostatistician at Emory University, who co-led a study on flights and disease transmission with scientists at Boeing. “Also, they suck in about 50% clean air with every re-circulation. So in some aspects, the air on a plane is cleaner than what’s going on in your new office buildings.”
Remember that Dr. Hertzberg’s advice applies only to passengers while the plane is in the air. As soon as that aircraft lands, passengers exit the plane and are no longer protected by HEPA filters while walking through the airport, or waiting at the baggage carousel, or shopping or dining in the airport, or getting onto airport transportation vehicles.
NOTE FROM CAROLYN: I wrote more about my fateful five-hour flight in Chapter One of my book, A Woman’s Guide to Living with Heart Disease . You can ask for it at your local library or favourite bookshop, or order it online (paperback, hardcover or e-book) at Amazon , or order it directly from my publisher, Johns Hopkins University Press (use the code HTWN to save 30% off the list price).
Like this? Share it with others!
- Click to email a link to a friend (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to print (Opens in new window)
- Click to share on Pocket (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to share on Mastodon (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on Tumblr (Opens in new window)
Published by Carolyn Thomas
View all posts by Carolyn Thomas
21 thoughts on “ How soon are heart patients safely fit to fly? ”
Very interesting . I have recently travelled from Houston to Perth. I had 2 heart stents inserted 3 weeks prior to my journey home. I have been home for 5 days now. I’m experiencing shortness of breath and nausea if I do too much.
I’m wondering if the jet lag and fatigue is the cause. I can’t do a lot as I become so exhausted.
Hello Kathleen – I’m sorry you’re experiencing these puzzling new symptoms. I’m not a physician so cannot comment specifically on your situation, but I can tell you generally that you’re still in relatively early days, post-stents. And as this post mentions, “severe fatigue can continue to be an issue for heart patients long after the other physical effects of cardiac procedures have healed.” It’s quite possible that the effects of jet lag and the travel itself are adding to that fatigue. If I were in your shoes, I’d contact my doctor just to check this out – especially if symptoms seem to be worsening instead of gradually improving.
Meanwhile, you could start a Symptom Journal ( more details here ) to track which specific activities seem to aggravate those symptoms. It’s important that recently diagnosed heart patients remain as physically active as possible – so you don’t want to stop moving or start dreading “doing too much” out of a fear of possible after-effects, but you also don’t want to be suffering!
Good luck to you! ♥
Hi Carolyn, I just some how have fallen outside of of the safety zones for flying. I was told from the point of my AMI that my heart was to weak to withstand G-force meaning flying will forever be out of range. Since then I’ve developed Supraventricular tachycardia (SVT-fast or irregular heartbeat) with episodes of SCD that won me an A-ICD (implanted defibrillator). The worse part of all is I don’t feel my SVTs, and my SCD has me going down in slow motion. I’m not allowed to move to far from where I am.
Lastly I have a stent and an A-ICD, I have set off security alarms and it does hurt. They say that we shouldn’t but my stent has set of the alarm. We were given color coded cards to carry with us when the devices were implanted. My stent is at the top of the list. In the 12 years since my AMI I’ve two long road trips. Both were 12 hour bus trips to New York. The first with the cardiac therapist and staff at the heart hospital, super safe trip. The second was with family for a weekend trip, they had to stop every three hours to slow swelling of feet and legs. Robin
This was so interesting to learn about my condìtion. And I will use the knowledge to teach others.
I am with CABG 2 months ago, I have breathing problem, can I traveling by air?
Hello Majid, only your cardiologist can answer you. The U.K. report suggests 6 weeks minimum before CABG patients fly, but longer if you have pulmonary problems. Ask your doctor – and good luck to you.
The NHS choices website also gives information apparently after discussion with the CAA. This suggests that you can safely fly 10 days after chest surgery or CABG. Clearly there is enormous variation in the advice given by different bodies.
With breathing complications like Majid describes, that 10-day suggestion may not be appropriate, which is why the best answer is to consult with her own physician.
Very comprehensive article. Thanks for this useful list of flying-related tips and facts. Now if you could just help us make the airlines run on time to get rid of those long delays . . .
Yeah, I’ll get right on that . . . 😉
Hi, I enjoyed this post. As a person who has congenital heart disease I have often faced “complications” at airports, with one particular gentleman asking what the “HUGE” scar was.. Well how rude.
I am from England and I have had lots of operations, ablations, implants, etc. But travelled a lot as I do not let it get in the way. I just would like to say that I have always brought insurance to cover myself (and family), especially for my heart, and although it costs a lot sometimes, it’s worth every penny.
Do not let it stop you travelling but always listen to your doctor too, if they say no, then go with that; save your money and go another time (she says through grumbled teeth, wanting to see her friends in America).
Great article.
That IS rude! (what’s the huge scar from? Preferred answer: How about “None of your frickety-frackin’ business!” ?!?) Travel insurance is such an important issue for heart patients as some policies will NOT cover pre-existing conditions or even incidents that follow a recent doctor’s appointment or meds change! Always read the fine print. Good luck with getting to America to see your friends!
Rude question answer, “I had my heart removed so insensitive questions like yours won’t hurt it.” But then, I am a brat! 🙂
Elizabeth Youmans RN, BSN
Like Liked by 1 person
My husband had a heart attack and cardiac arrest last week, not sure how much of the large muscle will return but hopeful, and he’s walking and breathing good. We also go abroad. Now feel worried as lots of people who have had heart attacks go, but have not seen any post re cardiac arrest. Whether this makes a difference, also been told as a cardiac arrest person it’s very difficult to get insurance, can you shed any light?
Hi Brian – The good news is that walking and breathing seem fine so far! I just went back and re-read the U.K. report mentioned in my post. You are right – nothing specifically about cardiac arrest; they seem to include that condition within heart attack criteria. Your cardiologist involved will have far more info and be able to advise both of you on the safety of international flights based on unique details of the case. Getting out-of-country travel medical insurance – regardless of cardiac arrest or any other cardiac diagnosis – is fraught with fine print designed to deny medical claims based on how “unstable” the patient’s condition is (but even a doctor’s appointment during the past 90 days at which any treatment decision is adjusted – like decreasing the dosage of a previously prescribed drug because the patient is doing better! – can suggest to the insurance company that the condition is now “unstable”). Talk to a trusted insurance broker for more info. Best of luck to you…
- Pingback: Tea&Biscotti
Hi Carolyn,
This is a very good post and one you should run every year at the start of vacation time. I said that I had been given paper work somewhere regarding travel and not to for this first year. It was clearly written in this post. When I went on my trip, they were running tests on me because of my edema. It dropped my EF (ejection fraction) down to 40% and they still haven’t been able to find out why. I also have congestive heart failure, when I talk about taking a trip I mean going outside of my state.
I went on a 12 hours-one way, and 12 hours-back home trip. I know that they had told me not to take trips without first talking it over with the doctor; this was one of those times in which I looked for someone to agree with me as opposed to following orders.
But it wasn’t an uneventful trip. I began to feel the discomfort shortly after heading back. They wanted to know if I wanted them to get emergency help, and I told them I could make it home. It was a week before I began to feel better.
I won’t make that mistake again, this is a very good posting for all of us, it reminds us of things we try to forget.
Very useful overview for those of us wondering about how soon is “too soon to fly”. Thanks for sharing this.
After I had heart surgery 4 years ago, I worried constantly about having another incident. But my most recently job had me traveling 50 – 75% of the time including many flights or long drives in the car. What my cardiologist was able to reassure me is that my continuing to control my diet, exercise and blood pressure should keep me healthy. Thanks for the article and the common sense flight precautions.
hallo there, thanks for this info on flying.I don’t have heart disease but the last time I flew, at Easter week the woman sitting next to me on the plane suffered a heart attack about 30 min out of Gatwick. The airline staff were very good, and they managed to keep her calm and the plane landed safely within a very short time and she was immed evacuated. I don’t know what happened to her after that but I can see how terrifying it might be if U are a heart patient and U are trapped in a plane. It was certainly terrifying for the rest of us to witness. Thx for your very good work here on this website. Useful and well-done.
Very excellent advice of highest quality on flying following a heart incident. My wife must fly to our daughter’s wedding in two months and already she is worried very much since her own heart incident so I’m showing to her this article. Thank you.
Your opinion matters. What do you think? Cancel reply

- Already have a WordPress.com account? Log in now.
- Subscribe Subscribed
- Copy shortlink
- Report this content
- View post in Reader
- Manage subscriptions
- Collapse this bar

- Work with Us
- Sierra Leone
- Philippines
- Bosnia and Herzegovina
- Czech Republic
- Netherlands
- Switzerland
- Paragliding
- Healthy Heart
- Food & Drinks

Adventure , Lifestyle
Steps to travelling with a pacemaker or defibrillator (icd).
Travelling with a Pacemaker or Implantable Cardioverter Defibrillator (ICD) can be an overwhelming experience. especially the first time. However, being prepared and taking the right steps will not only make your trip more enjoyable. It will put you and everyone else concerned at ease.
You can never be too careful in those moments when every second counts. When accessing your records or contacting relevant people is vital.

My story of flying with a pacemaker and ICD
5 weeks after my first pacemaker and defibrillator (ICD) insertion, I flew to Australia. So I was able to recover and spend time with my family. Apart from having a new foreign object inside my body, I also had a clot near my heart.
I had a cardiac arrest while out exercising and was rushed to ICU. They had discovered I have a heart condition called ‘Cardiac Sarcoidosis’. Then I was told I needed urgent surgery to have a Pacemaker and defibrillator. All of a sudden, everything seemed very complicated to me when it came to travelling again. Which was a little ironic because I am a travel blogger and write about travel for a living.
I just didn’t know where to start looking for the right answers. Like, can a person with a pacemaker go through airport security or how soon can l fly after pacemaker insertion .
Steps to flying with a pacemaker and defibrillator (ICD)
Knowing things like who to contact in an emergency, having the correct papers, and knowing your limits. As well as carrying the correct equipment will become a part of your everyday travelling agenda.
Here are some of the steps, I took before travelling with my pacemaker and defibrillator (ICD). I hope that they help you and are useful for your travels.
Table of Contents

1. How soon can I fly after having my pacemaker or Defibrillator ICD inserted?
They say it is best to wait an appropriate time before you start travelling or flying after implantation of your Pacemaker or Defibrillator (ICD). However, they usually say between 6 months to 1 year but it really depends on the individual and their case.
Best to consult with your doctor and have clearance before booking any type of travel or flight.
As stated earlier, I flew 5 weeks after my first pacemaker and Defibrillator (ICD) implant. I had healed quickly and my body was accepting the implant well. This made a huge difference in my case when travelling. One of the terms, before I flew to Taiwan for a month working, was to have a check-up with a local hospital. Which was an interesting experience.

Skiing with a Pacemaker or an ICD
Is it possible to go skiing with a Pacemaker or an ICD (Implantable Cardioverter Defibrillator)? Well, my answer is yes in my circumstance. [...]
1.1 Questions to ask your doctor before flying with your Pacemaker or Defibrillator
- Verify with your doctor that the underlying heart condition does not pose a risk for flying.
- Check if there is any equipment you need to take on the Plane, like the magnet to stop the ICD.
- Ask about your ID Card which you may need to show at the airport.
- See if you need to wear Compression stockings used after surgery to prevent blood clots
- Ask your doctor if your pacemaker contains any metal. Some versions do not contain metal, and they will not cause any trouble.
- Ask the doctor if there are any activities that you should avoid on your trip.
2. Pacemaker or Defibrillator (ICD) identification card
Make sure you have your Pacemaker or Defibrillator (ICD) identification card with you before you travel. If you don’t know where it is or don’t have one, ask your pacemaker clinic for a copy. As my understanding is there should be one in your file.
2.1 What is a Pacemaker or Defibrillator (ICD) identification card?
A Pacemaker or Defibrillator (ICD) identification card is an ID card that states all relevant information regarding your insertion. It lists information from the type of leads you have, the date of implantation, hospital where it was implanted to the doctor who operated.
It should even have some of your personal details like your DOB and contact number for your hospital. The ID card can also be known as the Medical Device ID Card, depending on the country you are from.
Your ID card will let the relevant people know that you have a Pacemaker or Defibrillator (ICD) implate. It will let security officials know at the airports, as well as help others know your situation in an emergency.

3. Obtain a Medical Alert Necklace or Wrist band while travelling
In an emergency, the simple addition of a Medical Alert necklace or bracelet can save your life. Especially if you have an ICD and an external defibrillator can not be used on you . Medical Alert ID bands give medical professionals crucial knowledge of your Pacemaker or Defibrillator (ICD) insertion. As well as what the problem may be and how to treat you.
Medical Alert Necklace or Wrist band is not a compulsory item but are definitely a great addition. Most feature the international medical symbol caduceus, the image of a staff with two snakes. As well open or turn to reveal securely concealed medical identification.
Here is the medical alert ID wrist band that I have been wearing for a few years now. It states my Cardiac Sarcoidosis condition, Pacemaker and ICD on the front. Then on the back, I have my husband’s international number to contact in an emergency.
You can check out the range of Medical Alert ID bracelets here , that vary in styles and sizes. You choose the one you want, size and what you want engraved onto it.
3.1 Top tip
- Let people know about your Medical Alert Necklace or Wrist band and what to point out in an emergency.
4. Travel Insurance for your Pacemaker or Defibrillator (ICD)
Obtaining travel insurance f o r your pacemaker or defibrillator (ICD) is definitely a great idea. Especially if you are travelling to a foreign country that you have not been to before. It will not only give you peace of mind but also the people who you are travelling with too.
Currently, l obtain travel insurance for my pacemaker and ICD as and when I need it. Each trip for me is a case by case situation like hiking in Austria to skiing in France . I have found that insurance seems to be more expensive if you have had an operation within 12 months. I have had 4 operations within the last two years but again this is my situation and circumstance. Everyone is different.
4.1 If you already have travel Insurance
When you have your pacemaker /ICD implanted you will need to inform your insurer of your change of circumstances. As far as I am aware if you don’t notify them of this change you are not legally covered . At the same time check to see if travel insurance covers travelling with a pacemaker or ICD.
My policy was not vailed anymore, after my pacemaker and ICD implant. The insurer cancelled the existing policy and paid out the duration, which was fine.
4.2 If you do not have already have travel insurance
Are you unsure where to look for insurance companies specialising in travelling with a pacemaker and ICD? Firstly, check with your pacemaker clinic, the heart foundation website, or the brochures given to you by your doctor. This may take a bit of research to find the right travel insurance company, so don’t worry.
Secondly, ask your previous insurer or try a search engine company for results. I use a free search engine called AllClear Travel Compare and add in my medical information. Then it shows me my options for different insurers, a quote, and what it covers.
4.3 Tips for pacemaker or defibrillator (ICD) insurance coverage
- Ask if the country you want to travel is covered under your travel insurance.
- Print a copy of your Travel Insurance and keep it on yourself.

5. How to book a flight with a pacemaker or defibrillator (ICD)
Since writing this original post, I have taken multi flights around the world before covid. Registering when you fly is just an option and at your own discretion.
For me, if I am taking a long haul flight on my own like when I flew to Japan, Taiwan or Sierra Leone . Then I let the flight attendants know my condition when I get on the plane. Short distance flights, like when I went to Austria and Italy , I let my travelling companion know.
This is a good idea also when you are travelling a long distance by train or boat, as well.
5.1 Register as a disabled person when you fly (Optional)
Registering as a disabled person when booking your flight is an option, not something you have to do. Though it is a good idea because you are informing and making the airline company aware of your situation. If something happens mid-air, It will assist the airline on what the problem may be and how to treat you.
I didn’t register before I flew to Australia because I needed to email the airline in advance. As I needed to have clearance to carry all my medication for my condition. So they were already aware that I had a pacemaker and a defibrillator (ICD) inserted.
5.2 If you don’t register as a disabled person when you fly
If you decide not to register as a disabled person or there is no option on the booking site. Then you can let the airline know when checking in your bags. Or when you are getting onto the plane.
- You can always email the airline with your details before you fly or speak to them

6. What to do at the Airport with your Pacemaker or Defibrillator (ICD)
Going to the airport and checking in becomes a whole new experience when you have a pacemaker/defibrillator (ICD). One thing, I have learnt is that it doesn’t have to be harder than you make it. I have gotten used to people looking at me and wondering why I am getting different treatment.
Even though different countries use different methods at security airports. One thing is the same and that is letting security know that you have a pacemaker/defibrillator (ICD). Before you even go through the airport security scanners. You can set off the alarms or the scanner can interfere with your device.
6.1 Checking onto your flight with your Pacemaker or Defibrillator (ICD)
When you are checking onto your flight make the staff aware of your pacemaker or a defibrillator (ICD). This is so they can make a note of your details. Though this is not a compulsory step it makes the airline aware of your situation in case of an emergency.

6.2 Let the airport security know you have a pacemaker or defibrillator (ICD)
When going through airport security, let the staff know you have a pacemaker or defibrillator (ICD). You will be required to show proof but that will depend on the airport security you are going through. Then you will either go through a different area or skip the scanner.
Sometimes, security will also either do a hand down search or check over you with a hand-held metal detector. Don’t worry though as they will guide you through the process.
I find the easiest and most efficient way to go through airport security is having your Pacemaker/Defibrillator ID card. Then when you tell the security, you show them straight away. This saves a lot of hassles and questions, as Pacemakers and Defibrillators ID’s should be uniform.

6 Helpful Tips for Hiking with a Heart Condition or Pacemaker
Hiking or walking is great for the body and soul, especially if you have a heart condition or pacemaker. It does not matter [...]
6.3 Can you go through scanners with a pacemaker or defibrillator (ICD)
There are reasons behind not going through a security scanner at the airport with your pacemaker or defibrillator. It can interfere with the scanner’s electric waves. You can set the security alarms off (rare but can happen). It is important to follow the protocol according to unseen disabilities.
Most scanners are safe that I am aware of but don’t take my word for it. Do your own research or ask questions if you are concerned or not sure. Always best to be safe and do the right thing.
7. Top Tips for Travelling with Pacemaker and Defibrillator (ICD)
- If you are wanting to drive while away travelling, check with your doctor if it is possible. It’s recommended you wait for at least a month.
- Let your doctor know in advance if you already had travel plans booked before your surgery. As you may have to cancel your trip.
- Obtain a list of places where your pacemaker can be repaired while you are travelling. The maker of your device should have information on their website of the addresses of local hospitals. Or doctors’ offices that can help you repair the pacemaker if needed.

Thank you for reading this article ‘Travelling with a Pacemaker or Defibrillator (ICD)’. I hope it helped answer any questions you may have about travelling with your implate. I spent a week at Park Igls Medical Spa Retreat recently after my ICD stocked me back into place. I highly recommend it. I came away feeling healthy and energised.
Do you have a Pacemaker or Defibrillator (ICD) and travel? Is there something that I should add to the above list? Please feel free to share your experience in the comments below. Or let me know what I can add to the list to help others with pacemakers or ICDs.
Pin it for later!!!

⇒ Looking for inspiration on what you can do with your pacemaker and defibrillator. Please feel free to head over to my healthy heart page
Disclaimer: All views are based on my own experience and research with my own Pacemaker and Defibrillator (ICD) while travelling.
“This post contains affiliate links, which means that at no additional cost to you if you click on one of the product links, we may earn a commission.” For further details, you can view our Privacy Policy, Terms & Conditions or contact me directly.
You may also like

A Guide for Skiing in Cortina D’Ampezzo Italy

I am Mel B an indigenous Australian with dual citizenship. I am now a full-time travel blogger and content creator at MelBTravel. Writing about Adventure, Mountains, History, UK & Healthy Heart "Not letting a Defibrillator/Pacemaker & Sarcoidosis Limit Me"
12 thoughts on “ Steps to Travelling with a Pacemaker or Defibrillator (ICD) ”
Thanks so much for this information!

You are more than welcome, I hope that it helps you 🙂
It’s an informative and insightful piece. Those of us not suffering from medical conditions really give so little thought to the challenges faced by some people simply to get out and onto the road. I was chatting to a woman with a heart condition recently and was shocked by the insurance premium she’d been quoted.
Thank you very much, Stuart I appreciate your comment. Things have definitely really changed for me and now I just want to help others with same situation. Insurance is a nightmare in itself these dates.
Great article, Mel! I’m really pleased this hasn’t stopped you from travelling and doing some of the things you love.
Did you arrange special assistance at the airport? I find with my own health issues, that makes a huge difference. It’s less overwhelming (and exhausting) navigating an airport and on the occasions that I’ve been escorted, it’s generally easier going through security – staff have more patience and are more supportive.
Thank you so much for your feedback. No, I didn’t get special assistance but I was ok with it all and I had my husband with me. I didn’t realise that you had health issues and I am sorry to hear that. I do hope that everything is ok. I really wrote the article to help others.
A friend of mine passed this onto me as l have a pacemaker and l am about to fly. I just want to say thank you so much for such informative information as l struggled to find anything. What a head piece l will definitely be let other know about your post.
Thank you very much for your message Berverly, I appreciate it and I am glad that my post was able to help you. I also hope that you have a safe flight to wherever you are going.
Good informative post. I have had a pacemaker for years. Which hasn’t slowed me down. Glad to hear your still travelling & not allowing your situation to stop you. There should be more people like you out there.
Thank you Don and glad to hear that your pacemaker has not slowed you down either. Once I had got one, I realised more and more people had them or knew someone else that had one. If anything it has pushed me more to do the things that I love. Mel
This post is going to very helpful for a lot of people. The things most of us take for granted when traveling and doing things like passing through scanners!
I would love to get a bracelet
Comments are closed.
Pacemaker device support
Recovering from your procedure
What to expect from recovery.
Some people stay in the hospital overnight after receiving their pacemaker implant. Before you leave, your doctor will program your pacemaker to your specific needs. Your overall recovery process may take anywhere from a few days to a few months—each case is different and your doctor will guide you throughout the process. Below you’ll find general tips on recovery, but be sure to speak with your doctor before making lifestyle changes or going back to your usual activities.
On this page

Post-recovery guidelines
After your procedure, be sure to ask your doctor any questions you may have about your device, heart rhythm, or medication. In addition, your healthcare team will give you post-operative directions, which may include:
- Call your doctor if you have any swelling, redness or discharge around your incision, your heart rate drops below the minimum set for your pacemaker or you have a fever longer than two or three days
- Keep tight clothing and jewelry away from the skin over your device
- Avoid rubbing your device or the surrounding chest area
- Follow your doctor’s instructions for exercise and bathing
- Continue medications as instructed by your doctor
- Tell your other doctors, dentists, and emergency personnel that you have an implanted device and show them your Medical Device Identification Card
Activities and exercises
Your doctor will help you decide what level of activity is best for you. Some general guidelines include:
- Avoiding rough contact that could result in blows to your implant site
- Asking your doctor if it is safe for you to do activities that could hurt you or others if you lose consciousness, like driving, swimming alone or climbing a ladder
- Avoiding supporting your weight with your arms during sexual activity while your incision is healing
- Avoiding strenuous activity, especially lifting and other activities that use your upper body. This gives the lead(s) time to firmly attach to your heart tissue and allows the incision time to heal
- Avoiding rough contact that could result in a blow to your implant site
- Limit certain arm movements that could affect your incision site
- Avoiding lifting heavy objects until your doctor tells you it is okay
Medical Device ID Card
Whether you’re going away for the weekend or running a quick errand, it’s important to carry your Medical Device Identification Card with you at all times. Your Medical Device ID Card contains your name, your doctor’s name and phone number, and the model numbers of your device and leads. In an emergency, the card will alert medical and security personnel that you have an implanted device. You will be given a temporary Medical Device ID Card when you receive your pacemaker. Your permanent card will be mailed to your home approximately six to eight weeks after your implant.
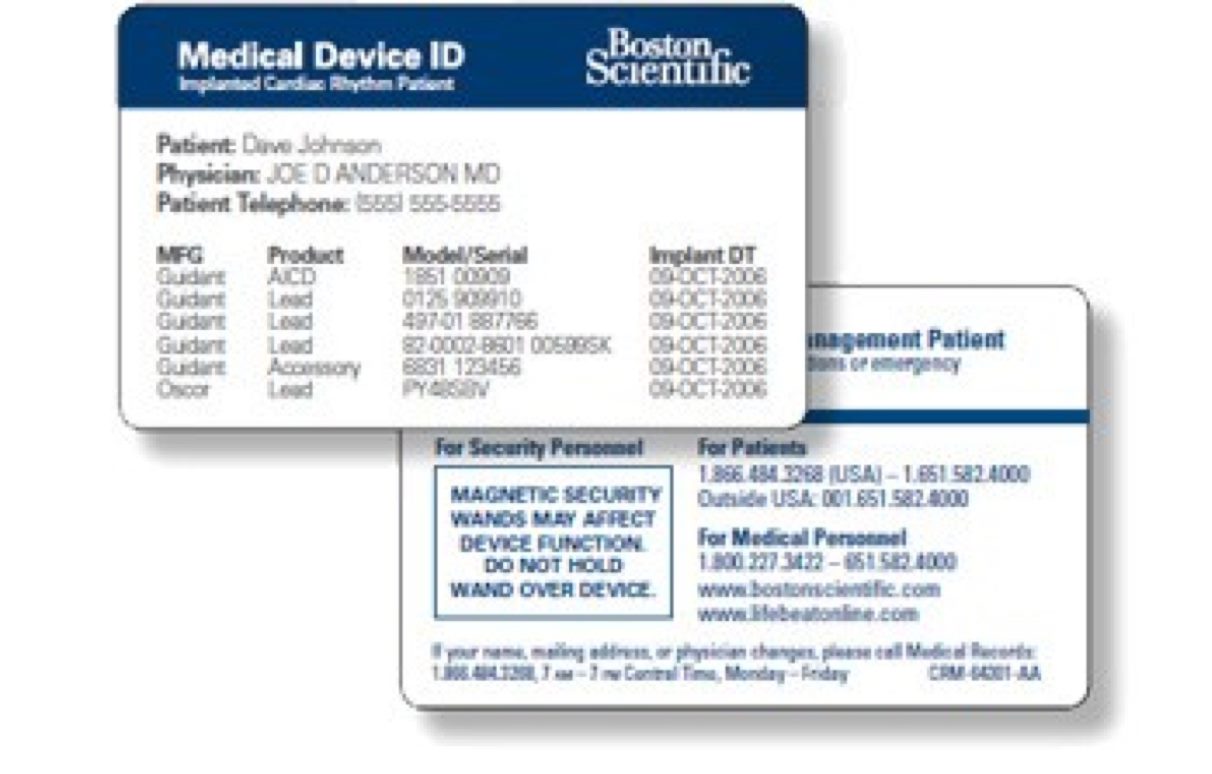
Moving or selecting a new doctor
Please tell us if you move or get a new doctor. You can use our online patient portal or call us at 1-800-728-3282 to update your record, and we will send you a new ID card.
Regular follow-up visits
Many pacemakers can be checked by the doctor’s office remotely using wireless technology. This allows your doctor to access data about your heart rate and rhythm, how your pacemaker is working, adjust settings if necessary and check its battery life.
Remote technology may mean fewer trips to the doctor. But, you’ll still need to be seen in person for follow-up visits so your doctor can adjust your pacemaker to best meet your needs. A typical follow-up visit takes about 20 minutes.
When to call a doctor
Your doctor will provide guidelines for when you should contact him or her. In general, call your doctor if you:
- Have a heart rate that drops below the lowest rate set for your pacemaker
- Develop symptoms of an abnormal heart rhythm and have been told to call
- Notice swelling, redness or drainage from your incisions
- Start a fever that lasts longer than two or three days
- Have questions about your device, heart rhythm or medications
- Plan to travel or move so you can form a care plan for while you are away
- Notice anything unusual or unexpected, like new symptoms or symptoms you had before your pacemaker
We’re here to help
Our patient services team is here to support you throughout your journey.
(866) 484-3268
Important Safety Information
A pacemaker system is designed to monitor and treat your heart rhythm problems, greatly reducing the risks associated with them. These devices are sensitive to strong electromagnetic interference (EMI) and can be affected by certain sources of electric or magnetic fields. With all medical procedures there are risks associated. In regard to an implanted pacemaker, the risks include but are not limited to inappropriate heart rate response to exercise, lead moves out of place, loss of stimulation capability, allergic reaction, fluid underneath the skin, and infection. In rare cases device failure or death can occur. Be sure to talk with your doctor so that you thoroughly understand all of the risks and benefits associated with the implantation of this system. To obtain a copy of the device Patient Handbook for more detailed device safety information, go to www.bostonscientific.com , or you can request a copy by calling 1-866-484-3268 or writing to Boston Scientific, 4100 Hamline Ave. N., St. Paul, MN 55112.
Device Quality and Reliability
It is Boston Scientific’s intent to provide implantable devices of high quality and reliability. However, these devices may exhibit malfunctions that may result in lost or compromised ability to deliver therapy. Refer to Boston Scientific’s CRM product performance report on www.bostonscientific.com for more information about device performance, including the types and rates of malfunctions that these devices have experienced historically. While historical data may not be predictive of future device performance, such data can provide important context for understanding the overall reliability of these types of products. Also, it is important that you talk with your doctor about the risks and benefits associated with the implantation of a device.
92481216 (Rev. A)
FAQs - Pacemaker implantation
How will i be monitored.
You'll be attached to a special monitor so the medical team can keep an eye on your heart rhythm.
The monitor consists of a small box connected by wires to your chest with sticky electrode patches.
The box displays your heart rhythm on several monitors in the nursing unit. The nurses will be able to observe your heart rate and rhythm.
A chest X-ray will be carried out to check your lungs, as well as the position of the pacemaker and leads.
Will I be in pain after the procedure?
You may feel some pain or discomfort during the first 48 hours after having a pacemaker fitted, and you'll be given pain-relieving medication.
There may also be some bruising where the pacemaker was inserted. This usually passes within a few days. Tell the staff if your symptoms are persistent or severe.
When can I leave hospital?
Most people are able to go home on the day they have the procedure or the day after.
You'll need to arrange for someone to pick you up from hospital and take you home.
Before going home, you'll be given a pacemaker registration card, which has the details of the make and model of your pacemaker. Always carry the card with you in case of an emergency.
You may also want to wear a MedicAlert bracelet or necklace engraved with important information, such as the type of pacemaker you have, a personal identity number and a 24-hour emergency phone number.
Find out more about medical ID jewellery on the MedicAlert website
How soon can I drive?
If you have an ordinary driving licence, you can start driving again after 1 week as long as:
- you don't have any symptoms, such as dizziness or fainting , that would affect your driving
- you have regular check-ups at the pacemaker clinic
- you haven't recently had a heart attack or heart surgery
You must also tell the Driver & Vehicle Licensing Agency (DVLA) and your insurance company that you have a pacemaker.
If you drive a large or passenger-carrying vehicle, you'll have to wait 6 weeks after your pacemaker is fitted before driving again.
Contact the DVLA to tell them about your pacemaker
Will I be able to feel or see the pacemaker?
You may be able to feel the pacemaker and it may feel uncomfortable when you lie in certain positions, but you'll soon get used to it.
Modern pacemakers are now so small they're almost completely hidden by the chest tissue and are barely noticeable.
How soon will I be back to normal?
You should feel back to your usual self, or even better, very quickly.
It's best to avoid reaching up on the side you had your operation for 4 to 6 weeks. That means not hanging out washing or lifting anything from a high shelf, for example.
But it's important to keep your arm mobile by gently moving it to avoid getting a frozen shoulder . A physiotherapist can show you how to do this.
You'll usually be able to do all the things you want to do after around 4 weeks.
The time you need off work will depend on your job. Your cardiologist will usually be able to advise you about this.
Typically, people who have had a pacemaker fitted are advised to take about a week off work.
People who drive for a living, such as bus and lorry drivers, will not be allowed to drive these types of vehicles for at least 6 weeks after the pacemaker is fitted.
When can I exercise or play sports again?
You should avoid strenuous activities for around 4 to 6 weeks after having your pacemaker fitted. After this, you should be able to do most activities and sports.
But if you play contact sports such as football or rugby, it's important to avoid collisions. You may want to wear a protective pad.
Avoid very energetic activities, such as squash.
The British Heart Foundation has more information and advice about how to start exercising again after having heart surgery
How can I care for my wound?
Do not get your wound wet until your stitches have been taken out. After that, avoid wearing anything that rubs against the area of your wound, such as braces.
Women may need a new bra with wider straps. Avoid exposing your wound to sunlight in the first year as this can cause a darker scar.
Will I have to have my stitches removed?
It depends on the kind of stitches used. Many doctors use soluble stitches that dissolve on their own. Before you go home, you'll be told what type of stitches you have.
If you need to have your stitches removed, it'll usually be after about 7 to 10 days.
What check-ups will I need?
You'll usually have your pacemaker checked after 4 to 6 weeks at the hospital where it was fitted.
After this, you'll have it checked every 3 to 12 months, depending on the type of pacemaker you have and how well it’s been working.
If after having the pacemaker fitted and leaving hospital you feel you're not getting as much benefit as you imagined, your pacemaker may need some small adjustments.
The cardiologist or cardiac technician will be able to do this.
What problems should I look out for?
Signs that your pacemaker is not working as it should or you have developed an infection or blood clot include:
- breathlessness
- prolonged weakness
- a swollen arm on the side of the pacemaker
- chest pains
- prolonged hiccups
- a high temperature
- pain, swelling and redness at the site of the pacemaker
Contact your GP or cardiologist as soon as possible for advice if you experience any of these problems after having a pacemaker fitted.
If this is not possible, call NHS 111 or your local out-of-hours service .
Will my pacemaker be affected by electrical equipment?
Anything that produces a strong electromagnetic field, like an induction hob, can interfere with a pacemaker.
Most common household electrical equipment, such as hairdryers and microwave ovens, will not be a problem, as long as you use them at least 15cm (6 inches) away from your pacemaker.
If you have an induction hob, keep a distance of at least 60cm (2ft) between the stove top and your pacemaker.
If this is a problem, you may want to consider replacing the appliance with something more suitable.
If you feel dizzy or your heart beating faster while using an electrical appliance, simply move away from it to allow your heartbeat to return to normal.
Mobile phones
It's safe to use a mobile phone, but make sure you keep it more than 15cm (6 inches) from your pacemaker. Use a headset or the ear on the opposite side to the pacemaker.
Shop security systems
Walking steadily through an anti-theft detector in a shop doorway should not affect your pacemaker, but do not stand too close to this type of security device for long.
Airport security systems
Airport security systems do not usually cause problems with pacemakers, but carry your pacemaker identification card with you and tell security staff you have a pacemaker.
Security staff in some countries may insist you pass through the scanner. Move quickly through it and do not linger nearby.
Handheld metal detectors shouldn't be placed directly over your pacemaker.
MRI scans are not usually recommended for people with pacemakers because they produce strong magnetic fields.
MRI-safe pacemakers and implantable cardioverter defibrillators (ICDs) are becoming more common.
Other types of medical tests are safe, but always tell the person treating you that you have a pacemaker.
TENS machines
TENS machines should not be used without first consulting your pacemaker clinic or manufacturer. They produce small electrical impulses that could interfere with your pacemaker.
Lithotripsy
Lithotripsy, a treatment for kidney stones , must be avoided if you have a pacemaker fitted.
General advice
If your job brings you into contact with strong electrical fields, such as arc welding, diathermy or working with high-power radio or TV transmitters, or you have direct contact with car ignition systems, check with your cardiologist or pacemaker technician before returning to work.
Avoid wearing magnetic bracelets and magnets near your chest.
Will I need to have another pacemaker?
Most pacemaker batteries last for 6 to 10 years. After this, you may need to have the batteries changed.
Ask your doctor how you'll know when the battery needs to be replaced or recharged.
Changing the batteries involves replacing the pacemaker box with a new unit. This is a simple procedure that may or may not require an overnight stay in hospital.
The original lead or leads can usually be left in place, although occasionally they'll also need to be replaced.
How often will I need follow-up appointments?
You'll need follow-up appointments for the rest of your life after having a pacemaker fitted.
These may be every 3 to 12 months, depending on the type of pacemaker you have and how well it works.
At your follow-up appointment, the technician or doctor will analyse the discharge rate of your pacemaker, measure the strength of the electrical impulse, and record the effects of the impulse on your heart.
Most modern pacemakers can store information about the state of the battery and the performance of the pulse generator.
Your pacemaker can then be reprogrammed to the best settings for you, if necessary.
Will my sex life be affected?
There's no reason you cannot continue to have a good sex life after having a pacemaker implanted and you're feeling better.
But you should avoid positions that place pressure on the arms and chest for the first 4 weeks of your recovery.
The risk of sex triggering a heart attack is low (around 1 in 1 million).
Who should I tell about my pacemaker?
You should tell your doctor, nurse and dentist about your pacemaker, as you may need to avoid some medical tests and treatments, such as MRI scans and the use of TENS machines.
You should also tell your family and close friends that you have a pacemaker fitted. Tell them what to do if you lose consciousness or collapse.
Will the pacemaker improve my quality of life?
Most people who have a pacemaker fitted feel it has a tremendously positive impact on their life.
Having a pacemaker can help you be more active. It may also help you stay out of hospital and live longer.
Above all, you should feel better. Previous symptoms, such as breathlessness or dizziness, should disappear.
Page last reviewed: 26 July 2022 Next review due: 26 July 2025

COMMENTS
The recovery time after pacemaker surgery can vary and depend on individual factors such as: . overall health; age; the specific circumstances of the surgery; Generally, people can go home either ...
In addition to your Medical Device ID Card, Boston Scientific offers a security card for international travel. The card explains that your implanted device may trigger airport security alarms and is printed in 13 languages. To get a Medical Device Patient Security Card, call us at 1-866-484-3268.
Soon after your surgery, you may hardly think about your pacemaker as you go about your day. Just be sure to follow your doctor's recommendations about daily activities. ... Feel free to take baths and showers after 2 days. Your pacemaker is completely protected against contact with water. Car, train or airplane trips should pose no danger.
Pacemaker Side Effects. Most people who receive a pacemaker don't experience any side effects other than some pain or discomfort when the device is implanted. However, there is a small risk of complications including: Infection at the insertion site. Bleeding, bruising, or swelling. Bleeding in the heart at the lead sites.
A pacemaker is a small, battery-powered device that prevents the heart from beating too slowly. You need surgery to get a pacemaker. The device is placed under the skin near the collarbone. A pacemaker also is called a cardiac pacing device. There are different types of pacemakers. Single chamber pacemaker. This type usually sends electrical ...
Daily Living - Pacemakers. Many people with an implantable heart device resume their normal daily activities after full recovery from surgery. However, there may be certain situations that your doctor will ask you to avoid. Your doctor or nurse will provide guidance for your particular condition, but these are some general guidelines to ...
Steps. 1. Ask your doctor if your pacemaker contains any metal. Some versions do not contain metal, and they will not cause any trouble if you choose to travel through airport security screening areas. [1] 2. Ask your doctor for an official card that states you have an implanted pacemaker.
You will go home with instructions on when to follow up and how to care for your pacemaker. Recovery after surgery is a gradual process. Recovery time varies depending on the procedure, type of anesthesia, your general health, age, and other factors. Your doctor may ask you to avoid strenuous activities or heavy lifting for about a month after ...
Patient Security Card. Boston Scientific offers a security card for you to carry when traveling. The card explains that your implanted device may trigger airport security alarms and is printed in 13 languages. To get a Patient Security Card, call us at 1-866-484-3268.
As you recover from your procedure, your pacemaker may allow you to return to an active lifestyle. But it's important to follow your doctor's instructions, including: Walk, exercise and bathe according to your doctor's instructions. Don't wear tight clothing that could irritate the skin over your implant.
During the first 6 weeks after the implant: DO NOT lift anything that weighs more than 10 pounds with the arm on the side of your body that has the pacemaker. DO NOT push or pull heavy objects. Avoid doing things like shoveling snow, mowing the lawn, know within 24 hours if there are changes to your device or heart rhythm.
Pacemaker surgery may be an outpatient procedure or an inpatient procedure based on your health and the cause of the rhythm disorder. A pacemaker is used for long-term correction of a too-slow heartbeat ( arrhythmia) or temporarily, such as after open-heart surgery. Implanting a pacemaker is considered a minimally invasive procedure.
Create a travel and emergency action plan for long-distance trips; Talk with you about travel safety rules for equipment; ... Usually, you need to wait at least 6-8 weeks after surgery before your doctor will approve you to drive. Some states have laws against letting people with a history of fainting, dizziness or cardiac arrest behind the wheel.
After Getting a Pacemaker. After getting a permanent pacemaker, you will recover in the hospital for a few hours or overnight. Your healthcare team will tell you about any precautions or problems to watch out for during your recovery. You will receive a card with information about the device and its settings, your doctor, and the hospital where ...
We'll share tips and advice related to travel with a pacemaker and also Ethan's own personal experience and thoughts on flying and traveling with his new pacemaker. Home; Blog; ... Normally after a successful pacemaker surgery you should be able to fly soon after surgery. The issues as noted in this article tend to be more about security ...
Those who have had heart valve repair or replacement surgery or coronary artery bypass grafts (open heart surgery) can usually fly after 4-6 weeks (longer if they have had pulmonary complications). Generally speaking, if you can walk briskly for 100 metres on the flat without being breathless or in pain, you can fly.
2. Pacemaker or Defibrillator (ICD) identification card. Make sure you have your Pacemaker or Defibrillator (ICD) identification card with you before you travel. If you don't know where it is or don't have one, ask your pacemaker clinic for a copy. As my understanding is there should be one in your file.
Chances are your pacemaker won't mean you can't travel - but if you've recently had surgery or an episode of ill health, such as a heart attack, you might be advised to postpone plans to fly until you're better. ... Handheld metal detectors shouldn't be held directly above your pacemaker. 3: Look after yourself This is common sense ...
To obtain a copy of the device Patient Handbook for more detailed device safety information, go to www.bostonscientific.com , or you can request a copy by calling 1-866-484-3268 or writing to Boston Scientific, 4100 Hamline Ave. N., St. Paul, MN 55112. Device Quality and Reliability. It is Boston Scientific's intent to provide implantable ...
Having a pacemaker can help you be more active. It may also help you stay out of hospital and live longer. Above all, you should feel better. Previous symptoms, such as breathlessness or dizziness, should disappear. You'll usually be able to go home on the same day or the day after having a pacemaker fitted.
Arnold Schwarzenegger reveals he is recovering after surgery to get pacemaker that's life with a genetic heart issue. Find out how the actor and former governor is doing now.