
- 800-3-ADVOCATE
- Español
- Find a Doctor
- Find a Location
- Sign in to Live Well

Send a message to a telehealth provider and get a diagnosis within one hour - 24/7.

Virtual care is just a few questions away
When you or your child isn't feeling well, e-visits can get you a quick diagnosis, 24/7. You'll fill out a questionnaire about your symptoms and a telemedicine provider will evaluate your condition and share a treatment plan – all by messaging you within an hour. For minor illnesses like back pain, cold symptoms and urinary infections, an e-visit can be a convenient, cost-effective alternative to visiting a clinic or urgent care.
When should I use an e-visit?
You can use telehealth visits , like e-visits, to get virtual care 24/7. E-visits are easy, online messages with a virtual care provider who can address this set list of common, nonurgent symptoms:
- Anxiety or depression
- Bladder or urinary infection
- Birth control refill
- Cold symptoms
- Erectile dysfunction
- Head lice (pediatric)
- COVID symptoms (with positive test result)
- Vaginal discharge or irritation
To ensure you’re receiving the best care possible, you may be asked to come in for lab tests such as a urine sample or to pick up medication as a result of your e-visit.
Can I use insurance to cover the cost of an e-visit?
Yes, we’ll bill your e-visit to your insurance. Your visit is subject to any coinsurance, copay or deductible – just like an in-person visit. You’ll receive a statement detailing your financial responsibility.
We're also able to provide e-visits if you have Medicare or Medicaid as your primary or secondary insurance.
Who can request an e-visit?
If you're an Advocate Health Care patient, are 18 or older and are physically located in Illinois, Wisconsin or Michigan, you can request a telehealth e-visit for yourself. You can also submit an e-visit for kids ages 2-11 if you're their legally authorized representative. Learn about proxy/dependent care .
Are e-visits safe?
Yes, we keep your personal health information safe when you request an e-visit through your LiveWell account.
How do I start an e-visit?
It takes a few minutes to start your e-visit in LiveWell. We walk you through the steps of starting an e-visit , plus answer common questions you may have.
Where can I learn more about LiveWell?
We can help answer your questions about LiveWell and its features.
How can I ask additional medical questions after an e-visit?
If you’ve recently had an e-visit and have additional medical questions, you can call 844-284-0381 to speak with a virtual health nurse.
Start an e-visit in LiveWell

Sign in to LiveWell and request an e-visit.

Answer a few quick questions about your symptoms.

Watch for a message with your diagnosis and next steps within one hour.
Still need a LiveWell account?
Download the LiveWell app and create an account in one easy step! You’ll find more ways to live well on the go – message your primary care provider, get test results, practice guided meditation and more.
Learn more about LiveWell and its features .
Create your LiveWell account

Other ways to get virtual care

Quick Care Video Visits
With Quick Care Video Visits, you can get access to medical care 24/7 with a video call.

Video visits with your provider
Meet with your primary care provider, specialist or other members of your care team – from home.
What to Expect from Your First Telemedicine Visit for Sinus Problems

Your nose is stuffed up and you can’t breathe well. You have a runny nose and other cold-type symptoms. If it’s a sinus infection, do you need an antibiotic?
Dr. Nilesh Patel, board-certified otolaryngologist , treats many patients with sinus problems . If it’s too difficult for you to come into the office for an appointment, we offer convenient telemedicine appointments to treat your sinus issues. Some health issues require an in-person appointment. But many sinus issues can be handled with a video visit.
What is a sinus infection?
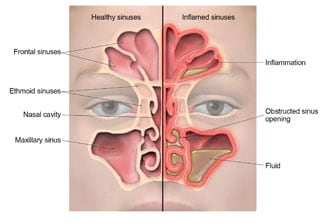
You have a sinus infection when the tissue in your nasal passages and sinuses are inflamed and swollen. Sinuses extend into your forehead, between your eyes, and behind your cheeks. They produce mucus that keeps your nose from drying out, which in turn guards against allergens and pollutants in the environment.
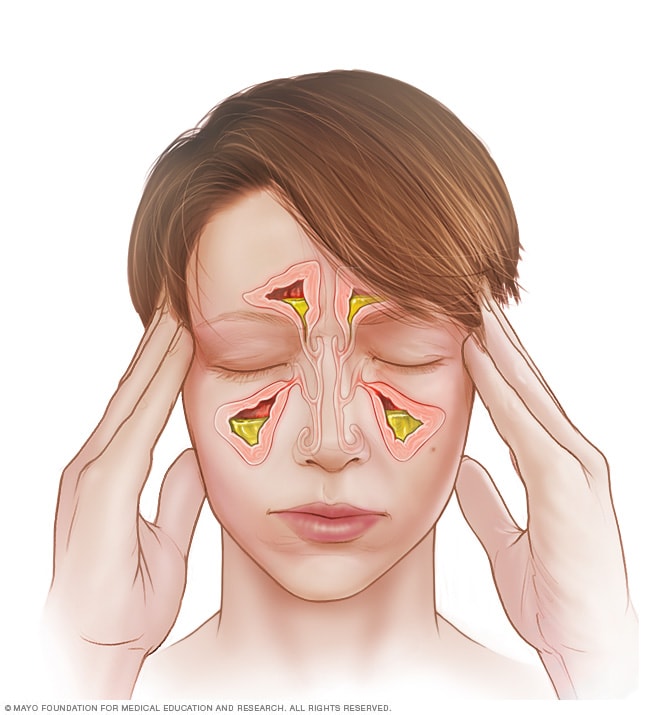
When your sinuses are inflamed, the passage is blocked and your normal nasal fluid can’t drain properly. Fluid becomes trapped and clogs your sinus passages. In that warm, moist environment, viruses and bacteria thrive, so an infection can develop.
What happens during a telemedicine visit for sinus problems?
Our office offers telemedicine appointments for some sinus problems. Telemedicine offers several obvious benefits. You don’t have to fight traffic and the weather when you’re not feeling well. You don’t have to sit in a waiting room with other sick people. You can concentrate on just getting well while resting at home.
Before your telemedicine appointment, we send you forms to complete. We need a thorough medical history so that we are aware of any factors, such as allergies or asthma, that have a bearing on your sinus problems. You’ll need to give your permission for a video visit.
We send you a link to open a few minutes prior to your appointment with Dr. Patel. During the visit, Dr. Patel reviews your medical history and asks you specific questions that help him determine if you have a sinus infection. Based on your own history and your responses, he determines what course of action is needed.
Following are common symptoms of a sinus infection:
- Closed or partially closed nasal passages
- Pain or pressure around the front of your head, including your forehead, nose, eyes, upper jaws and teeth
- Post-nasal drip with mucus draining down your throat
- Green nasal discharge
- Sore throat
- Fever
If you don’t have a fever or have a low-grade fever, your sinus infection is very likely a viral infection. An antibiotic doesn’t help if your infection is caused by a virus.
If you have signs of a bacterial infection, Dr. Patel prescribes an antibiotic. Signs of a bacterial infection include the following:
- A high fever of over 100 degrees occurring more than three or four days
- Severe pain which may be only on one side of your nose
- Discolored nasal discharge
- Symptoms that are worse after temporarily improving
If you have frequent sinus infections, have chronic post-nasal drip, and/or suffer often from sinus headaches, and other treatments such as nasal sprays, drops, and antibiotics haven’t worked, Dr. Patel may suggest a minor minimally invasive technique called a balloon sinuplasty that expands your sinuses so you can breathe easily again.
Call Dr. Nilesh Patel today or request a same-day appointment through our online portal for expert ear, nose, and throat care.
You Might Also Enjoy...

5 Signs Your Thyroid Is Off

Tips for Beating a Sinus Headache

I Have Allergies — Will My Children Have Them As Well?

Reasons Why Your Voice Is Hoarse (And What to Do About It)

Do This Now If You Want to Avoid Sinusitis This Winter

Why Does My Child Keep Getting Ear Infections?
- Patient Care & Health Information
- Diseases & Conditions
- Acute sinusitis
Acute sinusitis causes the spaces inside the nose, known as sinuses, to become inflamed and swollen. Acute sinusitis makes it hard for the sinuses to drain. Mucus builds up.
Acute sinusitis can make it hard to breathe through the nose. The area around the eyes and the face might feel swollen. There might be throbbing face pain or a headache.
The common cold is the usual cause of acute sinusitis. Most often, the condition clears up within a week to 10 days unless there's also an infection caused by bacteria, called a bacterial infection. Home remedies might be all that's needed to treat acute sinusitis. Sinusitis that lasts more than 12 weeks even with medical treatment is called chronic sinusitis.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Allergy and Sinus Solutions from Mayo Clinic Store
- Assortment of Health Products from Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Acute sinusitis symptoms often include:
- Thick, yellow or greenish mucus from the nose, known as a runny nose, or down the back of the throat, known as postnasal drip.
- Blocked or stuffy nose, known as congestion. This makes it hard to breathe through the nose.
- Pain, tenderness, swelling and pressure around the eyes, cheeks, nose or forehead that gets worse when bending over.
Other signs and symptoms include:
- Ear pressure.
- Aching in the teeth.
- Changed sense of smell.
- Bad breath.
When to see a doctor
Most people with acute sinusitis don't need to see a health care provider.
Contact your health care provider if you have any of the following:
- Symptoms that last more than a week.
- Symptoms that get worse after seeming to get better.
- A fever that lasts.
- A history of repeated or chronic sinusitis.
See a health care provider immediately if you have symptoms that might mean a serious infection:
- Pain, swelling or redness around the eyes.
- High fever.
- Double vision or other vision changes.
- Stiff neck.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
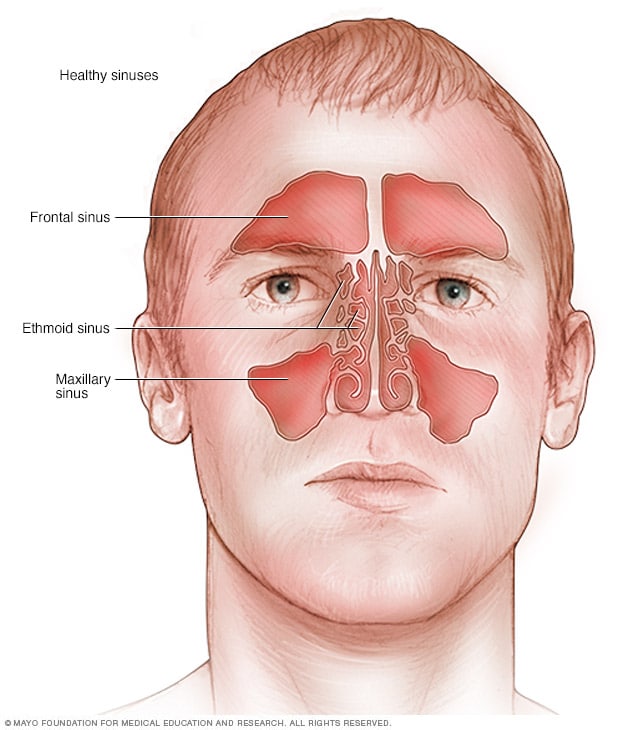
Healthy sinuses
Sinuses are cavities around nasal passages. If the sinuses become inflamed and swollen, a person may develop sinusitis.
Acute sinusitis is most often caused by the common cold. Signs and symptoms may include a blocked and stuffy (congested) nose, which may block your sinuses and prevent drainage of mucus.
Acute sinusitis is an infection caused by a virus. The common cold is most often the cause. Sometimes, sinuses that are blocked for a time might get a bacterial infection.
More Information
- Sinus infection and toothache: Any connection?
Risk factors
The following can raise the risk of getting sinusitis:
- Hay fever or another allergy that affects the sinuses.
- A common cold that affects the sinuses.
- A problem inside the nose, such as a deviated nasal septum, nasal polyps or tumors.
- A medical condition such as cystic fibrosis or an immune system disorder such as HIV/AIDS.
- Being around smoke, either from smoking or being around others who smoke, known as secondhand smoke.
Complications
Acute sinusitis doesn't often cause complications. Complications that might happen include:
- Chronic sinusitis. Acute sinusitis can be a flare-up of a long-term problem known as chronic sinusitis. Chronic sinusitis lasts longer than 12 weeks.
- Meningitis. This infection affects the membranes and fluid around the brain and spinal cord.
- Other infections. It's not common. But an infection can spread to the bones, known as osteomyelitis, or to skin, known as cellulitis.
- Vision problems. If the infection spreads to the eye socket, it can reduce vision or cause blindness.
Take these steps to help lower your risk of getting acute sinusitis:
- Stay well. Try to stay away from people who have colds or other infections. Wash your hands often with soap and water, such as before meals.
- Manage allergies. Work with your health care provider to keep symptoms under control.
- Avoid cigarette smoke and polluted air. Tobacco smoke and other pollutants can irritate lungs and inside the nose, known as nasal passages.
- Use a machine that adds moisture to the air, known as a humidifier. If the air in your home is dry, adding moisture to the air may help prevent sinusitis. Be sure the humidifier stays clean and free of mold with regular, complete cleaning.
- Ferri FF. Sinusitis. In: Ferri's Clinical Advisor 2023. Elsevier; 2023. https://www.clinicalkey.com. Accessed Feb. 2, 2023.
- Sinusitis (sinus infection or sinus inflammation). American Academy of Allergy, Asthma & Immunology. https://aafa.org/allergies/allergy-symptoms/sinusitis-sinus-infection/. Accessed Feb. 2, 2023.
- Patel ZM, et al. Acute sinusitis and rhinosinusitis in adults: Clinical manifestations and diagnosis. https://www.uptodate/com/contents/search. Accessed Feb. 2, 2023.
- AskMayoExpert. Acute bacterial rhinosinusitis. Mayo Clinic; 2022.
- Bennett JE, et al. Sinusitis. In: Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Feb. 2, 2023.
- Sinus infection. American College of Allergy Asthma and Immunology. https://acaai.org/allergies/allergic-conditions/sinus-infection/. Accessed Feb. 2, 2023.
- Sinus infection (sinusitis). Centers for Disease Control and Prevention. https://www.cdc.gov/antibiotic-use/community/for-patients/common-illnesses/sinus-infection.html. Accessed Feb. 2, 2023.
- Elderflower. Natural Medicines. https://naturalmedicines.therapeuticresearch.com. Accessed Feb. 2, 2023.
- Acute sinusitis: Do over-the-counter treatments help?
- Sinusitis and tooth pain
Associated Procedures
- Allergy skin tests
News from Mayo Clinic
- Mayo Clinic Q and A: Sinusitis and treatment options Oct. 02, 2022, 11:00 a.m. CDT
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Conclusions
- Article Information
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
Mehrotra A , Paone S , Martich GD , Albert SM , Shevchik GJ. A Comparison of Care at E-visits and Physician Office Visits for Sinusitis and Urinary Tract Infection. JAMA Intern Med. 2013;173(1):72–74. doi:10.1001/2013.jamainternmed.305
Manage citations:
© 2024
- Permissions
A Comparison of Care at E-visits and Physician Office Visits for Sinusitis and Urinary Tract Infection
Author Affiliations: University of Pittsburgh School of Medicine (Drs Mehrotra and Martich), RAND Corporation (Dr Mehrotra), University of Pittsburgh Medical Center Health System (Drs Paone, Martich, and Shevchik), and University of Pittsburgh Graduate School of Public Health (Dr Albert), Pittsburgh, Pennsylvania.
Internet capabilities create the opportunity for e-visits, in which physicians and patients interact virtually instead of face-to-face. In e-visits, patients log into their secure personal health record internet portal and answer a series of questions about their condition. This written information is sent to the physicians, who make a diagnosis, order necessary care, put a note in the patients' electronic medical records, and reply to the patients via the secure portal within several hours. E-visits are offered by numerous health systems and are commonly reimbursed by health plans. 1 , 2 They typically focus on care for acute conditions, such as minor infections.
There are several potential advantages of e-visits, including convenience and efficiency (avoiding travel and time) and lower costs. 3 Furthermore, e-visits can be provided by the patient's primary care physician instead of a physician at an emergency department or urgent care center. The main concerns about e-visits center on quality issues: whether physicians can make accurate diagnoses without a face-to-face interview or physical examination, 4 whether the use of tests and follow-up visits is appropriate, and whether antibiotics might be overprescribed.
To our knowledge, no studies have characterized the differences between e-visits and office visits. To fill this knowledge gap, we compared the care at e-visits and office visits for 2 conditions: sinusitis and urinary tract infection (UTI).
We studied all e-visits and office visits at 4 primary care practices within the University of Pittsburgh Medical Center Health System, Pittsburgh, Pennsylvania. These practices were the first to offer e-visits, but they are now offered at all primary care office locations. The practices have a total of 63 internal medicine and family practice physicians. We identified all office visits and e-visits for sinusitis and UTI at these practices between January 1, 2010, and May 1, 2011. Structured data were obtained directly from the electronic medical records (EpicCare).
Of the 5165 visits for sinusitis, 465 (9%) were e-visits. Of the 2954 visits for UTI, 99 were e-visits (3%). Physicians were less likely to order a UTI-relevant test at an e-visit (8% e-visits vs 51% office visits; P < .01) ( Table ). Few sinusitis-relevant tests were ordered for either type of visit. For each condition, there was no difference in how many patients had a follow-up visit either for that condition or for any other reason ( Table ).
Physicians were more likely to prescribe an antibiotic at an e-visit for either condition. The antibiotic prescribed at either type of visit was equally likely to be guideline recommended. We looked at possible explanations for the lower office visit antibiotic rate ( Table ). Among UTI office visits, the antibiotic prescribing rate was 32% when a urinalysis or urine culture was not ordered compared with 61% when a urinalysis or urine culture was ordered.
During e-visits for both conditions, physicians were less likely to order preventive care. Among patients with an e-visit for either condition, we tracked where they received care for any subsequent visits. Among e-visit patients, there were 147 subsequent episodes of sinusitis or UTI. Among these episodes, 73 (50%) were e-visits.
Our findings refute some concerns about e-visits but support others. The fraction of patients with any follow-up was similar. Follow-up rates are a rough proxy for misdiagnosis or treatment failure and the lack of difference will therefore be reassuring to patients and physicians. Among e-visit users, half will use an e-visit when they have a subsequent illness in the next year. Patients appear generally satisfied with e-visits.
On the other hand, antibiotic prescribing rates were higher at e-visits, particularly for UTIs. When physicians cannot directly examine the patient, physicians may use a “conservative” approach and order antibiotics. The high antibiotic prescribing rate for sinusitis for both e-visits and office visits is also a concern given the unclear benefit of antibiotic therapy for sinusitis. 5
Our data support the idea that e-visits could lower health care spending. While we did not directly measure costs, we can roughly estimate costs using Medicare reimbursement data and prior studies. 6 , 7 If we focus on UTI visits, the lower reimbursement for the e-visits ($40 e-visit vs $69 office visit [CPT 99213]) and the lower rate of testing ($11 urine culture) at e-visits outweigh the increase in prescriptions ($17 average prescription). In total, the estimated cost of UTI visits was $74 for e-visits compared with $93 for office visits.
There are several key limitations of our analyses. Our analyses are based on diagnosis codes and not on the patient's presenting symptoms. We captured only follow-up visits, and future studies should prospectively follow up outcomes such as resolution of symptoms. We do not compare phone care for these conditions, which is commonly provided in primary care. Our results highlight key differences between office visits and e-visits and emphasize the need to assess the clinical impact of e-visits as their popularity grows.
Correspondence: Dr Mehrotra, Department of Medicine, University of Pittsburgh School of Medicine, 230 McKee Pl, Ste 600, Pittsburgh, PA 15213 ( [email protected] ).
Published Online: November 19, 2012. doi:10.1001/2013.jamainternmed.305
Author Contributions: Study concept and design : Mehrotra, Paone, Martich, and Shevchik. Acquisition of data : Mehrotra, Paone, Martich, and Shevchik. Analysis and interpretation of data : Mehrotra, Martich, and Albert. Drafting of the manuscript : Mehrotra and Paone. Critical revision of the manuscript for important intellectual content : Martich, Albert, and Shevchik. Statistical analysis : Mehrotra and Albert. Obtained funding : Mehrotra, Paone, and Martich. Administrative, technical, and material support : Paone, Martich, and Shevchik. Study supervision : Mehrotra, Paone, Martich, and Shevchik.
Conflict of Interest Disclosures: None reported.
Funding/Support: This study was supported in part by funding from the National Institutes of Health (KL2 RR24154-6, R21 AI097759-01) and the University of Pittsburgh Medical Center.
Online-Only Material: Listen to an author interview about this article, and others, at http://bit.ly/OsqsNt .
Previous Presentation: This study was presented in part at the AcademyHealth Annual Research Meeting; June 25, 2012; Orlando, Florida.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Appl Clin Inform
- v.7(2); 2016

Sinusitis Treatment Guideline Adherence in the E-Visit Setting
Kevin l. smith.
1 Zipnosis, Minneapolis, Minnesota, United States
2 Fairview Health System, Minneapolis, Minnesota, United States
Bonnie L. Westra
3 University of Minnesota, School of Nursing, Minneapolis, Minnesota, United States
Studies demonstrate poor guideline adherence by health care providers for the treatment of upper respiratory infections, particularly acute bacterial rhinosinusitis (ABRS), in the appropriate prescribing of antibiotic medications.
The purpose of this quality improvement project was to evaluate the effect of implementing interventions for improving adherence to a clinical practice guideline for the management of ABRS for patients treated in the e-visit setting. Interventions included: providing a report to providers of their adherence to the ABRS clinical guideline prior to the intervention, providing updated education on the ABRS guideline, and implementing a clinical decision support system reminder.
A pre and post intervention evaluation design was used. Data were obtained from a retrospective electronic health record (EHR) data extract of all 316 diagnoses for ABRS in the pre-intervention 2-month time period and all 368 diagnoses of ABRS in the post-intervention 2-month time period. A review of the structured clinical data elements was performed to determine whether the provider adhered to the clinical guideline, meaning that only patients meeting the criteria for ABRS were to receive an antibiotic prescription.
Results and Conclusion
The interventions resulted in a 3.3% improvement in adherence to the ABRS clinical guideline from 95.25% adherence pre-intervention to 98.4% post-intervention. These results demonstrated that the use of an educational intervention and clinical decision support resulted in improved adherence to the ABRS clinical guideline in the e-visit setting. The implications for practice could be significant in that these quality improvement interventions improve guideline adherence and reduce unnecessary prescribing of antibiotics.
1. Background
Inappropriate antibiotic prescribing is common in spite of established upper respiratory infection (URI) guideline recommendations. Gill et al. [ 1 ] reported poor guideline adherence for the treatment of URIs, with providers prescribing antibiotics at rates in excess of the incidence of bacterial respiratory infections. Gill et al. reported 81% of patients received antibiotics for ABRS, and 65% of all URI patients with viral infections received antibiotics inappropriately. In fact, only 0.5% to 2.0% of all URI episodes result in a bacterial infection [ 2 ], which would justify using antibiotics. In Crocker et al’s study, ABRS antibiotic guideline adherence rates were 43% [ 3 ].
The Centers for Disease Control and Prevention (CDC) [ 4 ] estimates that nearly 50% of antibiotics prescribed in the outpatient setting are unnecessary and that overuse of antibiotics is resulting in increased antibiotic-resistant organisms. In particular, streptococcus pneumonia, a major cause of ear and sinus infections, is resistant to one or more clinically appropriate antibiotics in 30% of severe infections.
Sinus infections prevalence rates are high. According to the National Center for Health Statistics, ABRS affects one in seven adults annually [ 5 ]. ABRS is one of the most common diagnoses made in the primary care setting, resulting in approximately 31 million individuals diagnosed each year in the United States. ABRS is the fifth most common condition diagnosed in which antibiotics are prescribed in the United States and it accounts for 15% to 21% of all antibiotics prescribed for adults in the outpatient setting [ 6 , 7 ]. In a study comparing e-visits (an online interaction between a health care provider and a patient) and office visits for ABRS and urinary tract infections (UTIs), Mehrotra et al. [ 8 ] demonstrated a slightly higher adherence to specific antibiotic prescribing per guideline recommendation for ABRS via e-visit (70%) versus in-person clinic visits (67%). However, overall antibiotic prescribing rates were slightly higher for e-visit patients for ABRS via e-visit (99%) versus in-person clinic visits (94%).
The diagnosis of ABRS is typically a clinical decision based primarily on the patient history. According to the Infectious Disease Society of America (IDSA) guideline [ 9 ], ABRS should be considered in patients who present with any of the following factors: (a) persistent symptoms or signs of ABRS lasting 10 or more days with no clinical improvement, (b) onset of illness with severe symptoms (fever >102°F and purulent nasal discharge or facial pain) lasting at least 3 consecutive days at the beginning of illness, or (c) onset with worsening symptoms following a viral URI that lasted 5–6 days and was initially improving. The Institute for Clinical Systems Improvement (ICSI) [ 10 ] the CDC [ 11 ], and the American Academy of Otolaryngology—Head and Neck Surgery Foundation (AAO-HNS) [ 12 ] also have published evidence-based guidelines addressing appropriate diagnosis and treatment of URIs, including ABRS, which are in agreement with the IDSA guideline.
Various technology-based strategies have been studied for improving antibiotic stewardship. In a hospital based pediatric setting, Agwu et al [ 13 ] evaluated the impact of an Internet based antibiotic stewardship program which demonstrated reduction in antibiotic prescribing and cost. In a similar study using an Internet based antibiotic stewardship preapproval program over six years, Sick et al [ 14 ] demonstrated an effective reduction in the number of antibiotic doses and cost. Improved provider adherence to clinical-practice guidelines for minor acute illnesses, such as URIs, including sinusitis, has been demonstrated through the use of (CDSS) tools. These tools make it easier for the provider to choose the most appropriate treatment option and to offer feedback to providers regarding their practice patterns related to adhering to established guidelines [ 15 , 16 , 17 ].
For this project, an e-visit is defined as an asynchronous encounter between a patient and a provider; there is no real-time interaction with the patient such as a phone call or real-time video encounter. The patient completes a structured online health history for a specific health problem or concern. When patients have completed entering their health history e-visit information into the software system, the provider is electronically sent a text message or pager notification that a patient e-visit is ready to be reviewed. The provider is required to log in to the secure system to review and to respond to the e-visit within one hour. The structured patient history gathering process utilizes branching logic to capture relevant patient information according to evidence based practice guidelines. The clinicians are presented with the patient history as well as guideline-based assessment and treatment options utilizing clinical decision support system (CDSS) tools.
2. Objectives
The purpose of this quality improvement project was to evaluate provider adherence to ABRS clinical-practice guidelines in the e-visit setting. Conditions commonly treated via e-visits include minor acute illnesses such as upper respiratory infections, uncomplicated female bladder infections, conjunctivitis, and selected skin conditions.
3.1 Study Design and Setting
A pre and post intervention evaluation design was used. Each of the 29 participating e-visit providers (physicians, nurse practitioners, and physician assistants), employees of a large Midwest integrated health system, agreed to participate in the study. They received a pre-intervention report of their percentage rate of adherence to the ABRS guideline, received an educational intervention, and were provided with CDSS tools, embedded in the e-visit application, to aid in their appropriate adherence to the ABRS guideline at the point of care. Guideline adherence was measured again two months later using the ABRS guideline criteria. Comparison between the pre and post intervention adherence rates was performed by analyzing an electronic record data extract using descriptive statistics.
The patient population was limited to those seeking care via e-visits. Patients with serious medical conditions, such as congestive heart failure, and those with serious symptoms, such as severe headache pain, were triaged to receive care in a clinic or urgent care setting.
3.2 Intervention: Guideline Adherence Improvement Strategies
The performance-improvement project involved dissemination of current baseline provider performance for management of ABRS relative to the guideline to each of the providers (percentage adherence to the ABRS guideline in the e-visit setting), the implementation of an educational session on the ABRS guideline, and an ABRS-specific enhancement of the CDSS software functionality within the e-visit application. A description of the enhanced CDSS functionality was also included in an email communication to the providers.
The baseline review of provider ABRS guideline adherence included a two-month period, November through December 2013. A de-identified export of structured data for all ABRS e-visit encounters from the EHR for this time period was obtained. Inclusion criteria for the patient records included those who were assigned a diagnosis of ABRS, ICD 9 code 461.9, by e-visit providers. The data export was designed to include the patient symptom history, which was necessary to determine whether or not the patient met the criteria for ABRS. Key patient symptom data, derived from the structured patient interview, included separate columns for each of the symptoms. The columns were coded with basic labels: symptom duration (in days), URI symptom onset prior to facial pressure (yes/no), presence of sinus pressure (yes/no), (fever yes/no), or mild-to-moderate headache (yes/no). The structured data also included the assessment selected, by ICD 9 code, and treatment recommendations prescribed, specifically whether or not an antibiotic was prescribed, displayed in the prescription data field including the medication name, strength, dose, frequency, and duration. This report was sent to all participating providers; the performance measures included the number of ABRS e-visits performed by each of the participating providers including both individual and group aggregate measures of the percentage of cases managed according to the guidelines.
3.3 Educational Intervention
The ABRS educational intervention was delivered in two ways. First, the participating providers received a verbal reminder regarding the ABRS guideline at a mandatory in-person training session, which was an overall review and update of the e-visit initiative. Second, a brief email was sent to the same providers; it highlighted the key components of the ABRS guideline and described the soon-to-be-deployed enhancement of the CDSS, specific to the guideline. Updates to the CDSS included two changes. The structured patient history clinical note summary was modified so that the provider could see the duration (days) of symptoms text highlighted in red as CDSS for the provider. In addition, a very brief bullet-point summary of the ABRS guideline (based on ICSI, CDC, and IDSA) was added to the clinician screen, located in the visual workflow for the clinician to see while they were performing the review and clinical decision making for the e-visit patient.
3.4 Analysis
The structured data elements used to determine whether the clinician adhered to the guideline includes the following discrete components: duration of symptoms, fever, headache, sinus pressure, and bi-modal symptoms. The final data point is binary; it was tabulated in one of two categories as guideline adherence being met or not. The determination of adherence was based on criteria for a diagnosis of ABRS including duration of symptoms of seven days with two or more of the following symptoms: sinus pressure, worsening of pressure after initial improvement, fever, mild to moderate headache; or sinusitis symptoms for ten days or more. ► Figure 1 depicts the general workflow from patient interview, provider review and assessment of clinical summary, selection of diagnosis and treatment plan, and determination of adherence to the ABRS guideline.

Acute bacterial rhinosinusitis CDS workflow
The percentage change in guideline adherence performance from the first pre-intervention sample to the second post-intervention sample was calculated as well as statistical analysis using chi-square.
The results of the data analysis prior to the educational and CDSS interventions revealed a rate of guideline adherence of 95.25%. Measurement of ABRS guideline adherence post-intervention was 98.40%, a 3.30%, improvement in adherence to the guidelines, see ► Table 1 . Further analysis revealed that, in the pre-intervention group, duration of symptoms was the reason a case was not adherent to guidelines 80% of the time and 33.30% in the post-intervention group. A statistically significant change (p < .05) in provider adherence was found as evidenced by the 3.30% improvement from pre-intervention (15/301) to post-intervention (6/368) using chi-square analysis.
Adherence to ABRS guideline before and after intervention
5. Discussion
The interventions in this project included ABRS guideline performance feedback to participating providers, an educational intervention, and enhanced CDSS focused on evidence based guideline recommendations for ABRS management. With these three interventions, there was an increase in provider adherence in the use of ABRS clinical guideline. The improvement in provider guideline adherence, as measured by the percentage change between pre- and post-intervention guideline use, was modest at 3.30%. If these interventions were replicated with a larger sample size, the impact of a 3.30% improvement in ABRS guideline adherence on the estimated 31 million annual diagnoses of ABRS [ 6 ] would likely indicate a clinically significant improvement.
The data collected in this quality improvement project demonstrated that provider adherence to the ABRS may be improved with these interventions in the e-visit setting. These improvements could improve the rates of appropriate antibiotic prescribing and ultimately improve patient outcomes, such as reducing potential adverse events related to the medications and antibiotic resistance associated with overprescribing of these medications.
Since the mode of care delivery in this project was the e-visit, which is a relatively new care-delivery method, the quality improvement literature is limited in this area so comparison with other studies is limited.
One aspect of the findings that was not anticipated was that the baseline (pre-intervention) rates of guideline adherence for the treatment of ABRS for the health system were much higher than those reported in the literature. However, even though the health system baseline rate of guideline adherence was at 95.25%, leaving a limited opportunity for improvement, the health system had made improving antibiotic stewardship a priority and was committed to this project to demonstrate both baseline guideline adherence and possible improvements. In addition, providing care via e-visits was relatively new for the health system, and it was committed to both monitoring and improving the quality of care in this setting.
5.1 Limitations
There are several limitations to this project. First, this performance improvement in ABRS guideline adherence was specific to the e-visit setting at one health system and may not apply to other e-visit settings or to the traditional ambulatory care setting, such as primary care clinics, urgent care centers, or emergency departments. Second, there were no controls in this quality improvement project to conclude that the intervention caused the improvement; rather, an improvement was observed after the interventions. Third, the use of three interventions (performance feedback, education, and CDSS) make it impossible to determine whether one, two, or all three of the interventions were needed to achieve the results of successfully improving adherence to the ABRS clinical guideline. However, a meta-analysis of sepsis guideline compliance concluded that a combination of education and process improvement results in higher compliance, so it maybe that a combination of interventions in this study had an additive effect (Damiani, 2015). Fourth, participating providers may have individually participated in an educational event or pursued self-study related to ABRS guidelines and appropriate use of antibiotics in treating URIs, thereby being influenced by factors independent of the three interventions. Finally, this study did not measure whether the most appropriate antibiotics were selected when prescribed, another important component of antibiotic stewardship. Additional study of interventions to improve adherence to antibiotic prescribing guidelines is necessary.
6. Conclusions
The purpose of this project was to improve adherence to ABRS treatment guidelines in the e-health visit setting. After interventions with provider using feedback, education, and CDSS interventions, an improvement of 3.30% in adherence to the ABRS guideline was observed. This project demonstrates the potential influence of these interventions on provider performance related to clinical guideline adherence. Finally, the results of this project suggests that the intervention strategies utilized could be used to improve guideline adherence for other conditions in the e-visit setting as well as treatment of similar conditions in the traditional ambulatory care setting. There is the potential to improve clinical care and ultimately improve the safety and quality of care with these strategies. Future studies are needed to further investigate the use of specific individual quality improvement interventions versus the combined interventions used here. Future studies should also focus on definitions of clinically important outcomes to determine whether the outcomes are both statistically and clinically significant.
7. Clinical Relevance
The goal of this project was to evaluate the effectiveness of interventions, including education and CDSS, to improve provider adherence to ABRS clinical-practice guidelines in the e-visit setting. However, The improved guideline adherence may not represent a significant clinical impact given the modest sample size and study design. Additional studies are recommended involving health systems with greater differences in baseline guideline adherence performance measures. Also, further investigation is needed to compare the differences between and the use of a single intervention versus more than one intervention for improving adherence to guidelines.
8. Conflict of Interest
The authors have no conflict of interest to disclose with regards to this work. The authors report no external funding source for this project.
9. Protection of Human and Animal Subjects
This performance improvement project involved de-identified electronic medical record review. Human subject protection and approval was obtained through the University of Minnesota School of Nursing and the University of Minnesota Institutional Review Board (IRB) process.
Sinus Infection (Sinusitis)
Stuffy nose that just isn’t getting better? You might have a sinus infection, also called sinusitis
Antibiotics are not needed for many sinus infections, but your doctor can decide if you need an antibiotic.
Sinus infections happen when fluid builds up in the air-filled pockets in the face (sinuses). This fluid buildup allows germs to grow. Viruses cause most sinus infections, but bacteria can cause some sinus infections.
- Risk Factors
Several factors can increase your risk of getting a sinus infection:
- A previous cold
- Seasonal allergies
- Smoking and exposure to secondhand smoke
- Structural problems within the sinuses. For example, growths on the lining of the nose or sinuses, known as nasal polyps.
- A weak immune system or taking drugs that weaken the immune system
Common symptoms of sinus infections include:
- Stuffy nose
- Facial pain or pressure
- Mucus dripping down the throat (post-nasal drip)
- Sore throat
When to Seek Medical Care
How to feel better, over-the-counter medicine and children.
When you have a sinus infection, one or more of your sinuses becomes inflamed. Fluid builds up, which can cause congestion and runny nose.
Talk to a healthcare professional right away if your child is under 3 months old with a fever of 100.4 °F (38 °C) or higher.
See a doctor if you have:
- Severe symptoms, such as severe headache or facial pain.
- Symptoms that get worse after improving.
- Symptoms lasting more than 10 days without getting better.
- Fever longer than 3-4 days.
You should also seek medical care if you have had multiple sinus infections in the past year.
This list is not all-inclusive. Please see a doctor for any symptom that is severe or concerning.
Other conditions can cause symptoms similar to a sinus infection, including:
Your doctor will determine if you have a sinus infection by asking about symptoms and examining you.
Antibiotics are not needed for many sinus infections. Most sinus infections usually get better on their own without antibiotics. When antibiotics aren’t needed, they won’t help you, and their side effects could still cause harm. Side effects can range from mild reactions, like a rash, to more serious health problems. These problems can include severe allergic reactions, antibiotic-resistant infections and C. diff infection. C. diff causes diarrhea that can lead to severe colon damage and death.
However, in some cases, you may need antibiotics. Talk to your doctor about the best treatment for your illness.
For some sinus infections, your doctor might recommend watchful waiting or delayed antibiotic prescribing .
- Watchful waiting: Your doctor may suggest watching and waiting for 2-3 days to see if you need antibiotics. This gives the immune system time to fight off the infection. If your symptoms don’t improve, the doctor may prescribe an antibiotic.
- Delayed prescribing: Your doctor may prescribe an antibiotic but suggest that you wait 2–3 days before filling the prescription. You may recover on your own and may not need the antibiotic.
What antibiotics treat and won’t treat
Transcript [TXT – 294 B]
Below are some ways to help relieve sinus pain and pressure:
- Put a warm compress over the nose and forehead to help relieve sinus pressure.
- Use a decongestant or saline nasal spray.
- Breathe in steam from a bowl of hot water or shower.
Ask your doctor or pharmacist about over-the-counter medicines that can help you feel better. Always use over-the-counter medicines as directed.
Visit Sinus Rinsing for Health or Religious Practice for information on how to safely use a sinus rinse.
Carefully read and follow instructions on over-the-counter medicine product labels before giving medicines to children. Some over-the-counter medicines are not recommended for children of certain ages.
- Children younger than 6 months: only give acetaminophen.
- Children 6 months or older: it is OK to give acetaminophen or ibuprofen.
- Never give aspirin to children because it can cause Reye’s syndrome. Reye’s syndrome is a very serious, but rare illness that can harm the liver and brain.
- Children younger than 4 years old: do not use over-the-counter cough and cold medicines in young children unless a doctor specifically tells you to. Cough and cold medicines can result in serious and sometimes life-threatening side effects in young children.
- Children 4 years or older: discuss with your child’s doctor if over-the-counter cough and cold medicines are safe to give to your child.
Ask your doctor or pharmacist about the right dosage of over-the-counter medicines for your child’s age and size. Also, tell your child’s doctor and pharmacist about all prescription and over-the-counter medicines they are taking.
You can help prevent sinus infections by doing your best to stay healthy and keep others healthy, including:
- Clean your hands .
- Receive recommended vaccines, such as the flu vaccine and pneumococcal vaccine .
- Avoid close contact with people who have colds or other upper respiratory infections.
- Don’t smoke and avoid secondhand smoke.
- Use a clean humidifier to moisten the air at home.
To receive email updates about this page, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.

Online Sinus Infection Treatment
Online sinusitis, sinus pain relief, and doctor's note.
Sinus congestion or pain following a cold or severe allergies may indicate a sinus infection. Treatment with prescription medications, including antibiotics at times, will help speed your recovery. Ages 18-65.
Online sinus Infection treatment.
- Quick online doctor visits
- No appointment needed
- Complete your visit in minutes without video or voice calls
- Doxycycline
- Azithromycin
- Doctor's note only available with "Visit & Note" selection
What Causes a Sinus Infection?
- Viral infections (most common)
- Occur when sinuses are inflamed
- Symptoms that get better and then suddenly worsen may indicate that you have sinusitis
- Can lead to other very serious infections if left untreated
- Some sinus infections require antibiotic treatment
Who can benefit from this treatment?
- People with bacterial sinusitis who may require antibiotics
- People with uncomfortable sinus pressure
- Our physicians will determine if you need treatment with antibiotics or other medications and alert you if your symptoms may be due to something more serious
What can I expect?
- Our online assessment will help determine if you are a good candidate for treatment
- You may be prescribed an antibiotic and/or other medications
- Sometimes, based on your symptoms, it may be recommended that antibiotics be used in a delayed fashion, if needed.
- Just answer a few questions to get started with your online visit
Select a treatment or medical service on MDAnywhere.com
Begin by selecting one of our many available services. If you need some guidance, detailed descriptions of the services and their respective treatments or tests are available for your review. Consultation fees from $29.
Tell us about your visit including any symptoms and medical history
Our online assessments average 5 minutes and will determine if you are a good candidate for immediate medical care . We will never share your protected health information with anyone but your medical team.
Complete your health profile by entering contact, pharmacy and billing information
The medical team will review your visit after checkout and build a treatment plan which may include prescriptions, lab orders, aftercare instructions, and/or a doctor's note. They will contact you if more information is needed.
Remember to verify your email address/account by clicking on the MDAnywhere link in your inbox.
***You must verify your email address when your account is created***
The treatment team will contact you using our secure messaging system. Enable text messaging for the quickest service.
What happens next?
Creating an account and completing your visit:
- Create an MDAnywhere account at any time
- Answer a few medical interview questions and provide your medical history & billing information to complete your visit
- Remember, you do not need insurance or an appointment to complete your visit
- Once these two steps are complete AND you have received your treatment request confirmation, a physician will review your entire visit
- We share your treatment plan with you minutes once the physician reviews your request
- We notify you when any additional information is needed
After your visit is complete:
- Remember to routinely check for new messages in your patient portal because this will expedite your care
- You may message your doctor for up to 2 weeks after completing your treatment, in case you have any concerns
- The doctor sends prescriptions or vaccine orders electronically to your pharmacy
- Medication cost is NOT included and is thus charged directly by your pharmacy
- We send a visit summary with any new prescriptions (e.g. medication for a UTI or yeast infection), prescription refills or lab/vaccine orders directly to your portal
- Doctor's notes are sent to the Messages section of your portal by the end of the day, if not sooner
- Treatment for any additional health concern requires a separate visit
- We do not charge you when online treatment is not recommended
- We protect your private information, store it securely, and certainly keep it confidential (HIPAA compliant)
For a complete listing of all of our services, click the button below:
What we proudly are:.
MDAnywhere is an affordable, patient centered telemedicine service that provides quick visits and treatment. Basically, a modern healthcare alternative. Easy visits, expert care, and low, transparent fees are our top priorities. 100% of the consultations are with board certified physicians and provided without appointments.
The MDAnywhere difference:
MDAnywhere is here for YOU. Our team strives to prescribe the lowest cost options whenever possible and takes great pride in delivering care when it is convenient for you. Accordingly, we offer extended service hours and short response times. We are not a pharmacy, nor do we sell, deliver, or profit from pharmaceuticals.
The MDAnywhere team provides accessible medical care and extended hours every day! The medical team reviews requests from 7am - 1am EST every day of the year. All medical evaluations are provided by Access Medical Associates, PLLC.
The content displayed on this page is for informational purposes only and is not medical opinion or advice.
Thanks for visiting! GoodRx is not available outside of the United States. If you are trying to access this site from the United States and believe you have received this message in error, please reach out to [email protected] and let us know.
Sinus Infections

Sinus Infection Treatment
Get diagnosed by top-rated doctors for sinus infections. Learn about different treatment options, including medications and at-home remedies.
For: All ages Estimated wait time: 5 minutes or less
Who is this right for?
Patients with a sinus infection are usually looking for relief from their symptoms, such as nasal congestion, facial pain or pressure, headache, and sinus pressure.
Sinusitis symptoms
You are exhibiting sinus infection symptoms and are looking for fast relief.
Medications
You are able to take nasal spray, oral medications or antibiotics.
You want convenience
You’re looking for a convenient diagnosis and a cost-effective treatment.
Doctor On Demand is a covered benefit for over 98 million Americans. If you’re covered by your employer or insurance, then you’ll pay $0. No insurance, no problem. You can use Doctor On Demand starting at $89 per visit.

Here are a few of the commonly prescribed sinusitis medications that you might receive from your doctor.
- Antibiotics, such as Augmentin and Doxycycline
- Decongestants, like pseudoephedrine or phenylephrine, which can reduce inflammation in the sinuses
- Nasal corticosteroids, such as fluticasone or mometasone, which can help relieve symptoms such as postnasal drip
- Pain relievers, such as acetaminophen or ibuprofen
- Antihistamines, such as loratadine or cetirizine

During a visit for a sinus infection, patients can expect the clinician to:
They will ask about your symptoms, medical history, and any current medications.
You may be eligible to receive a same-day prescription; however, your doctor will meet with you to determine if you need additional testing.
They may prescribe antibiotics to treat the sinus infection—either during the visit or after the lab returns your testing results.
They may also recommend over-the-counter or prescription pain relievers to help manage the symptoms.
They may offer additional guidance on how to prevent a future sinus infection.

Getting ready for your sinus infection visit with Doctor On Demand:
- Find a comfortable and quiet space where you can speak freely about your symptoms.
- Pull all of your insurance information together (if you don’t have insurance, you can skip this step).
- Find a photo ID, like your driver’s license or passport.
- Set aside five to 10 minutes, so you can answer questions about your symptoms and health history.

Set up your account.
Once you finish registering, you’ll be able to see the cost of your visit.

See the next available provider or schedule your appointment.
Select your concern and answer a few questions to provide the doctor with some context.

Start your live virtual visit.
Meet with one of our board-certified doctors who will diagnose your symptoms and offer a custom treatment plan. If needed, you can get prescriptions delivered to you or sent to your local pharmacy.
"I finally did a televisit this morning and in 4 minutes and 35 seconds this wonderful doctor was able to see that I had strep throat and sinus issues. As a parent, time is very important and we don’t have much free time so this was a blessing for me to be able to get myself treated without the hassle of bringing all of my children into an urgent care with me and waiting for hours! Thank you!!!"
–Chelsea
"Very friendly and understanding of my symptoms! This was my first time using this, I was very impressed, just saved a lot of time and money by not having to go to the doctors office for a sinus infection. Will definitely be using this again. Thank you!"
–James
"I'm stuck at home, positive for COVID, which turned into a sinus infection. Doctor On Demand saved me a trip to urgent care and infecting others with COVID. Thank you!"

Top-rated providers
Get care from a team of doctors rated 4.9 out of 5 stars by patients just like you.

Same-day appointments, 24/7/365
Why wait to be seen? Connect to care in as little as 5 minutes.
Custom treatment plan
Get the right treatment option and prescription for your unique care needs.

Care at home or on the go
Connect with a provider from anywhere you have internet.
What is a sinus infection?
A sinus infection is an inflammation of the tissues in your sinuses. It can cause facial pain, a stuffy or runny nose, and often a fever plus other symptoms. It’s often caused by the common cold, but other viruses, bacteria, fungi or allergies can also cause a sinus infection. Bacterial infections, viral infections, or allergies can irritate your sinuses, causing them to get blocked and filled with fluid. In turn, this can cause pressure and pain in your face, nasal congestion, or other symptoms.
What are the typical symptoms of a sinus infection?
Typical symptoms of a sinus infection include postnasal drip, runny nose with thick yellow or green mucus, stuffy nose, facial pressure, pressure or pain in your teeth, ear pressure or pain, fever, bad breath or a bad taste in your mouth, cough, headache, or tiredness.
Do I have to take an antibiotic prescription to get rid of my sinus infection?
No. Doctors will often wait to see how long your symptoms last before prescribing antibiotics since some sinus infections are caused by viruses, and viral infections cannot be cured with antibiotics. Your doctor will also want to make sure a patient isn’t overusing antibiotics, which can make future infections harder to treat.
What causes a sinus infection?
A sinus infection, or sinusitis, is an inflammation or swelling of the tissue that lines the sinuses. When sinuses become blocked and filled with fluid, it allows viruses, bacteria, or fungi to grow more easily and cause an infection. Many s inus infections are often a result due to viruses, allergies, environmental exposures, and bacteria.
How do you treat a sinus infection?
Understanding the symptoms of sinusitis is important to help determine the best treatment. You can manage your symptoms with home remedies like nasal sprays, hydration, rest, and using humidifiers. However, if you have questions about symptoms or if they last more than seven to ten days, you may need to see a doctor.

When to Go to the ER for Sinus Infection
When to Go to the ER
Nov 27, 2016

A sinus infection (sinusitis) comes with loads of awful and draining symptoms. Of course anyone with a sinus infection is uncomfortable, but how do you know when a sinus infection becomes a serious issue? While it is true that most sinus infections clear up on their own in a few days, if left unchecked, a sinus infection can lead to serious medical complications.
When to Go to the ER for Sinus Infection (Sinusitis)
Below are some signs to watch out for that may indicate a sinus infection is more serious, and medical attention is required.
1. High Fever
Having a fever when fighting an infection, including a sinus infection, is completely normal. The elevated temperature is expected as the body burns fluids to combat the infection. What isn’t normal though, is anything over 100.5 F. Having a higher temperature may indicate that the infection has spread to other parts of the body, and you may need medication to control the infection.
2. Severe Pain
Undoubtedly with a sinus infection, there is going to be some pressure and discomfort, but if the pain gets severe, it is time to see a doctor. A sinus infection becomes very serious if there is severe pain in the eyes, throat, ears, or head. The infection can easily spread to create an eye or ear infection. The sinus infection can also spread to the lining of the brain, which becomes a very serious condition known as meningitis.
3. Chronic Sinus Infections
Typically, a sinus infection clears up in a few days to a week. When the infection lasts longer though, the sinus infection becomes serious. A sinus infection is classified as chronic once it has lasted for four weeks or longer.
Having a chronic sinus infection can mean that there is a bigger, underlying problem that may be causing the infection in the first place. Having a constant infection could also lead to more serious infections developing. If your sinus infection lasts for four weeks or longer it is time to see a doctor so the infection does not turn into something more serious.
Visit Complete Care
Even if a sinus infection has just started, it is never a bad idea it still may be necessary to seek emergency care. Complete Care has multiple ER locations across Texas, meaning an ER is always just minutes away.
Share this on
- Case report
- Open access
- Published: 05 April 2024
Acute invasive fungal sinusitis with orbital tip syndrome in patients on long-term use of ruxolitinib: a case report
- Zhiyuan Tang 1 &
- Zhaohui Shi 2 , 3
Journal of Medical Case Reports volume 18 , Article number: 199 ( 2024 ) Cite this article
61 Accesses
1 Altmetric
Metrics details
Introduction
A long-term ruxolitinib-treated patient with primary myelofibrosis, who was co-infected with aspergillosis infection during a short period, developed acute invasive fungal sinusitis with consequent orbit apex syndrome. This may be the first reported case in the world.
This is a 75-year-old Chinese man; the patient was admitted with 2-month history of headache accompanied by numbness and 8-day history of vision loss. The preliminary clinical diagnoses were suspected acute invasive fungal sinusitis or adenoid cystic carcinoma. We performed endoscopic debridement and antifungal therapy. About 90 days after surgery, magnetic resonance imaging revealed no recurrence of pathological tissue.
One of the bases for the occurrence of invasive fungal sinusitis may be the patient’s long-term use of ruxolitinib for essential thrombocythemia. Some patients with invasive fungal sinuses have atypical nasal symptoms and are referred to the corresponding departments with eye and headache as the first symptoms. It is suggested that enhanced magnetic resonance imaging should be performed at an early stage. Surgical treatment in combination with antifungal and enhanced immunotherapy can effectively prevent the spread of infection and reduce the risk of death.
Peer Review reports
Case presentation
Ruxolitinib is a novel potent biologic agent that inhibits Janus kinase 1 (JAK1) and Janus kinase 2 (JAK2), reserved for patients with myeloproliferative diseases [ 1 ]. Although it is effective and improves survival in such patients, the immunosuppressive agent may increase the risk of acquiring opportunistic infections. However, very little data are available regarding the infectious complications while on this agent. Previous studies have reported bacteria, Mycobacterium tuberculosis , Cryptococcus neoformans , Pneumocystis jirovecii , herpes simplex, and varicella-zoster virus to be etiologic agents that had been isolated from patients receiving ruxolitinib [ 2 ]. Here, we report a long-term ruxolitinib-treated patient with primary myelofibrosis, who was coinfected with aspergillosis infection during a short period and developed acute invasive fungal sinusitis with consequent orbit apex syndrome.
Patient information
This is a 75-year-old Chinese man; the patient was admitted with a 2 month history of headache accompanied by numbness and an 8 day history of vision loss.
From November 2021 onward, the patient experienced right-sided toothache and sought treatment at other hospitals. Computed tomography (CT) examination suggested possible temporomandibular joint (TMJ) disorder; however, conservative management proved ineffective as the patient developed persistent swelling pain and unbearable temporal pain. Subsequently, he was admitted to the pain department where he received a diagnosis of TMJ pain and trigeminal neuralgia.
After conservative treatment proved ineffective and the patient experienced persistent head and facial numbness, as well as gradually worsening head and facial pain that became unbearable, they sought medical attention at multiple hospitals but were unable to receive a proper diagnosis or effective symptomatic treatment. In mid-November, the above-mentioned symptoms significantly exacerbated, accompanied by intermittent confusion. The diagnosis was great occipital neuralgia in the pain department for localized treatment followed by minimally invasive surgery.
Although head and facial pain were substantially alleviated, numbness gradually intensified while swelling, protrusion, and decreased vision manifested in the right eye. In early January 2022, he was admitted to the ophthalmology hospital owing to a decrease in visual acuity in his right eye. The orbital CT scan revealed bilateral proptosis without evidence of extraocular muscle thickening. Sinus magnetic resonance imaging (MRI) demonstrated inflammation in the right maxillary, bilateral ethmoid, and sphenoidal sinuses with increased orbital fat.
The right eye experienced a loss of light sensation and subsequently became blind within a few days. He was admitted with the diagnosis of “a space-occupying lesion in the infratemporal fossa and skull base: suspected acute invasive fungal sinusitis and adenoid cystic carcinoma" and “orbital apex syndrome (right).” The patient was diagnosed with thrombocythemia in 2006 and was initially treated with hydroxyurea for 10 years. Since 2017, he had received ruxolitinib for the treatment of myelofibrosis for 4 years. He had received long term blood transfusions with diabetes denial.
Clinical findings
Physical examination revealed stable vital signs, including a temperature of 36.5 °C and a normal level of consciousness. The right eyelid was droopy, swollen, and could not elevate properly, accompanied by a bulging eyeball, conjunctival chemosis, and a transparent cornea. The pupil of the right eye was dilated by 5 mm, and the right direct and indirect reflexes were lost. The pupil size of the left eye was 3 mm, with normal reflexes. The right middle face and upper lip were numb, while the sensation from the tongue and in the lower lip was normal (Fig. 1 ). Examination of the nose revealed a pale nasal mucosa, swelling of both inferior turbinates, and no secretion or lump. An internal endoscopic examination of the nose showed a deviated nasal septum, dilation of vessels, swelling of the mucosa in the nasopharynx, and a lump with a smooth surface arising from the roof and posterior wall of the nasopharynx.
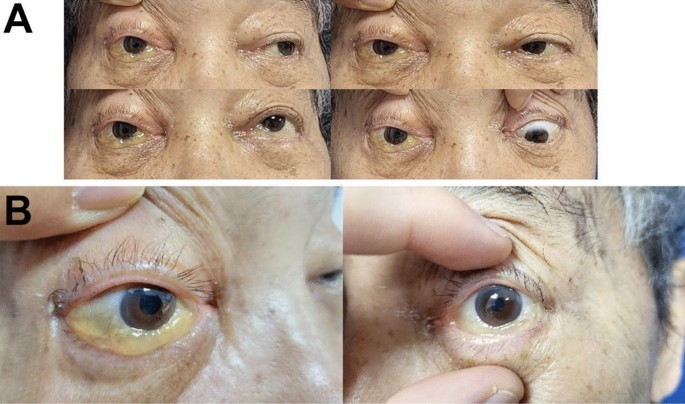
Eye examination of patients before surgery
Magnetic resonance imaging (MRI) scan of the sinuses indicated a right maxillary and sphenoid lesion extending to the pterygopalatine fossa, orbital apex, infratemporal fossa, extraconal fat, right cavernous sinus, and meninges situated in the bilateral anterior and middle skull base (Fig. 2 B). We suspected neoplasms (adenoid cystic carcinoma) and chronic invasive fungal sinusitis. The random blood glucose level was between 7.42 and 9.56 mmol/L. Urinalysis revealed that the amount of glucose in urine was more than 1 mmol/L. Glycated hemoglobin was more than 6.0%. Combined with the medical history, the preliminary clinical diagnoses were as follows: (1) a space-occupying lesion in the infratemporal fossa and skull base: suspected acute invasive fungal sinusitis or adenoid cystic carcinoma; (2) orbital apex syndrome (right); (3) severe anemia; (4) myelofibrosis; and (5) diabetes.
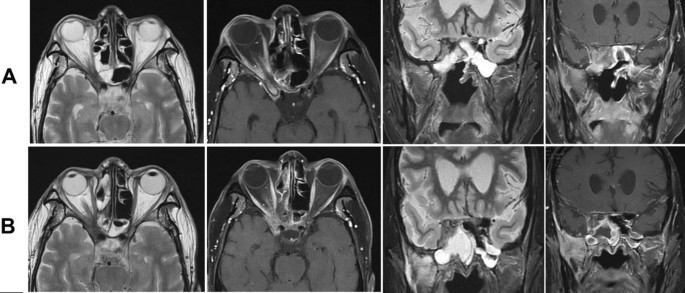
Comparison of magnetic resonance images of the sinuses before and after treatment: A 3 months after treatment; B before treatment
Therapeutic and intervention
The preoperative evaluation was done before undergoing endoscopic sinus surgery. The endoscopic transethmoidal sphenoidotomy with maxillary antrostomy was performed for surgical excision of lesions, which were suspected to be located on the right side of the pterygopalatine fossa, infratemporal fossa, skull base, orbital apex, or cavernous sinus, accompanied by the partial removal of the right middle turbinate, right medial orbital wall, right maxillary bone, and right inferior turbinate bone.
During surgery, fungal balls were seen in the maxillary sinus with evident edema of the sinus mucosa. Bone fragments of the maxillary sinus posterior wall and the lateral orbital wall were broken off. Necrosis was seen in the lateral pterygoid muscle and numerous soft tissue masses, and purulent discharge was visible in the tissue spaces. The necrotic bone of the pterygopalatine fossa eroded through the inferior orbital fissure and extended to the orbital floor and orbital apex. Apart from necrosis of the maxillary nerve, the lesion led to muscle necrosis and the extension of the fracture from the inferior and medial walls of the orbit to the orbital apex, where necrosis of the muscle fascia and orbital contents was partially observable.
Through the right optic canal, a pale and necrotic optic nerve was found. Combined with intraoperative and postoperative fungal antigen detection in blood and tissue (Fig. 3 ). Postoperatively, the patient was treated with ceftriaxone at 2.0 g/day, voriconazole at 400 mg/day (200 mg twice a day) on the first day [followed by 200 mg/day (100 mg twice a day)], and human immunoglobulins at 10 g/day. At 5 days after surgery, he was referred to the division of hematology to continue antifungal treatments for myelofibrosis.
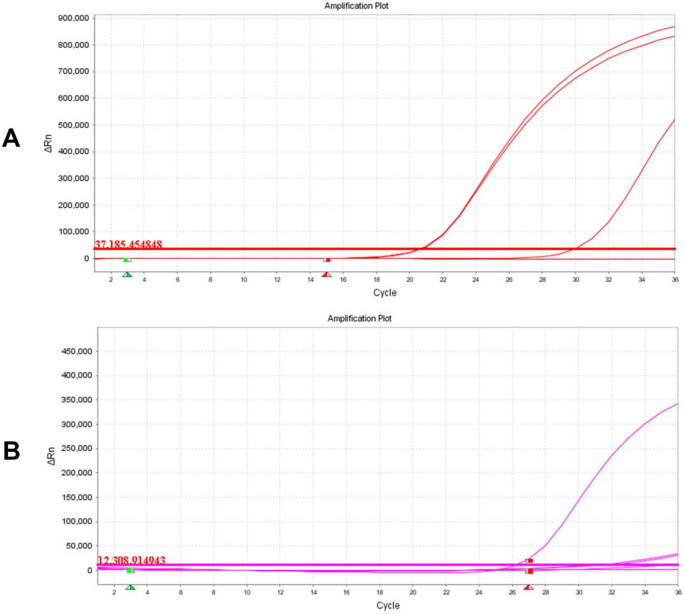
DNA of pan Aspergillus detected in diseased tissue: A pan Aspergillus detection curve; B internal extraction control DNA detection curve
Follow-up and outcomes
Oral voriconazole was continued after surgery. About 90 days after surgery, the MRI revealed no recurrence of pathological tissue (Fig. 2 A). The upper eyelid of the affected eye was able to be fully elevated, and conjunctival edema resolved; however, regrettably, the patient’s right pupil dilated by 5 mm, and the elimination of both direct and indirect light reflections was observed, resulting in complete loss of vision (Fig. 4 ). This may be attributed to the rapid progression of acute invasive fungal rhinosinusitis resulting in misdiagnosis during the early stages and irreversible optic nerve damage.

Eye examination of patients about 90 days after surgery
Discussion and conclusion
Fungi produce large numbers of asexual spores called conidia that are released into the air. Humans inhale hundreds to thousands of these infectious propagules every day. In immunocompetent individuals, the cooperation of the respiratory epithelium, lung-resident macrophages, and recruited neutrophils and monocytes clear conidia efficiently. However, in immunocompromised states, it can lead to invasive fungal infections. It has been reported that in patients with myelofibrosis, the hazard ratio of bacterial infections was 1.9 times as high as that of normal people, viral infections were 2.1 times as high, and fungal infections were the highest at about 2.9 times [ 3 ].
Myelofibrosis, belonging to a group of diseases called myeloproliferative disorders, is a type of blood cancer characterized by chronic hematologic malignancies [ 3 , 4 ]. The deregulation of the JAK/signal transducers and activators of transcription pathway leads to myelofibrosis that can be treated by ruxolitinib. However, a growing body of clinical data suggests that ruxolitinib exerts potent anti-inflammatory and immunosuppressive effects [ 5 ], interferes with the signaling of several cytokines and growth factors associated with the immune system, and decreases levels of proinflammatory cytokines in patients with myelofibrosis [ 6 ]. Furthermore, several studies indicate that ruxolitinib is associated with Treg cell-mediated downregulation, impaired dendritic cell function [ 7 , 8 , 9 , 10 ], and reduction in natural killer (NK) cell numbers. Although the exact relationship between its effects on immune function and the incidence of infection remains to be elucidated, these immunosuppressive mechanisms may contribute to the increased risk of infection in patients treated with ruxolitinib. A study conducted by Polverelli et al . of 507 patients with myelofibrosis showed a 15% correlation between the use of ruxolitinib and aspergillosis as well as other severe infections [ 11 ]. Nevertheless, no cases of acute invasive fungal sinusitis owing to aspergillosis in patients with myelofibrosis with ruxolitinib treatment have been reported in literature.
The patient in this case had a history of myelofibrosis with long-term ruxolitinib treatment, which may have been the main cause of acute invasive fungal sinusitis.
Orbital apex syndrome is a rare ocular complication usually resulting from infection, inflammation, neoplasms, and vascularity, which can lead to damage to the superior orbital fissure and optic canal, resulting in optic nerve dysfunction. Immunocompromised patients, such as those with diabetes or receiving immunosuppressive drugs, are susceptible to fungal infections. Orbital apex syndrome owing to aspergillosis has been reported in an immunocompromised patient with persistent methylprednisolone treatment during chemotherapy for metastatic colorectal cancer [ 12 , 13 ]. However, no cases of orbital apex syndrome caused by aspergillosis have been reported in patients undergoing long-term treatment with ruxolitinib.
The patient typically presented with proptosis, rapid vision loss leading to eventual blindness, visual fixation, a 5 mm dilated pupil in the right eye, loss of direct and indirect light reflexes, and droopy eyelids. On the other hand, the head MRI identified multiple foci on both sides of the face and cavernous sinuses, as well as the right side of the sphenoid sinus, ethmoid sinus, temporal lobe, and retrobulbar space. Infectious lesions and abscesses were diagnosed on the basis of the former comprehensive investigation. We found that the extension of fungal infection from the sinuses to the orbital apex was the pivotal reason for orbital apex syndrome in this case, with the disease progressing aggressively.
In this case, aspergillosis was generally caused by Aspergillus niger , Aspergillus fumigatus , and Aspergillus flavus . The lesion extended to the orbital apex resulting in orbital apex syndrome, thus making the condition complex and difficult to treat. In terms of treatment, we suggested that early surgical intervention was of paramount importance. Prompt surgical care after the patient’s admission and investigations, as well as timely removal of fungal masses and necrotic tissue from the nasal cavity and sinuses, is the key to treatment, which can effectively limit the further extension of the infection. Early empirical antifungal treatment and debridement can potentially reduce morbidity and mortality [ 14 ]. Antifungal agents that have been reported to be used successfully include itraconazole and fluconazole to treat aspergillosis [ 15 ]. However, patients with myelofibrosis have associated autoimmunity and hypoproteinemia, which contribute to aspergillosis. Hence, simultaneous enhancement of patient immunity in treatment with combination antifungal therapy of voriconazole with human immunoglobulins significantly strengthens the anti- Aspergillus effects.
In spite of timely surgery and 6 weeks of antifungal treatment, it is still difficult to predict prognosis. After discharge, computed tomography (CT) scans should be performed every 3–4 months, as well as nasal endoscopy every 2–3 months, to check for local recurrence or recurrence of lesions in the eye, brain, and adjacent organs [ 16 ].
From the experience of this case, we have learned that we should carefully evaluate the possible potential risk of infection before ruxolitinib initiation. Currently, this is the first case of aspergillosis with acute invasive fungal sinusitis in a patient undergoing treatment with ruxolitinib for primary myelofibrosis. This case highlights the possibility of acute invasive fungal sinusitis with more serious complications in immunosuppressed patients, especially those receiving long-term ruxolitinib treatment.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Dioverti MV, Abu Saleh OM, Tande AJ. Infectious complications in patients on treatment with ruxolitinib: case report and review of the literature. Infect Dis (Lond). 2018;50(5):381–7. https://doi.org/10.1080/23744235.2017.1390248 .
Article CAS PubMed Google Scholar
Landtblom AR, Andersson TM, Dickman PW, Smedby KE, Eloranta S, Batyrbekova N, Samuelsson J, Björkholm M, Hultcrantz M. Risk of infections in patients with myeloproliferative neoplasms-a population-based cohort study of 8363 patients. Leukemia. 2021;35(2):476–84. https://doi.org/10.1038/s41375-020-0909-7 . ( Epub 2020 Jun 16 ).
Barbui T, Thiele J, Gisslinger H, Finazzi G, Vannucchi AM, Tefferi A. The 2016 revision of WHO classification of myeloproliferative neoplasms: clinical and molecular advances. Blood Rev. 2016;30:453–9.
Hultcrantz M, Ravn Landtblom A, Andreasson B, Samuelsson J, Dickman PW, Kristinsson SY, et al . Incidence of myeloproliferative neoplasms—trends by subgroup and age in a population-based study in Sweden. J Intern Med. 2020;287:448–54.
Article CAS PubMed PubMed Central Google Scholar
McLornan DP, Khan AA, Harrison CN. Immunological consequences of JAK inhibition: friend or foe? Curr Hematol Malig Rep. 2015;10(4):370–9.
Article PubMed Google Scholar
Quintas-Cardama A, Kantarjian H, Cortes J, et al . Janus kinase inhibitors for the treatment of myeloproliferative neoplasias and beyond. Nat Rev Drug Discov. 2011;10(2):127–40.
Heine A, Brossart P, Wolf D. Ruxolitinib is a potent immunosuppressive compound: is it time for anti-infective prophylaxis? Blood. 2013;122(23):3843–4.
Heine A, Held SA, Daecke SN, et al . The JAK-inhibitor ruxolitinib impairs dendritic cell function in vitro and in vivo. Blood. 2013;122(7):1192–202.
Lussana FD, Ianni M, Rambaldi A. Tregs: hype or hope for allogeneic hematopoietic stem cell transplantation? Bone Marrow Transplant. 2017;52:1225–32.
Massa M, Rosti V, Campanelli R, et al . Rapid and long-lasting decrease of T-regulatory cells in patients with myelofibrosis treated with ruxolitinib. Leukemia. 2014;28(2):449–51.
Polverelli N, Breccia M, Benevolo G, et al . Risk factors for infections in myelofibrosis: role of disease status and treatment. A multicenter study of 507 patients. Am J Hematol. 2017;92:37–41. https://doi.org/10.1002/ajh.24572 .
Miyamoto Y, Sakamoto Y, Ohuchi M, Tokunaga R, Shigaki H, Kurashige J, Iwatsuki M, Baba Y, Yoshida N, Watanabe M, Baba H. Orbital apex syndrome caused by invasive aspergillosis as an adverse effect of systemic chemotherapy for metastatic colorectal cancer: a case report. Anticancer Res. 2016;36(2):821–3.
CAS PubMed Google Scholar
Willermain F, Bradstreet C, Kampouridis S, et al . Different presentations of ophthalmic aspergillosis. Eur J Ophthalmol. 2008;18(5):827–30.
Yuan M, Tandon A, Li A, Johnson E, Greer C, Tooley A, Tran AQ, Godfrey KJ, Dinkin M, Oliveira C. Orbital apex syndrome secondary to invasive aspergillus infection: a case series and literature review. J Neuroophthalmol. 2021;41(4):e631–8. https://doi.org/10.1097/WNO.0000000000001105 .
Farina C, Gotti E, Mouniée D, Boiron P, Goglio A. Phaeoacremonium parasiticum subcutaneous infection in a kidney-transplanted patient successfully treated by surgery. Transpl Infect Dis. 2007;9:253–5. https://doi.org/10.1111/j.1399-3062.2007.00206.x .
Biswas SS, Al-Amin Z, Razib FA, Mahbub S. Acute invasive fungal rhinosinusitis: our experience in immunocompromised host. Mymensingh Med J. 2013;22(4):814–9.
Download references
Acknowledgements
Ms.Yanjie Luo and Ms. Xiaoyi Liu provided professional translation and editing services.
Shenzhen Science and Technology Program (Grant No. JCYJ20210324121413037).
Special Fund for Economic and Technological Development of Longgang District, Shenzhen (Grant No. LGKCYLWS2021000029).
Sanming Project of Medicine in Shenzhen (SZSM202003003).
Shenzhen Science and Technology Plan funded key basic research projects of Shenzhen Science and Technology Innovation Commission (JCYJ20200109114244249).
These funds supported the collection and analysis of case data, surgical procedures, patient follow-up, and translation and editing services.
Author information
Authors and affiliations.
Department of Otolaryngology Head and Neck Surgery, Shenzhen University General Hospital, Shenzhen, 518055, China
Zhiyuan Tang
Department of Otorhinolaryngology-Head and Neck Surgery, Department of Allergy, Naso-Orbital-Maxilla and Skull Base Center, The Third Affiliated Hospital of Sun Yat-sen University, Guangzhou, 510630, Guangdong, China
Zhaohui Shi
Departmentof Otolaryngology, Shenzhen Longgang Otolaryngology Hospital & Shenzhen Otolaryngology Research Institute, Shenzhen, 518172, Guangdong, China
You can also search for this author in PubMed Google Scholar
Contributions
Z.T collated and analyzed the case data. Z.S performed the surgery and followed up the patient after surgery. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Zhaohui Shi .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Informed consent
The patient gave verbal informed consent.
Competing interests
Additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Tang, Z., Shi, Z. Acute invasive fungal sinusitis with orbital tip syndrome in patients on long-term use of ruxolitinib: a case report. J Med Case Reports 18 , 199 (2024). https://doi.org/10.1186/s13256-024-04486-3
Download citation
Received : 11 January 2024
Accepted : 01 March 2024
Published : 05 April 2024
DOI : https://doi.org/10.1186/s13256-024-04486-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Acute invasive fungal sinusitis
- Orbital tip syndrome
- Ruxolitinib
Journal of Medical Case Reports
ISSN: 1752-1947
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

I have chronic sinus infection
I have been having cold and catarrh for the past few weeks. On my last visit to the doctor, I was diagnosed with Sinusitis. Although my doctor tried to explain what this is, I would still appreciate it if you can explain what it is.
Sulaiman (by SMS)
Sinus infection (Sinusitis) is an inflammation of the sinuses – the air-filled cavities around your nose, eyes, and cheeks. It can be caused by viruses, bacteria, fungi, or allergies.
Symptoms like facial pain, congestion, nasal discharge, headaches, cough, fatigue, and a reduced sense of smell. Acute sinusitis lasts a short time, while chronic sinusitis persists for more than 12 weeks. Common causes include respiratory infections, nasal polyps, or a deviated septum.
In addition to medications prescribed by your doctor, hot steam inhalation with some life style changes will also go a long way in the cure of the Sinusitis.
Abuja doctor reveals unique way to permanently cure weak erection, small and shameful manhood and infertility issues without side effects within a short period. Click now to see!!

IMAGES
VIDEO
COMMENTS
Sinus infections (acute sinusitis). Upper respiratory illness. UTIs (urinary tract infections).** ... * Adults only. ** Women and adults assigned female at birth (AFAB) only. Scheduled Virtual Visit: This is an appointment with your primary care physician or specialist that's scheduled in advance — like a regular in-person appointment ...
When you or your child isn't feeling well, e-visits can get you a quick diagnosis, 24/7. You'll fill out a questionnaire about your symptoms and a telemedicine provider will evaluate your condition and share a treatment plan - all by messaging you within an hour. For minor illnesses like back pain, cold symptoms and urinary infections, an e ...
During the visit, Dr. Patel reviews your medical history and asks you specific questions that help him determine if you have a sinus infection. Based on your own history and your responses, he determines what course of action is needed. Following are common symptoms of a sinus infection: Runny nose; Closed or partially closed nasal passages
You should see a doctor if you still have sinusitis symptoms after a week or if they return more than a few times within a year. You should also see a doctor as soon as possible if the infection worsens. Signs of a worsening sinus infection include: fever. increase in pain or the pain spreads. over-the-counter pain medications do not relieve ...
We make it easy to get the online care you need for sinus infections, UTIs, pink eye and more - wherever you are. Health issues don't follow a 9-5 schedule, and neither do we. Day or night, visit Virtuwell's online clinic for diagnosis, treatment and prescriptions - no appointment or video needed.
sinus infection; stye (eyelid bump) sunburn; swimmer's ear; tick bite; tinea (fungal skin infection) urinary problems; urinary tract infection (UTI) ... Your eVisit costs $49, which will be billed after the visit, and may be covered by insurance. You'll enter your payment information after completing a short questionnaire. Some conditions ...
Use a warm compress. A warm compress on the nose and forehead might help lessen pressure in the sinuses. Keep sinuses moist. Breathing in the steam from a bowl of hot water with a towel over the head might help. Or take a hot shower, breathing in the warm, moist air. This will help ease pain and help mucus drain.
A comparison of care at e-visits and physician office visits for sinusitis and urinary tract infection. JAMA Intern Med. 2013;173(1 ... including demographic characteristics of all patient users. We assessed e-visit success outcomes by evaluating follow-up care seeking within 72 hours and 7 days after the e-visit, including associated ...
Common symptoms of a sinus infection include: Postnasal drip (mucus dripping down your throat). Runny nose with thick yellow or green mucus. Stuffy nose. Facial pressure (particularly around your nose, eyes and forehead). This might get worse when you move your head around or bend over. Pressure or pain in your teeth.
Symptoms. Acute sinusitis symptoms often include: Thick, yellow or greenish mucus from the nose, known as a runny nose, or down the back of the throat, known as postnasal drip. Blocked or stuffy nose, known as congestion. This makes it hard to breathe through the nose. Pain, tenderness, swelling and pressure around the eyes, cheeks, nose or ...
Of the 5165 visits for sinusitis, 465 (9%) were e-visits. Of the 2954 visits for UTI, 99 were e-visits (3%). Physicians were less likely to order a UTI-relevant test at an e-visit (8% e-visits vs 51% office visits; P < .01) . Few sinusitis-relevant tests were ordered for either type of visit.
In a study comparing e-visits (an online interaction between a health care provider and a patient) and office visits for ABRS and urinary tract infections (UTIs), Mehrotra et al. demonstrated a slightly higher adherence to specific antibiotic prescribing per guideline recommendation for ABRS via e-visit (70%) versus in-person clinic visits (67% ...
Services & Specialties. E-Visit. Get fast medical care—anytime anywhere—for 20 common conditions. Essentia E-Visit makes it easy and convenient for you to get the care you need from an Essentia Health provider online. Best of all, an E-Visit only costs $30. And, if you don't get a diagnosis and treatment plan within 60 minutes, your visit ...
Put a warm compress over the nose and forehead to help relieve sinus pressure. Use a decongestant or saline nasal spray. Breathe in steam from a bowl of hot water or shower. Ask your doctor or pharmacist about over-the-counter medicines that can help you feel better. Always use over-the-counter medicines as directed.
Prevention. One of the most effective ways to avoid a sinus infection or other upper respiratory infection is to keep your hands away from your face. You also want to wash your hands often with hot, soapy water (be sure to rub your hands together, clean under your nails, use lots of soap, wash for at least 20 seconds, and dry your hands ...
Sinus pain after a cold can be signs of a sinus infection. Sinus infection antibiotics are sometimes needed to prevent more serious issues. Menu . 1-800-632-4981; Mission; Team; How it Works; Health Blog; FAQ; ... We send a visit summary with any new prescriptions (e.g. medication for a UTI or yeast infection), prescription refills or lab ...
Sinus infections or sinusitis happen from time to time, but find out when you should see an otolaryngologist (ear, nose, and throat doctor) for help. Otolaryngologists are commonly known as ENTs (ears, nose, and throat doctors). Often, you can get treatment for a sinus infection from your primary care provider or at urgent care.
A sinus infection, or sinusitis, is an inflammation or swelling of the tissue that lines the sinuses. When sinuses become blocked and filled with fluid, it allows viruses, bacteria, or fungi to grow more easily and cause an infection. Many s inus infections are often a result due to viruses, allergies, environmental exposures, and bacteria.
A tear duct infection. Dacryocystitis is an infection of the tear ducts that can happen when (you guessed it) your bacterial sinus infection travels toward your eyes. Symptoms include eye pain ...
Below are some signs to watch out for that may indicate a sinus infection is more serious, and medical attention is required. 1. High Fever. Having a fever when fighting an infection, including a sinus infection, is completely normal. The elevated temperature is expected as the body burns fluids to combat the infection.
Hold a warm compress over the nose, forehead, or ear to help relieve pain or pressure. Place a cold cloth over the ear. Use an over-the-counter (OTC) decongestant to clear excess fluid buildup ...
A long-term ruxolitinib-treated patient with primary myelofibrosis, who was co-infected with aspergillosis infection during a short period, developed acute invasive fungal sinusitis with consequent orbit apex syndrome. This may be the first reported case in the world. This is a 75-year-old Chinese man; the patient was admitted with 2-month history of headache accompanied by numbness and 8-day ...
Sinus infection (Sinusitis) is an inflammation of the sinuses - the air-filled cavities around your nose, eyes, and cheeks. It can be caused by viruses, bacteria, fungi, or allergies.