- Introduction
- Conclusions
- Article Information
Patient self-scheduling capability first added to the Kaiser Permanente Northern California patient portal in 2016.
A, Video visit vs clinic visit comparison. B, Telephone visit vs clinic visit comparison. SES indicates socioeconomic status.
A, Video visit vs clinic visit comparison. B, Telephone visit vs clinic visit comparison.
eFigure. Number of Patient-Scheduled Primary Care Telephone Visits, by Quarter
- Payment Reforms to Incentivize Innovations in Home-Based Care JAMA Viewpoint June 23, 2020 This Viewpoint discusses the need for new payment models to incentivize innovations in personalized home care and facilitate transitions already occurring in response to the COVID-19 pandemic, and to develop lower-cost higher-quality approaches to home-based management of chronic illnesses such as heart failure and Parkinson disease. Kevin G. Volpp, MD, PhD; Susan M. Diamond, CPA; William H. Shrank, MD, MSHS

See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Reed ME , Huang J , Graetz I, et al. Patient Characteristics Associated With Choosing a Telemedicine Visit vs Office Visit With the Same Primary Care Clinicians. JAMA Netw Open. 2020;3(6):e205873. doi:10.1001/jamanetworkopen.2020.5873
Manage citations:
© 2024
- Permissions
Patient Characteristics Associated With Choosing a Telemedicine Visit vs Office Visit With the Same Primary Care Clinicians
- 1 Kaiser Permanente Division of Research, Oakland, California
- 2 Rollins School of Public Health, Emory University, Atlanta, Georgia
- 3 The Permanente Medical Group, Oakland, California
- 4 University of California at Berkeley, Berkeley
- Viewpoint Payment Reforms to Incentivize Innovations in Home-Based Care Kevin G. Volpp, MD, PhD; Susan M. Diamond, CPA; William H. Shrank, MD, MSHS JAMA
Question Which patient characteristics are associated with choosing either a telemedicine visit or an office visit with the same primary care clinician?
Findings In this cross-sectional study of data from 1.1 million patients with 2.2 million primary care visits, 14% of visits were scheduled as telemedicine (primarily by telephone), with patients more likely to choose telemedicine with their personal primary care clinician. Patient demographic characteristics, and office visit barriers were significantly associated with choosing telemedicine.
Meaning This study suggests a nuanced context for patient choice between a telemedicine visit and an office visit; the associations identified in this study may indicate opportunities for engagement with mobile technology access for those who face barriers to in-person visits.
Importance Video or telephone telemedicine can offer patients access to a clinician without arranging for transportation or spending time in a waiting room, but little is known about patient characteristics associated with choosing between telemedicine or office visits.
Objective To examine patient characteristics associated with choosing a telemedicine visit vs office visit with the same primary care clinicians.
Design, Setting, and Participants This cross-sectional study included data from 1 131 722 patients who scheduled a primary care appointment through the Kaiser Permanente Northern California patient portal between January 1, 2016, and May 31, 2018. All completed primary care appointments booked via the patient portal were identified. Only index visits without any other clinical visits within 7 days were included to define a relatively distinct patient-initiated care-seeking episode. Visits for routine physical, which are not telemedicine-eligible, were excluded. Data were analyzed from July 1, 2018, to December 31, 2019.
Main Outcomes and Measures Patient choice between an office, video, or telephone visit. Relative risk ratios (RRRs) for patient sociodemographic characteristics (age, sex, race/ethnicity, neighborhood socioeconomic status, language preference), technology access (neighborhood residential internet, mobile portal use), visiting the patient’s own personal primary care clinician, and in-person visit barriers (travel-time, parking, cost-sharing), associated with choice of video or telephone telemedicine (vs office visit).
Results Of 2 178 440 patient-scheduled primary care visits scheduled by 1 131 722 patients, 86% were scheduled as office visits and 14% as telemedicine visits, with 7% of the telemedicine visits by video. Choosing telemedicine was statistically significantly associated with patient sociodemographic characteristics. For example, patients aged 65 years and over were less likely than patients aged 18 to 44 years to choose telemedicine (RRR, 0.24; 95% CI, 0.22-0.26 for video visit; RRR 0.55; 95% CI, 0.54-0.57 for telephone visit). Choosing telemedicine was also statistically significantly associated with technology access (patients living in a neighborhood with high rates of residential internet access were more likely to choose a video visit than patients whose neighborhoods had low internet access: RRR, 1.10; 95% CI, 1.06-1.14); as well as in-person visit barriers (patients whose clinic had a paid parking structure were more likely to choose a telemedicine visit than patients whose facility had free parking: RRR, 1.70; 95% CI, 1.41-2.05 for video visit; and RRR, 1.73, 95% CI, 1.61-1.86 for telephone visit).
Conclusions and Relevance In this cross-sectional study, patients usually chose an in-person visit when scheduling an appointment online through the portal. Telemedicine may offer the potential to reach vulnerable patient groups and improve access for patients with transportation, parking, or cost barriers to clinic visits.
Telemedicine in various forms has the potential to engage patients through convenient health care access. 1 , 2 Video or telephone visits can offer patients real-time access to a clinician without the need to go to a clinic. Patients in the US spend an average of 2 hours, including travel and wait time, for a 20-minute in-person office visit. 2 , 3 Accordingly, while patient care-seeking for primary care has been associated with a wide range of financial and nonfinancial access barriers, patients who face greater barriers to in-person visits may choose a telemedicine visit if it offers greater convenience. 4 - 6
While more than 1 million US patients have used telemedicine, 7 direct-to-consumer services without in-person facilities often are not integrated with ongoing patient-clinician relationships or patient history within the electronic health record (EHR), which may create fragmentation from ongoing clinical care. 1 , 8 - 13 Expanding technology use is increasing the availability of video telemedicine to patients, but limited consensus for payers remains a barrier. 14 , 15 While video telemedicine has long been used in rural and specialty consultation, evidence remains particularly limited on video telemedicine use in primary care. 11 , 14 , 16 - 20 To our knowledge, no prior research evidence from large studies of patient choice between a traditional office visit and a telemedicine telephone or video visit within ongoing patient-clinician relationships in community primary care has been performed. 1 , 19 , 21 , 22
We examined an integrated delivery system setting in which patients using an online patient portal to schedule a primary care appointment were offered the choice to self-schedule a video telemedicine visit for primary care. Patients were offered a direct choice between 3 visit types with the same primary care clinician: office visit, video visit, or telephone visit. We examined rates of scheduled video or telephone telemedicine and patient characteristics associated with choosing telemedicine. We examined a broad set of patient characteristics including sociodemographic characteristics, technology access, and potential in-person visit barriers. We hypothesized that patient visit type preferences are associated with sociodemographic characteristics, and that greater technology access and barriers to in-person visits are associated with choosing telemedicine.
We examined primary care visits in Kaiser Permanente Northern California, a large integrated health care delivery system with more than 4 million members that uses a comprehensive outpatient-inpatient electronic health record (EHR; including outpatient, emergency, inpatient, laboratory, imaging, pharmacy history) and patient portal (website and mobile applications). The setting first implemented video visit technology in late 2014, with telephone visits used widely in clinical care since 2008. 23 Plan members are linked with a personal primary care clinician but may also visit other primary care clinicians.
Starting in 2016, patients scheduling a primary care appointment through the patient portal must choose their visit type: office, video, or telephone visit (except for visits designated as a routine physical examination, which were offered only as office visits). Available clinicians included patients’ own personal primary care clinician (primarily MDs, including nurse practitioners) or other primary care clinicians the patient had visited recently. The schedule availability and clinicians available were comparable across visit types, with appointment availability generally within 3 days (often the same day). Telemedicine was generally exempt from any patient out-of-pocket cost-sharing. Only the small subset of patients with a high-deductible health plan defined by the US Internal Revenue Service for health savings account eligibility faced cost-sharing for telemedicine visits.
All primary care clinicians had access to technology to conduct patient-physician telephone or video visits through the existing clinician-facing EHR including from any office phone or computer or from a work-issued mobile device. As in an office visit, clinicians had full access to the patient’s EHR history and documented telemedicine visits directly within the EHR. Patients could receive a call for a telephone visit at any phone number and could access video visits from home or elsewhere in their daily lives directly through any internet-connected and video-enabled computer or mobile device. Use of video visits in this setting and initial patient experiences have been described previously. 4
The Institutional Review Board of the Kaiser Foundation Research Institute approved the study protocol and materials and waived the requirement for written informed consent for participants in this data-only study. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guidelines for cross-sectional studies.
We identified all completed primary care appointments booked via the patient portal from January 1, 2016, to May 31, 2018. We included only index visits without any other clinical visits within 7 days prior to define a relatively distinct patient-initiated care-seeking episode. We also excluded visits for routine physical examination, which are not telemedicine-eligible.
Our study examined several types of patient characteristics including patient sociodemographic characteristics and other measures of accessibility and affordability grouped into technology access, in-person visit barriers, and patient-clinician affiliation. 5 For each patient included in the study, we used the EHR to identify patient sociodemographic characteristics (age, sex, race, language preference). Using the patients’ residential address, we defined their neighborhood socioeconomic status using 2010 US census measures at the census block group level, and neighborhood residential high-speed internet access level using FCC census tract level data. As additional measures of technology access, we captured patients’ prior mobile portal use as a measure of mobile device access, and video visit use in the past year to measure prior video visit experience. We extracted the patient’s insurance benefit cost-sharing for office visits, including copayment if a nondeductible plan, and deductible type if applicable (including health savings account–eligible high-deductible plans). We extracted the mean drive time from the patient’s residence to the nearest health system medical facility (61 total facilities), collected the type of parking offered at that facility and any parking fees (free parking lot or structure vs paid parking structure). We also used automated data sources to identify whether each visit was scheduled by a family care partner with permission to act for the patient through the patient portal, and whether the appointment was scheduled with the patient’s own personal primary care clinician.
We used multinomial logistic regression to examine the association (relative risk ratio [RRR]) between the chosen visit type (using office visit as the reference type) and patient characteristics, including patient sociodemographic characteristics (age, sex, race/ethnicity, neighborhood socioeconomic status, preferred language for health care), potential in-person visit barriers (out-of-pocket cost-sharing for office visits, drive time to clinic, facility parking garage and fee), technology access (neighborhood internet access level, portal access via mobile device in prior 365 days, video visits in prior 365 days), whether the appointment was booked by a care partner on behalf of the patient, and whether the clinician was the patient’s own personal primary care clinician. The multivariate model adjusted for patient medical problem ( International Statistical Classification of Diseases and Related Health Problems, Tenth Revision code grouping of primary diagnosis), whether patient had preexisting chronic conditions (in clinical registry of asthma, heart failure, diabetes, and hypertension in the quarter prior to index visit) and medical center. Statistical significance was determined by 2-sided P < .05. Standard errors were adjusted for the repeated visits within patients using Stata, version 14.2 (StataCorp LLC).
A total of 2 178 440 eligible patient-scheduled primary care visits were scheduled by 1 131 722 patients. Among all patient-scheduled visits through the portal, 86% were scheduled as in-person office visits and 14% as telephone or video telemedicine visits. Figure 1 shows quarterly video visit counts during the study period which began when online video visit scheduling was first offered (telephone visits in eFigure in the Supplement ). The Table shows demographic characteristics of patients scheduling a primary care visit included in the study.
Adjusted associations between patient sociodemographic characteristics and telemedicine visit choice are presented in Figure 2 . After adjustment, female patients and patients aged 18 to 44 years were more likely to choose a telemedicine visit (either phone or video) than male patients or patients of other ages. For example, patients aged 65 and over were less likely than patients aged 18 to 44 to choose telemedicine (RRR, 0.24; 95% CI, 0.22-0.26 for video visit; RRR, 0.55; 95% CI, 0.54-0.57 for telephone visit).
Black patients were significantly more likely than white patients to choose both types of telemedicine, with higher RRRs for video visits (RRR, 1.62; 95% CI, 1.52-1.73 for video visit; RRR, 1.28; 95% CI, 1.25-1.31 for telephone visit), while Hispanic patients were only less likely than White patients to choose video (RRR, 0.92; 95% CI, 0.88-0.97), and Asian patients were more likely than white patients to choose video (RRR, 1.26; 95% CI, 1.22-1.32), but less likely than white patients to choose telephone (RRR, 0.96; 95% CI, 0.94-0.97). After adjustment, black patients were more likely to choose both phone and video visits than any other race/ethnicity.
Patients living in a lower-socioeconomic status neighborhood were significantly less likely to choose a video visit (RRR, 0.93; 95% CI, 0.89-0.97). Patients with documented non–English-language preference were significantly less likely to choose either type of telemedicine than English speakers.
Adjusted associations between barriers to in-person visits and telemedicine visit choice are presented in Figure 3 . Patients whose insurance benefit plans required higher out-of-pocket cost-sharing for office visits (higher copayment if no deductible, or higher deductible if any deductible) were more likely to choose a telemedicine visit than patients with lower cost-sharing for office visits. For example, patients with an office visit copayment of $35 or more were significantly more likely to choose a video visit than patients with a $0-10 copayment (RRR, 1.49; 95% CI, 1.34-1.65) as were patients with a high-deductible plan (RRR, 1.85; 95% CI, 1.71-2.00).
Similarly, patients with longer relative driving time from home to the medical facility were significantly more likely to choose a telemedicine visit. Patients with a drive time longer than 30 minutes were significantly more likely than those with a less than or equal to 20-minute drive time to choose both video telemedicine (RRR, 1.32; 95% CI, 1.26-1.39) and telephone telemedicine (RRR, 1.14; 95% CI, 1.12-1.16). In addition, patients who may have needed to pay for parking in a garage structure were more likely to choose a telemedicine visit than patients whose facility had free parking (RRR, 1.70; 95% CI, 1.41-2.05 for video visit; RRR, 1.73; 95% CI, 1.61-1.86 for telephone visit).
Adjusted associations between patient technology access and personal clinician with telemedicine visit choice are presented in Figure 4 . Patients living in a neighborhood with higher rates of residential internet access were more likely to choose a video visit than patients whose neighborhoods had lower internet access (RRR, 1.10; 95% CI 1.06-1.14), as were patients with mobile device access defined by recent history of accessing the patient portal by mobile device (RRR, 1.35; 95% CI, 1.30-1.40). Prior experience with a video visit within the past year was associated with telemedicine choice (RRR, 11.39; 95% CI, 10.82-11.99 for video visit; RRR, 1.53; 95% CI, 1.48-1.58 for telephone visit). Patients whose visit was scheduled by a family care partner on their behalf were more likely to have a telemedicine visit rather than an office visit (RRR, 1.14; 95% CI, 1.05-1.25 for video visit; RRR, 1.53; 95% CI, 1.49-1.58 for telephone visit).
Patients were also more likely to schedule a telemedicine visit if they were visiting their own personal primary care clinician than visiting another primary care clinician (RRR 1.70, 95% CI, 1.62-1.79 for video visit; RRR 1.14, 95% CI, 1.13-1.16 for telephone visit).
In this study, we found that patients scheduled 86% of visits as office visits and 14% as telemedicine visits, with 7% of the telemedicine visits scheduled as video visits. While most patients scheduling a visit through the patient portal chose a traditional office visit, we found that telemedicine preference varied by patient age and race, was supported by greater technology access, and appeared to represent a convenient option to access some health care visits when facing logistical barriers to an office visit including transportation time and visit costs. Patients were more likely to choose telemedicine with their own personal primary care clinician.
Our findings suggest that some patient groups may be particularly well-reached by telemedicine, including some vulnerable groups. Further, there appears to be nuance in choice between phone and video visit types. For example, black patients were more likely than white patients to choose both video and telephone telemedicine, however, Asian patients were less likely than white patients to choose telephone but more likely than white patients to choose video visit. Patients living in lower socioeconomic status neighborhoods were more likely to choose a telephone visit but were less likely to choose a video visit than patients in higher socioeconomic status neighborhoods. Because mobile devices are used in most video visits, 23 and are increasingly the primary internet-access in vulnerable groups or those with lower health-engagement, mobile-friendly tools may represent valuable opportunities to engage these patients. 24 Even though mobile devices are widely adopted, our findings of differences in visit choice by technology access indicate that technology access is not uniform. 25
While early telemedicine efforts aimed to overcome travel barriers for specialty medical care access in remote locations, we found that patients were less likely to choose an office visit if the clinic was a farther drive or if parking was relatively more challenging. 26 Also, because telemedicine was more likely chosen by family care partners helping patients to schedule appointments, those with additional transportation or mobility challenges may gain greater health care access through telemedicine. Telemedicine may also efficiently connect a family member to a live visit over geographic distances that might make attending a clinic visit together impractical. 27 Further examination of specific patient groups whose needs may be particularly well met by telemedicine access is warranted.
Our findings suggest that patients with high out-of-pocket costs for office visits were more likely to choose a telemedicine visit. While most patients in our study had no out-of-pocket charge for telemedicine, in the small group with a high-deductible health plan that included an out-of-pocket charge for telemedicine, the cost-sharing differential still favored telemedicine. Notably, if visit cost-sharing was a factor in a patient delaying or avoiding any visit, these situations are not directly represented in our study sample.
Patients can face a wide range of financial and nonfinancial obstacles to receiving timely medical care, with barriers to primary care associated with more emergency department visits. 28 We examined an integration of patient-initiated telemedicine visits with ongoing clinical care and patient-clinician relationships. While the landscape of telemedicine payment barriers is evolving, this study offers an opportunity to examine when patient-scheduled telemedicine is fully integrated into clinical care delivery and into the EHR. We offer specific findings about patient choice of telemedicine in the absence of differences in clinician and availability that may have consequences for direct-to-consumer telehealth. Our finding that patients were more likely to choose telemedicine with their own personal primary care clinician suggests that telemedicine might be especially preferred within ongoing patient-physician relationships. This telemedicine continuity may also hold clinical value as primary care continuity improves health care efficiency and health outcomes. 29
This study has several limitations. Findings from this specific setting and limited to patient-initiated appointments scheduled online may not be generalizable to other less-integrated telemedicine delivery settings or different patient-initiated appointment-scheduling workflows. In deriving patient characteristics such as internet access, parking status, and socioeconomic status, we use general area characteristics and cannot directly associate any given barrier to an individual’s own experience. Another unmeasured common barrier, noted in our prior patient surveys, is a need to take time off from work to attend an in-person doctor’s office visit. 4 In this study we do not have available automated data measures about patient work schedule and other personal responsibilities or visit barriers, but future research may examine this issue directly. While our analysis statistically adjusts for the general clinical area of a visit, it is still possible that patients are making visit-typed decisions based on perceptions of clinical need such as acuity, severity, or comorbidities that are not accounted for in our analysis. Future research may assess telemedicine follow-up visits within a given episode of care. Overall, our extensive set of patient and system variables allows for rigorous statistical adjustment, but an observational study cannot determine causation.
Our study period is limited to the initial implementation period after patient online-scheduled video telemedicine was first offered in the study setting. While telemedicine visits were primarily by telephone, video visit rates were increasing. We hypothesize that the telephone visit format was more familiar to patients in the study setting because telephone visits had been widely used in primary care for several years prior to the introduction of video visits. In the emerging area of telemedicine delivery of primary care, patient visit choice patterns will likely change over time and the study setting will also adapt its offerings. For example, more recently the study’s health system plans to integrate language interpretation services within telemedicine to improve access for non–English-speaking patients. Indeed, we found rates of choosing video were more than 10 times higher in patients who had prior scheduled video visit experience than in patients without prior experience. As patients and clinicians continue to gain experience with video telemedicine and the unique ways that it might fit particular personal and clinical situations, ongoing research on patient telemedicine preference and choice is needed. Also needed is further research examining quality and clinical outcomes associated with telemedicine visits and implementation factors that may affect adoption rates by both patients and clinicians. 26
While telemedicine can offer patients a convenient way to seek care from familiar clinicians, in this study of patient-scheduled primary care visits through a patient portal, we found that patients still primarily chose to schedule a traditional in-person office visit. Choosing a telemedicine visit was associated with patient sociodemographic characteristics, technology access and experience, in-person visit barriers, and continuity with the patient’s personal clinician, indicating a nuanced context within which patients may choose telemedicine rather than an office visit. While patient access to telemedicine visits may represent a transformative shift in patient-centered convenient health care access, the associations identified in this study of patient choice may indicate opportunities to engage non-white patients, patients with lower socioeconomic status, patients with mobile technology access, and those who face barriers to in-person visits.
Accepted for Publication: March 20, 2020.
Published: June 17, 2020. doi:10.1001/jamanetworkopen.2020.5873
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2020 Reed ME et al. JAMA Network Open .
Corresponding Author: Mary E. Reed, DrPH, Kaiser Permanente Division of Research, 2000 Broadway, Oakland CA, 94612 ( [email protected] ).
Author Contributions : Drs Reed and Huang had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Reed, Huang, Graetz, Muelly, Kim.
Acquisition, analysis, or interpretation of data: Reed, Huang, Lee, Muelly, Kennedy.
Drafting of the manuscript: Reed.
Critical revision of the manuscript for important intellectual content: Huang, Graetz, Lee, Muelly, Kennedy, Kim.
Statistical analysis: Reed, Huang, Muelly, Kennedy.
Obtained funding: Reed.
Supervision: Reed, Lee, Muelly.
Conflict of Interest Disclosures: Drs Reed and Huang reported receiving grants from the Agency for Healthcare Research and Quality during the conduct of the study. No other disclosures were reported.
Funding/Support: This study was funded by the Agency for Healthcare Research and Quality (grant R01HS25189).
Role of the Funder/Sponsor: The funding source had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- View Locations
- Call Us (951) 779-1670
- [email protected]
- Mon - Fri: 9:00am - 5:00pm

- Appointments
The Nine Types of Patient Visits
1) physical exams & sports physicals, 2) non-physical or sick visits, 3) consultation & results review visits, 4) “nurse only” (medical assistant) (such as weight checks, shots and tb tests), 5) medical consent and instructional or teaching visits, 6) pre-op & surgery visits (including dental clearance for anesthesia), 7) psychiatric related visits (including questions about behavioral disorders, eating disorders and add), 8) follow-up visits, 9) telemedicine visits.
Each visit is given a different time allotment at the time you call to schedule your appointment, and this time slot cannot be changed after you arrive in the office. It is very rare that we are able to combine visit types and thus it should not be expected. So if your concerns overlap appointment types, you will most likely need more than one appointment.
Appointments
Select a Section
- New Patients
- Visit Descriptions
- Telemedicine
Establish Care (New Patient): This type of appointment is for your first visit with your new health care provider after switching your health care to our practice. It is designed to include a thorough review of your past medical history. It may include blood work or other testing, if indicated.
Consultation (New Patient): This type of appointment is for your first visit with one of our providers to discuss a specific issue, such as nutrition, if you may not want to transfer your care entirely.
Once you have created your portal account and have been scheduled for your first telehealth appointment, please feel free to upload any medical records directly into your portal prior to your visit.
Annual Physical Examination: This examination is typically done yearly and is a time to provide routine preventive care. During your visit, your doctor may review your overall health (including lifestyle risk factors, such as exercise and diet) and order any age-specific screening tests (such cancer screening or depression screening) and immunizations you may need. The goal is to identify risk factors or early signs and symptoms of chronic diseases, and counsel you on how you can reduce your risk and improve your overall health. Blood work may or may not be part of this visit, based on your individual state of health and your risk factors. Please note that annual physical examinations are in-office visits and cannot be done virtually.
To optimally address all your health concerns, other complaints or issues are best addressed during a problem visit. Examples include the management of diabetes or other chronic diseases or the evaluation of a new complaint such as fatigue or joint pain. If these issues are addressed during your appointment for an annual physical, your health care provider may bill for these services in addition to your annual physical.
Learn more about Annual Visits vs. Office Visits .
Medicare does not cover annual physical examinations but does cover Medicare annual wellness visits (see description below). In addition, some insurance plans do not cover annual physical exams; please be aware of what your individual plan does and does not cover.
Follow-Up Office Visits: This type of appointment is for the routine monitoring of any specific chronic medical conditions or problems you may have, for example, a follow-up visit to monitor the status of your blood pressure if you have chronic high blood pressure or your blood sugar control if you have diabetes. This appointment is currently being offered via telehealth only.
Non-Urgent Problem Visit: This type of appointment is for any new health problem that is not urgent; for example, if you developed chronic knee pain or rash that has persisted over several weeks. This appointment is currently being offered via telehealth only.
Urgent/Same-Day Appointment: This type of appointment is for a new symptom or a recent change in your health that you feel needs to be evaluated as soon as possible, for example, if you started to have burning and pain while urinating or an acute sore throat. This appointment is currently being offered via telehealth only unless otherwise specified by a clinician.
Medicare Annual Wellness Visit (AWV): This appointment is currently being offered via telehealth only. The purpose of this visit is to develop or update a personalized prevention help plan to prevent disease and disability based on your current health and risk factors. Your provider will ask you to fill out a health risk assessment questionnaire. It is helpful to have this filled out prior to the visit. Answering these questions can help you and your provider develop a personalized prevention plan to help you stay healthy and get the most out of your visit. It also includes:
- A review of your medical and family history
- A list of current providers and prescriptions
- Height, weight, blood pressure, and other routine measurements
- Detection of any cognitive impairment
- Personalized health advice
- A list of risk factors and treatment options for you
- A screening schedule (like a checklist) for appropriate preventive services
Medicare also covers a variety of other preventive screenings and services as outlined here: https://www.medicare.gov/coverage/preventive-and-screening-services.html
Please note that AWV does not cover an examination or any routine lab work (other than a lipid panel every five years). Your health care provider may still recommend certain screening lab tests, but Medicare may not cover these services.
Please note that if you have other chronic medical conditions that are addressed during your AWV, your health care provider may bill for these services in addition to your AWV.
Medical Nutrition Therapy (MNT): This visit includes evaluation by a registered dietitian, who is trained to use dietary interventions to prevent or treat many chronic health conditions. Our dietitians will work with you to develop personalized dietary advice to help you reach your health goals. Medicare and certain other insurance plans may only pay for this service if you have very specific medical conditions. However, we do offer discounts in the event you have to pay out of pocket for MNT.
For new patients that wish to meet with a dietitian, we need a referral from your current primary care or specialist provider indicating the reason why you need to meet with a nutritionist along with most recent labs. Once we receive those necessary documents, we will reach out to make an appointment for you.
For current patients , you would need to meet with one of clinicians first so they can write a referral for you and order any necessary labs. A member of our staff will reach out to you to make that appointment for you.
Shared Medical Appointments: These combine group and one-on-one care—with extra time for education, group support, and lots of Q&A—at the same cost as a regular individual visit. The sessions will focus on diabetes reversal or heart health and include other patients and health care professionals, while leaving plenty of time for individual care. And, of course, we will go over your medications, order tests, discuss test results, talk about side effects and treatment options, and provide brief exams, if necessary. Some sessions will also include in-person educational sessions with Neal Barnard, MD, FACC, our clinic founder.
The purpose of these appointments is to give us extra time to discuss questions you have regarding your health, and to take advantage of something we have discovered in our research studies: Patients gain key insights and support from each other. The educational component of the visits allows you to gain deeper knowledge of the causes, treatment, and hopefully reversal of many chronic diseases.
Make an Appointment
To schedule your next appointment, please call us at 202-527-7500. Monday: 8:30 a.m. - 4 p.m. Tuesday: 8:30 a.m. - 4 p.m. Wednesday: 8:30 a.m. - 12 p.m. Thursday: 8:30 a.m. - 4 p.m. Friday: 8:30 a.m. - 4 p.m.
Patient Login
Support Our Lifesaving Work
5100 Wisconsin Ave., NW, Suite 401 Washington, DC 20016
Phone: 202-527-7500 Fax: 202-527-7400
Contact Us Find Us on Facebook
This site does not provide medical or legal advice. This website is for information purposes only. Due to privacy concerns and the insecure nature of e-mail, please do not send medical, insurance, or financial information via e-mail. Full Disclaimer
For informational purposes only, a link to the federal Centers for Medicare and Medicaid Services (CMS) Open Payments web page is provided here. https://openpaymentsdata.cms.gov/ The federal Physician Payments Sunshine Act requires that detailed information about payment and other payments of value worth over ten dollars ($10) from manufacturers of drugs, medical devices, and biologics to physicians and teaching hospitals be made available to the public.

- Center on Health Equity and Access
- Health Care Cost
- Health Care Delivery
- Value-Based Care
Provider Type and Management of Common Visits in Primary Care
- Lee F. Cromwell, MS
- Michael Robbins, PhD
- Brandi E. Robinson, MPH
- David Auerbach, PhD
- Ateev Mehrotra, MD, MPH
In primary care, nurse practitioners and physician assistants do not necessarily order more ancillary services, or more costly services among alternatives, than physicians.
Objectives: Debate continues on whether nurse practitioners (NPs) and physician assistants (PAs) are more likely to order ancillary services, or order more costly services among alternatives, than primary care physicians (PCPs). We compared prescription medication and diagnostic service orders associated with NP/PA versus PCP visits for management of neck or back (N/B) pain or acute respiratory infection (ARI).
Study Design: Retrospective, observational study of visits from January 2006 through March 2008 in the adult primary care practice of Kaiser Permanente in Atlanta, Georgia.
Methods: Data were obtained from electronic health records. NP/PA and PCP visits for N/B pain or ARI were propensity score matched on patient age, gender, and comorbidities.
Results: On propensity score-matched N/B pain visits (n = 6724), NP/PAs were less likely than PCPs to order a computed tomography (CT)/magnetic resonance image (MRI) scan (2.1% vs 3.3%, respectively) or narcotic analgesic (26.9% vs 28.5%) and more likely to order a nonnarcotic analgesic (13.5% vs 8.5%) or muscle relaxant (45.8% vs 42.5%) (all P ≤.05). On propensity score-matched ARI visits (n = 24,190), NP/PAs were more likely than PCPs to order any antibiotic medication (73.7% vs 65.8%), but less likely to order an x-ray (6.3% vs 8.6%), broad-spectrum antibiotic (41.5% vs 42.5%), or rapid strep test (6.3% vs 9.7%) (all P ≤.05).
Conclusions: In the multidisciplinary primary care practice of this health maintenance organization, NP/PAs attending visits for N/B pain or ARI were less likely than PCPs to order advanced diagnostic radiology imaging services, to prescribe narcotic analgesics, and/or to prescribe broad-spectrum antibiotics.
Am J Manag Care. 2017;23(4):225-231 Takeaway Points
Practice variation by providers, rather than by provider type, may be more important in understanding differences in management of conditions commonly presented in primary care.
Nevertheless, concerns have been expressed that nurse practitioners (NPs) and physician assistants (PAs) might more frequently order ancillary services, or more costly services among alternatives, compared with primary care physicians. In this study of a group model health maintenance organization’s primary care practice, we found NPs and PAs were less likely to order:
- Advanced diagnostic imaging or narcotic analgesics for management of neck or back pain.
- Broad-spectrum antibiotics or rapid strep tests for management of acute respiratory infections.
Increasing the percentage of nurse practitioners (NPs) and physician assistants (PAs) in the primary care provider workforce has been suggested as one strategy for addressing the United States’ national shortage of primary care physicians (PCPs). 1-5 Although NPs/PAs have clinical training and regulated scopes of practice that differ from those of PCPs, they are permitted to manage a range of medical conditions in ambulatory care. 6-11 A recent survey of the US national population indicated broad acceptance of NPs/PAs as primary care providers. 12
Currently, there is interest in how the addition of NPs/PAs to primary care might impact patient outcomes, medical service utilization, and costs. 13-17 Prior studies have been relatively consistent in demonstrating that levels of patient satisfaction with care and quality of care are similar between NPs/PAs and physicians 11,18-23 ; however, it is less clear whether care provided by NPs/PAs or PCPs affects medical services use and cost.
An NP/PA visit can be cost saving compared with a PCP visit because salary differentials lower the cost of time for patient evaluation and management. 13,17,24,25 However, this cost advantage may be offset if NPs/PAs order ancillary services (ie, laboratory, radiology, pharmacy) at higher rates than PCPs, or order more costly services among alternatives (eg, computed tomography [CT] scan/magnetic resonance image [MRI] vs x-ray).
Studies show mixed results on use of ancillary services by provider type. One study found NPs/PAs ordered significantly more CTs/MRIs for primary care visits than physicians treating Medicare patients 26 ; another found no difference in office-based care using the National Ambulatory Medical Care Survey (NAMCS). 16 A study of Veterans Affairs patients with lower back pain found no statistically significant difference in clinical appropriateness of lumbar spine MRIs by provider type (physician, PA, or NP). 27 In prescribing medications, rates of prescribing controlled medications 28 and antibiotics 16,29 were similar for NPs, PAs, and physicians.
The primary question of our retrospective observational study was: Do NPs/PAs attending visits for neck or back (N/B) pain or acute respiratory infection (ARI) in primary care order ancillary services at different rates than PCPs? We focused on these 2 medical conditions for several reasons. Musculoskeletal pain and respiratory infections are common reasons that adults present for medical care in the United States, 30 and visits for N/B pain or ARI are frequently accompanied by orders for ancillary services. There are general concerns that, across all providers, certain types of ancillary services are overused and add cost without value—specifically, CTs/MRIs and narcotic analgesics in management of N/B pain, 16,31,32 and antibiotics (particularly broad-spectrum antibiotics) in management of ARI. 33-38
METHODS Study Setting and Period
At the time of this study, Kaiser Permanente Georgia (KPGA) provided comprehensive medical services to approximately 240,000 enrollees per year (59% Caucasian, 33% African American) in the Atlanta area. The study protocol was reviewed, approved, and monitored by the KPGA Institutional Review Board.
During the 27-month study period (January 2006 through March 2008), approximately 180,000 KPGA members were empaneled to a PCP in the Adult Medicine department. The study period is limited to these 27 months because, beginning in 2006, an electronic health record (EHR) system was fully implemented—allowing for measurement of providers’ orders for medical services—and it ends in early 2008 when the multidisciplinary Adult Medicine department became a PCP-only department. 39 More recent comparisons of practice variation are not available.
Sample Definition
The sample used for analysis consisted of patients 18 years or older at the time of presentation for an “incident” N/B pain or ARI visit in the KPGA Adult Medicine department. An “incident” visit was considered to have occurred if the patient who presented for N/B pain or ARI had no visit in adult ambulatory medicine for N/B pain or ARI, respectively, for at least a period of 30 days prior to the visit. Using this definition, a single patient may have had multiple incident visits during the study period.
A visit for N/B pain or ARI was determined from specific International Classification of Diseases, Ninth Revision, Clinical Modification ( ICD-9-CM ) diagnosis codes associated with the visit, either designated as a primary or secondary condition ( eAppendix A [eAppendices available at ajmc.com ]). Due to the broad range of ARIs, we selected specific ICD-9-CM diagnosis codes used in previously published studies as indicative of an ARI. 33-38
Research Design
We used propensity score matching of visits to reduce the effect of patient selection on comparisons of practice variation between NPs/PAs and PCPs when attending a visit for N/B pain or ARI. NPs/PAs tend to treat younger, healthier patients than physicians which, in turn, can affect rates and mix of ancillary service orders. 11,16,40 Thus, we propensity score-matched NP/PA visits with PCP visits on preexisting patient characteristics to address potential selection issues.
Separate analyses were conducted for N/B pain and ARI visits. First, within each visit class, the propensity for a visit to be attended by a NP/PA
versus PCP was estimated with logistic regression. 41-43 Second, based on the estimated propensity of NP/PA versus PCP attending a visit, each N/B pain or ARI visit attended by an NP/PA was matched with an N/B pain or ARI visit, respectively, attended by a PCP.
All analyses used computerized administrative and EHR databases. Records were linked by unique identifiers and sequenced by event dates. The EHR databases distinguished services ordered by the provider from services completed by the patient. We used services ordered rather than services delivered because rates of services delivered can be affected by factors such as patient access (eg, limited locations for CT/MRI services) or cost sharing (eg, co-payments for prescription medicines). 44 Thus, services ordered are more representative of practice style than services delivered.
Services ordered at the time of the visit were linked to the incident N/B pain or ARI visit by unique visit numbers. All services ordered were attributed to the provider attending the visit. Thus, there is no attribution of orders by an NP/PA to a PCP providing practice supervision (as might occur in billing of “incidental to” visits).
We were advised by several senior physicians that some orders related to the incident visit might occur up to 3 to 5 days following conveyance to the attending provider of initial tests or consultation results. Thus, we considered a diagnostic service order or prescription order as related to the incident visit if it occurred within 5 days from the visit date and was ordered by a provider in the adult primary care department at the same primary care facility where the incident visit occurred. Follow-up orders occurred in less than 5% of NP/PA visits and/or PCP visits for either N/B pain or ARI (data available on request).
Dependent variables. The outcomes of interest were the percentages of visits associated with an order for a specific service class. The service order classes defined for N/B pain visits were: N/B x-rays, N/B CTs/MRIs, nonnarcotic analgesic prescriptions, narcotic analgesic prescriptions, and prescriptions for skeletal muscle relaxants. The service order classes defined for ARI visits were: ARI x-rays, ARI CTs/MRIs, rapid strep tests, any systemic antibiotic prescription, any broad-spectrum antibiotic prescription, and any prescription for relief of ARI symptoms (eg, decongestants, expectorants, respiratory system anti-inflammatory medications). We combined CTs with MRIs because preliminary review of the data indicated very low rates of MRIs relative to CTs, and availability of one or the other of these advanced diagnostic imaging services at selected facilities preferred by a patient might have affected a provider’s decision to schedule one or the other of these services.
Independent variable. The primary independent variable was the type of provider who attended the visit: NP/PA versus PCP.
Patient covariates. Covariates were: age at the time of the visit, gender, years of enrollment with KPGA at the time of the visit, and the presence (vs absence) of several major comorbidities (diabetes, hypertension, hyperlipidemia, cardiovascular disease [coronary artery disease, congestive heart failure, cerebrovascular disease], asthma or chronic obstructive pulmonary disease, or cancer) at the time of the visit.
Statistical Analysis
The initial step in analysis was to compare the distribution of patient characteristics at presentation for a visit for N/B pain or ARI with respect to attending provider type: NP/PA versus PCP. Independence of patient characteristics from attending provider type (ie, NP/PA vs PCP) was assessed using a 2 test.
Propensity of a visit for N/B pain or ARI to have been attended by an NP/PA versus PCP was estimated using logistic regression including the patient covariates. This step resulted in a probability estimate of NP/PA versus PCP selection. Matching of 1 NP/PA visit with 1 PCP visit was done using a caliper of 0.25 times the standard deviation (SD); matching was done without replacement. Distributions of patient covariates before and after propensity score matching were compared using a 2 test. Before and after propensity score matching, the percentages of visits with a related diagnostic test or a medication order on an NP/PA versus PCP visit were compared using a 2 test.
Several sensitivity analyses were conducted. Results might be sensitive to the granularity of matching of NP/PA to PCP visits. Sensitivity of propensity score matching was tested with a finer caliper of 0.025 times the SD. Second, we examined percentages of visits with diagnostic radiology or medication orders by subgroups of visits classified according to the primacy of codes for presenting conditions, assuming that NPs/PAs or PCPs might use the EHR differently and, therefore, code visits differently according to sequence of “presenting” and “diagnosed” conditions. Finally, we estimated a logistic regression of each service order type as a function of NP/PA versus PCP using PROC GENMOD (SAS Institute, Cary, North Carolina) to evaluate whether clustering of service orders by provider might account for statistical significance of likelihood of a service type order by NP/PA or PCP.
All data management and statistical analyses were conducted using SAS version 9.4 (SAS Institute, Cary, North Carolina).
NPs/PAs attended to 16.2% of the visits (6724 of 41,404) with N/B pain as a primary or secondary diagnosis. NPs/PAs attended to 22% of the visits (24,190 of 109,844) with ARI as a primary or secondary diagnosis.
Table 1 displays patient characteristics on visits for N/B pain or ARI. Compared with PCPs, patients on N/B pain or ARI visits attended by NPs/PAs were younger, of shorter enrollment duration, and had lower prevalence of major comorbidities.
Table 2 displays the percent of N/B pain visits with orders for diagnostic radiology services and prescription medications by provider type, both before and after propensity score matching. After propensity score matching, PCPs were more likely to order an N/B-related CT/MRI (3.3% vs 2.1%; P <.01) or a narcotic analgesic (30.1% vs 26.9%; P <.01). On the other hand, NPs/PAs were more likely to order a nonnarcotic analgesic (13.5% vs 8.5%; P <.01) or a musculoskeletal relaxant (45.8% vs 42.5%; P <.01). N/B pain visits with an order for an x-ray did not differ between NPs/PAs or PCPs (21.6% vs 22.1%; P = .53).
Table 3 displays the percent of ARI visits with orders for diagnostic radiology services and prescription medications by provider type, both before and after propensity score matching. After propensity score matching, there were significant differences in practice between NPs/PAs and PCPs in treatment of ARI. Over all visits, PCPs were more likely to order ARI-related x-rays (8.6% vs 6.3%; P <.01), CTs/MRIs (0.5% vs 0.3%; P <.01), a broad-spectrum antibiotic (42.5% vs 41.5%; P = .03), or a rapid strep test (9.7% vs 6.3%; P <.01). NPs/PAs, however, were more likely to order any antibiotic (73.7% vs 65.8%; P <.01). As with N/B pain visits, this difference in practice variation between NPs/PAs and PCPs was the same as that observed before propensity score matching.
In the first sensitivity analysis, matching on a smaller caliper made no difference in the findings. Next, the practice pattern differences between NPs/PAs and PCPs over all visits on which a diagnosis of N/B pain (or ARI) was suggested were basically the same whether the relevant ICD-9-CM code was primary or secondary (Tables 2 and 3). Finally, there was some clustering by provider, and adjusting for this clustering tended to push the statistical significance of the NP/PA versus PCP effect toward the null ( eAppendix B ) in some cases; for example, CT/MRI for back pain pushing significance to nonsignificance (ie, P >.05). For most comparisons by provider type, however, the NP/PA versus PCP effect was significant whether the model did or did not account for clustering of service orders by provider.
The objective of our study was to ascertain whether NPs/PAs differed from PCPs in frequency of orders for diagnostic services or prescription medications when managing adults presenting with N/B pain or ARI in primary care. We used propensity score matching of visits to adjust for the fact that patients attended by NPs/PAs tended to be younger and have a lower prevalence of comorbidities, which could affect diagnostic or therapeutic treatment choice.
After matching, several important differences by type of primary care provider were noted in management of N/B pain: PCPs were more likely to order CTs/MRIs and narcotic analgesics and NPs/PAs were more likely to order nonnarcotic analgesics and muscle relaxants. Similarly, differences were noted in management of ARI: PCPs were more likely to order CTs/MRIs—although the rate of these orders was low—as well as x-rays, broad spectrum antibiotics, and rapid strep tests; NPs/PAs were more likely to order any antibiotic. Thus, on balance, PCPs tended to be more likely than NPs/PAs to order diagnostic or therapeutic services related to N/B pain and ARI visits and to order more costly services among alternatives (eg, CTs/MRIs vs x-rays for adults with N/B pain, broad spectrum antibiotics vs first-line general antibiotics for adults with ARIs).
Evidence from this health maintenance organization (HMO), therefore, differs from the results of other studies, suggesting that NPs/PAs might more frequently order diagnostic or therapeutic services for common conditions treated in primary care; or, among alternatives, order more costly services. 27 Our study’s findings are, however, consistent with another recent study using data from the National Ambulatory Medical Care Survey (NAMCS), which found no significant differences between NPs/PAs and physicians in office-based practice when ordering “low-value” ancillary services. 16 In our study, the pattern of ancillary services use suggests that NPs/PAs might have been more judicious in use of “low-value” ancillary services than PCPs. For management of back pain, overuse of CTs/MRIs and narcotic analgesics is a current concern. 32 We found NPs/PAs had lower rates of use of CTs/MRIs and narcotic analgesics in management of N/B pain. In management of an ARI, overuse of antibiotics—particularly broad-spectrum antibiotics—is a long-standing concern. 33-36,38 Overuse of rapid strep tests is another concern in management of ARIs, 37 and we found NPs/PAs were less likely to order broad-spectrum antibiotics and rapid strep tests.
What factors might have contributed to this NPs/PA practice pattern? Training of NPs/PAs typically emphasizes patient education and self-management over other interventional strategies. Thus, NPs/PAs may be more comfortable in initially managing N/B pain or ARI with fewer ancillary services. It is also possible that NPs/PAs are more compliant than PCPs with clinical practice guidelines in management of N/B pain or ARI in primary care.
Sensitivity analyses suggest this study’s findings are robust. Matching a narrower caliper —one a tenth of that used for the findings discussed in this paper—yielded similar results. Frequencies of orders by NPs/PAs versus PCPs for visits related to N/B pain (or ARI) did not generally differ by whether N/B pain (or ARI) was indicated as a primary or secondary diagnosis. The clustering analyses do indicate some proportion in outcomes by provider type is due to practice variation among individual providers; however, the persistence of significance of the NP/PA effect after adjusting for provider clustering strongly suggests that practice variation by provider type is important.
Limitations
Our study was conducted within the context of a single, group-model HMO in the southeastern United States. Because this HMO had a strong tradition encouraging multidisciplinary, collaborative primary care, study findings might not be generalizable to other settings with a different delivery model. NPs/PAs work under supervision of PCPs; however, we had no measure of how supervision practices might have influenced NP/PA ordering patterns. During the study period, NPs/PAs were relatively established in this HMO; their practice patterns might not represent practice patterns of newly hired NPs/PAs. This HMO had relatively well-defined practice guidelines for management of N/B pain and ARI. Rates of orders for medications reflect only orders for prescriptions and not over-the-counter medications. We did not investigate specific quality measures, so we cannot conclude that over- or underuse of specific diagnostic services or prescribed medications was beneficial or detrimental to patient health. The propensity score matching relied on a limited number of patient covariates, and does not necessarily account for illness acuity within the selected comorbidities. Other factors that varied across clinics where NPs/PAs practiced (eg, use of care managers in some clinics but not others) might also influence practice variation by provider type.
Other factors that we did not consider in our analyses could offset the potential savings in medical care delivery costs due to lower ancillary services rates on visits attended by NPs/PAs. Length of visit was not available, so we could not assess if longer NP/PA visits decreased visit productivity (in terms of visits per day) and attenuated labor cost savings due to lower NP/PA salaries. 13,45 We did not examine variation by provider type in other utilization measures such as referrals or potentially avoidable hospital admissions. Other studies that have examined postvisit utilization generally find equal or lower rates of these classes of services following NP/PA visits compared with physician visits. 15,22 Similarly, we show elsewhere that the extent of NP/PA integration into this HMO’s primary care delivery system did not increase levels of these broad classes of utilization across all medical conditions. 39
CONCLUSIONS
In this group model HMO, NPs/PAs who attended visits related to N/B pain or ARI in adult primary care typically had lower rates of associated orders for diagnostic services or prescription medications than PCPs when treating patients of comparable age, gender, and comorbidities.  Author Affiliations: School of Public Health, Georgia State University (DWR), Atlanta, GA; Center for Clinical and Outcomes Research, Kaiser Permanente (DWR, LFC, BER), Atlanta, GA; RAND Corporation (HL, MR, AM), Santa Monica, CA; Harvard University (HL, AM), Cambridge, MA; Massachusetts Health Policy Commission (DA), Boston, MA.
Source of Funding: Funds to conduct this study were provided by a grant from the American Academy of Family Physicians. The funding source had no role in the study design, data collection, interpretation of the results, and decision to submit the manuscript. Analyses and interpretations presented in this manuscript are solely those of the authors and do not represent the views of the sponsor or the authors’ employers.
Author Disclosures: The authors report no relationship or financial interest with any entity that would pose a conflict of interest with the subject matter of this article.
Authorship Information: Concept and design (DWR, HL, MR, DA, AM); acquisition of data (DWR, LFC, DA); analysis and interpretation of data (DWR, HL, LFC, MR); drafting of the manuscript (DWR, MR); critical revision of the manuscript for important intellectual content (DWR, HL, MR, BER, AM); statistical analysis (DWR, LFC, MR); provision of patients or study materials (BER); obtaining funding (DWR, DA); administrative, technical, or logistic support (BER, AM); and supervision (DWR).
Address Correspondence to: Douglas W. Roblin, PhD, School of Public Health, Georgia State University, 1 Park Pl, Rm 662C, Atlanta, GA 30303. E-mail: [email protected].
1. Auerbach DI, Chen PG, Friedberg MW, et al. Nurse-managed health centers and patient-centered medical homes could mitigate expected primary care physician shortage. Health Aff (Millwood) . 2013;32(11):1933-1941. doi: 10.1377/hlthaff.2013.0596.
2. Bodenheimer TS, Smith MD. Primary care: proposed solutions to the physician shortage without training more physicians. Health Aff (Millwood) . 2013;32(11):1881-1886. doi: 10.1377/hlthaff.2013.0234.
3. Kirch DG, Henderson MK, Dill MJ. Physician workforce projections in an era of health care reform. Annu Rev Med . 2012;63:435-445. doi: 10.1146/annurev-med-050310-134634.
4. Kuo YF, Loresto FL Jr, Rounds LR, Goodwin JS. States with the least restrictive regulations experienced the largest increase in patients seen by nurse practitioners. Health Aff (Millwood) . 2013:32(7):1236-1243. doi: 10.1377/hlthaff.2013.0072.
5. Sargen M, Hooker RS, Cooper RA. Gaps in the supply of physicians, advance practice nurses, and physician assistants. J Am Coll Surg . 2011;212(6):991-999. doi: 10.1016/j.jamcollsurg.2011.03.005.
6. Christian S, Dower C, O’Neil E. Overview of nurse practitioner scopes of practice in the United States—discussion. The Center for the Health Professions, University of California, San Francisco website. https://healthforce.ucsf.edu/publications/overview-nurse-practitioner-scopes-practice-united-states. Published December 1, 2007. Accessed June 23, 2016.
7. Dunker A, Krofah E, Isasi F. The role of physician assistants in health care delivery. National Governors Association website. https://www.nga.org/files/live/sites/NGA/files/pdf/2014/1409TheRoleOfPhysicianAssistants.pdf. Published September 22, 2014. Accessed June 23, 2016.
8. Gadbois EA, Miller EA, Tyler D, Intrator O. Trends in state regulation of nurse practitioners and physician assistants, 2001 to 2010. Med Care Res Rev . 2015;72(2):200-219. doi: 10.1177/1077558714563763.
9. Schiff M. The role of nurse practitioners in meeting increasing demand for primary care. National Governors Association website. https://www.nga.org/cms/home/nga-center-for-best-practices/center-publications/page-health-publications/col2-content/main-content-list/the-role-of-nurse-practitioners.html. Published December 20, 2012. Accessed June 23, 2016.
10. Morgan PA, Abbott DH, McNeil RB, Fisher DA. Characteristics of primary care office visits to nurse practitioners, physician assistants and physicians in United States Veterans Health Administration facilities, 2005 to 2010: a retrospective cross-sectional analysis. Hum Resour Health . 2012;10:42. doi: 10.1186/1478-4491-10-42.
11. Roblin DW, Becker ER, Adams EK, Howard DH, Roberts MH. Patient satisfaction with primary care: does type of practitioner matter? Med Care . 2004;42(6):579-590.
12. Dill MJ, Pankow S, Erikson C, Shipman S. Survey shows consumers open to a greater role for physician assistants and nurse practitioners. Health Aff (Millwood) . 2013;32(6):1135-1142. doi:
10.1377/hlthaff.2012.1150.
13. Basu S, Landon BE, Song Z, Bitton A, Phillips RS. Implications of workforce and financing changes for primary care practice utilization, revenue, and cost: a generalizable mathematical model
for practice management. Med Care . 2015;53(2):125-132. doi: 10.1097/MLR.0000000000000278.
14. Hughes DR, Jiang M, Duszak R Jr. A comparison of diagnostic imaging ordering patterns between advanced practice clinicians and primary care physicians following office-based evaluation and management visits. JAMA Intern Med . 2015;171(1):101-107. doi: 10.1001/jamainternmed.2014.6349.
15. Kuo YF, Chen NW, Baillargeon J, Raji MA, Goodwin JS. Potentially preventable hospitalizations in Medicare patients with diabetes: a comparison of primary care provided by nurse practitioners versus physicians. Med Care . 2015;53(9):776-783. doi: 10.1097/MLR.0000000000000406.
16. Mafi JN, Wee CC, Davis RB, Landon BE. Comparing use of low-value health care services among U.S. advanced practice clinicians and physicians. Ann Intern Med . 2016;165(4):237-244. doi: 10.7326/M15-2152.
17. Perloff J, DesRoches CM, Buerhaus P. Comparing the cost of care provided to Medicare beneficiaries assigned to primary care nurse practitioners and physicians. Health Serv Res . 2016;51(4):1407-1423. doi: 10.1111/1475-6773.12425.
18. Everett C, Thorpe C, Palta M, Carayon P, Bartels C, Smith MA. Physician assistants and nurse practitioners perform effective roles on teams caring for Medicare patients with diabetes. Health Aff (Millwood) . 2013;32(11):1942-1948. doi: 10.1377/hlthaff.2013.0506.
19. Horrocks S, Anderson E, Salisbury C. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ . 2002;324(7341):819-823.
20. Laurant M, Harmsen M, Wollersheim H, Grol R, Faber M, Sibbald B. The impact of nonphysician clinicians: do they improve the quality and cost-effectiveness of health care services? Med Care Res Rev . 2009;66(suppl 6):36S-89S. doi: 10.1177/1077558709346277.
21. Lenz ER, Mundinger MO, Kane RL, Hopkins SC, Lin SX. Primary care outcomes in patients treated by nurse practitioners or physicians: two-year follow-up. Med Care Res Rev . 2004;61(3):332-351.
22. Mundinger MO, Kane RL, Lenz ER, et al. Primary care outcomes in patients treated by nurse practitioners or physicians: a randomized trial. JAMA . 2000;283(1):59-68.
23. Obman-Strickland PA, Orzano AJ, Hudson SV, et al. Quality of diabetes care in family medicine practices: influence of nurse-practitioners and physician’s assistants. Ann Fam Med . 2008;6(1):14-22. doi: 10.1370/afm.758.
24. Essary AC, Green EP, Gans DN. Compensation and production in family medicine by practice ownership. Health Serv Res Manag Epidemiol . 2016;3:1-5. doi: 10.1177/2333392815624111.
25. Roblin DW, Howard DH, Becker ER, Adams EK, Roberts MH. Use of midlevel practitioners to achieve labor cost savings in the primary care practice of an MCO. Health Serv Res . 2004;39(3):607-626.
26. Hughes DR, Jiang M, Duszak R Jr. A comparison of diagnostic imaging ordering patterns between advanced practice clinicians and primary care physicians following office-based evaluation and management visits. JAMA Intern Med . 2015;171(1):101-107. doi: 10.1001/jamainternmed.2014.6349.
27. Gidwani R, Sinnott P, Avoundjian T, Lo J, Asch SM, Barnett PG. Inappropriate ordering of lumbar spine magnetic resonance imaging: are providers choosing wisely? Am J Manag Care . 2016:22(2):e68-e76.
28. Cipher DJ, Hooker RS, Guerra P. Prescribing trends by nurse practitioners and physician assistants in the United States. J Am Acad Nurse Pract . 2006;18(6):291-296.
29. Ladd E. The use of antibiotics for viral upper respiratory tract infections: an analysis of nurse practitioner and physician prescribing practices in ambulatory care, 1997-2001. J Am Acad Nurse Pract . 2005;17(10):416-424.
30. National Ambulatory Medical Care Survey: 2010 summary tables. CDC National Center for Health Statistics website. http://www.cdc.gov/nchs/data/ahcd/namcs_summary/2010_namcs_web_tables.pdf. Accessed October 2, 2015.
31. Daubresse M, Chang HY, Yu Y, et al. Ambulatory diagnosis and treatment of non-malignant pain in the United States, 2000-2010. Med Care . 2013;51(10):870-878. doi: 10.1097/MLR.0b013e3182a95d86.
32. Mafi JN, McCarthy EP, Davis RB, Landon BE. Worsening trends in the management and treatment of back pain. JAMA Intern Med . 2013;173(17):1573-1581. doi: 10.1001/jamainternmed.2013.8992.
33. Barnett ML, Linder JA. Antibiotic prescribing for adults with acute bronchitis in the United States, 1996-2010. JAMA . 2014;311(19):2020-2022. doi: 10.1001/jama.2013.286141.
34. Barnett ML, Linder JA. Antibiotic prescribing to adults with sore throat in the United States, 1997-2010. JAMA Intern Med . 2014;174(1):138-140. doi: 10.1001/jamainternmed.2013.11673.
35. Grijalva CG, Nuorti JP, Griffin MR. Antibiotic prescription rates for acute respiratory tract infections in US ambulatory care settings. JAMA . 2009;302(7):758-766. doi: 10.1001/jama.2009.1163.
36. Lee GC, Reveles KR, Attridge RT, et al. Outpatient antibiotic prescribing in the United States: 2000 to 2010. BMC Med . 2014;12:96. doi: 10.1186/1741-7015-12-96.
37. Nakhoul GN, Hickner J. Management of adults with acute streptococcal pharyngitis: minimal value for backup strep testing and overuse of antibiotics. J Gen Intern Med. 2013;28(6):830-834. doi: 10.1007/s11606-012-2245-8.
38. Steinman MA, Landefeld CS, Gonzales R. Predictors of broad-spectrum antibiotic prescribing for acute respiratory tract infections in adult primary care. JAMA . 2003;289(6):719-725.
39. Liu H, Robbins M, Mehrotra A, et al. The impact of using mid-level providers in face-to-face primary care on health care utilization. Med Care . 2017;55(1):12-18.
40. Halter M, Drennan V, Chattopadhyay K, et al. The contribution of physician assistants in primary care: a systematic review. BMC Health Serv Res . 2013;13:223. doi: 10.1186/1472-6963-13-223.
41. Austin PC, Tu JV. Bootstrap methods for developing predictive models in cardiovascular research. Am Stat . 2004;58(2):131-137. doi: 10.1198/0003130043277.
42. D’Agostino RB Jr. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med . 1998;17(19):2265-2281.
43. Rubin DB. Estimating causal effects from large data sets using propensity scores. Ann Intern Med . 1997;127(8 pt 2):757-763.
44. Liang S-Y, Eaton L, Pu J, Chen T, Luft H. Variations in prescription fills in an insured population. Poster presented at: AcademyHealth, Annual Research Meeting; June 15, 2015; Minneapolis, MN. https://academyhealth.confex.com/academyhealth/2015arm/meetingapp.cgi/Session/1814. Accessed June 23, 2016.
45. Larson EH, Hart LG, Ballweg R. National estimates of physician assistant productivity. J Allied Health . 2001;30(3):146-152. 

Download PDF: Provider Type and Management of Common Visits in Primary Care

Institutional Practices for Charitable Medication Access for Uninsured Patients
Analysis of a patient sample enrolled in charitable care at an academic medical center revealed that chronic medications were variably filled at a significant cost.

A Pulmonologist on Why You Should Think About Respiratory Health and the Lungs
On this episode of Managed Care Cast, we speak with MeiLan K. Han, MD, MS, the author of a book released this month called Breathing Lessons: A Doctor’s Guide to Lung Health. Han, a pulmonologist, gives an inside tour of the lungs and how they work, zooms out to examine the drivers of poor respiratory health, and addresses policy changes that are needed to improve lung health.
Trends in Low-Value Cancer Care During the COVID-19 Pandemic
Among adults with newly diagnosed cancer, rates of low-value cancer services persisted throughout the COVID-19 pandemic in areas ranging from peridiagnosis imaging to end-of-life care.

How Can Digital Care Programs Aid Those With Chronic Musculoskeletal Pain?
On this episode of Managed Care Cast, we speak with Jeffrey Krauss, MD, chief medical officer of Hinge Health and Stanford Clinical assistant professor, about the efficacy of a 12-week digital care program aimed to reduce lower back and knee pain in a real-world population.

Study: 1 in 6 US Patients With COPD Suffer From Cost-Related Medication Nonadherence
Medication nonadherence among patients with chronic obstructive pulmonary disease (COPD) is associated with increasing COPD symptoms, hospitalizations, morbidity, mortality, and health care expenditures.
Prices and Complications in Hospital-Based and Freestanding Surgery Centers
Average prices are substantially higher but rates of complications are similar in hospital-based vs freestanding surgery centers for colonoscopy, arthroscopy, and cataract removal surgery.
2 Commerce Drive Cranbury, NJ 08512
609-716-7777
- Research article
- Open access
- Published: 19 November 2022
The association between video or telephone telemedicine visit type and orders in primary care
- Nathan Juergens ORCID: orcid.org/0000-0002-5227-5730 1 , 2 ,
- Jie Huang 3 ,
- Anjali Gopalan 1 , 3 ,
- Emilie Muelly 1 , 3 &
- Mary Reed 3
BMC Medical Informatics and Decision Making volume 22 , Article number: 302 ( 2022 ) Cite this article
1958 Accesses
10 Citations
1 Altmetric
Metrics details
Introduction
Telemedicine is increasingly relied upon for care delivery in primary care, but the impact of visit type on clinical ordering behavior is uncertain.
Within Kaiser Permanente Northern California, we identified patients who self-scheduled and completed telemedicine encounters with their personal primary care provider or another available primary care provider in the same medical group, between April 1st, 2020, and October 31st, 2020, while physical distancing restrictions for COVID-19 were in place. We collected patient sociodemographic and clinical characteristics, measures of technology access, and categorized the most common primary encounter diagnoses. We measured proportions of patient-scheduled video versus telephone visits for each of eight diagnosis groups (Skin & Soft Tissue, Musculoskeletal Pain, Back Pain, General Gastrointestinal, Hypertension & Diabetes, Mental Health, Upper Respiratory, and Abdominal Pain), and compared physician orders for medications, antibiotics, lab and imaging studies by visit type within each diagnosis group.
There were 273,301 included encounters, with 86,676 (41.5%) video visits and 122,051 (58.5%) telephone visits. Of the diagnosis groups, Skin & Soft Tissue conditions had the highest proportion of video visits (59.7%), while Mental Health conditions had the highest proportion of telephone visits (71.1%). After adjusting for covariates, the overall rates of medication orders (46.6% vs. 44.5%), imaging orders (17.3% vs. 14.9%), lab orders (19.5% vs. 17.2%), and antibiotic orders (7.5% vs. 5.2%) were higher during video visits as compared to telephone visits ( p < 0.05). The largest difference within diagnosis groups was for Skin & Soft Tissue conditions, where the rate of medication orders was 9.1% higher than during video visits than telephone visits (45.5% vs. 36.5%, p < 0.05).
Conclusions
We observed statistically significant differences in clinician orders by visit type during telemedicine encounters for common primary care conditions. Our findings suggest that, for certain conditions, visual information conveyed during video visits may promote clinical work-up and treatment.
Peer Review reports
Telemedicine has the opportunity to increase access to health care, particularly for those patients with barriers to traditional care models [ 1 , 2 ]. The availability of high-fidelity digital devices has increased the potential of remote care and has made barriers to widespread implementation less daunting [ 3 ]. Today, in many health care organizations, patients are able to interact with medical providers through video and telephone visits or with asynchronous secure messaging.
The shift of health care communication from traditional in-person visits to these relatively novel mediums may impact clinical decision-making. How, and to what degree, physician behavior changes as a result of remote visits has not been extensively studied. The limited data that does exist suggests physicians may prescribe more medicines, particularly antibiotics, during telemedicine encounters than in-person visits for the same diagnoses[ 4 , 5 , 6 ]. There is also evidence that adherence to clinical guidelines is less consistent when comparing telemedicine to in-office encounters, a somewhat concerning finding [ 6 , 7 ].
The influence of the specific telemedicine modality on prescribing behavior has also not been thoroughly investigated. While clinician-specific characteristics have been associated with likelihood of prescription during telemedicine visits, and there have been comparisons of guideline-adherent orders between multiple virtual visit health care companies, the association between video versus telephone encounter on prescription patterns has not been studied [ 8 , 9 ]. Of note, many studies of prescribing practices during remote encounters have had small sample size and have been conducted on stand-alone, direct-to-consumer telemedicine companies, a model of care that does not foster continuity and which may also influence rates of prescriptions independent of visit modality [ 6 , 7 , 10 ].
The COVID-19 pandemic added urgency and import to the study of telemedicine and its effects on population health. Following the announcement of physical distancing measures, a large proportion of non-urgent outpatient visits shifted to telemedicine. One major medical system reported an 80% decrease in clinic visits and a more than 4000% increase in daily virtual visits over the first weeks of the pandemic [ 11 ]. Both patients and providers were essentially forced by the pandemic emergency to rapidly adjust to remote care.
An increasing number of clinical decisions are occurring via telemedicine, but the effect of virtual care visit type on the diagnostics and treatments patients receive is still uncertain [ 12 ]. The goal of our study was to observe patients choice of video versus telephone visits for the most common primary care conditions, and to investigate the differences in physician ordering by these visit types. We hypothesized that there would be meaningful differences in orders by visit type and that those differences would vary depending on how important visual information was to the primary condition in question.
Study setting
Kaiser Permanente Northern California (KPNC) is a large integrated health care organization. Since 2016, KPNC patients have been able to schedule primary care appointments through an online patient portal, with the option to choose an in-person, video, or telephone visit. Patients have the option to schedule appointments with their personal primary care provider, or with another available clinician within the study setting. All available providers have experience with and access to the necessary technologies to conduct either telephone or video visits. The option to schedule an in-person office visit was not offered through the online portal after COVID-19 restrictions were enacted in March, 2020, thus patients chose between telephone or video visit when scheduling a primary care appointment.
Population and measures
Using data from the KPNC electronic health record (EHR), we examined all completed video or telephone primary care telemedicine appointments scheduled through the patient portal between April 1st, 2020 and October 31st, 2020 for patients 18 years of age or older (Fig. 1 ). For each patient who completed at least one telemedicine visit during this interval, we collected sociodemographic characteristics from the EHR (age, sex, race/ethnicity, and English language proficiency). We identified whether patients had completed a video visit or accessed the online patient portal from a mobile device in the prior 365 days, as a measure of technology access. Additionally, based on the patients’ residential addresses, we categorized patients as living in a neighborhood with low socioeconomic status (SES) using 2010 US census block group data. We also categorized patients as living in a neighborhood with greater than or equal to 80% broadband connectivity versus less than 80% connectivity using FCC census tract level data [ 13 ].

Patient cohort and study design
We acquired patient and visit-level clinical data, including patient comorbidities, the primary encounter diagnosis (using codes from the International Classification of Diseases, Tenth Revision (ICD-10)), whether the visit was with a patient’s personal primary care provider (PCP) or a different clinician, the visit type (video or telephone), KPNC medical center through which the visit occurred. Lastly, for each encounter we identified whether there were any associated medicine prescriptions (with an additional indicator for specifically an antibiotic prescription), as well as any associated laboratory or imaging orders.
Diagnosis groups
To isolate the difference in provider ordering behavior by visit type, we grouped encounter diagnoses by organ system and clinical pathway, with organizational guidance from the Medical Dictionary for Regulatory Activities (MedDRA). To focus our analysis on the most common conditions managed in primary care, we initially categorized all the diagnoses in our data set with at least 1,000 associated encounters. This represented 140 unique primary ICD-10 diagnoses and 63.7% of all encounters initially included in the data set. To validate our diagnosis groups, five physicians independently categorized the diagnoses. We measured inter-rater reliability using Randolph’s free-marginal multi-rater Kappa score (overall Kappa = 0.91, 95% CI 0.87–0.94, and within diagnosis groups included in the final analysis Kappa = 0.96, 95% CI 0.92–0.99) [ 14 ].
We included the most common eight primary care diagnosis groups in this study. In order of frequency, these were 1- Skin & Soft Tissue, 2—Musculoskeletal (MSK) Pain, 3—Back Pain, 4—General Gastrointestinal (GI), 5—Hypertension (HTN) & Diabetes (DM), 6—Mental Health, 7—Upper Respiratory, and 8—Abdominal Pain (see Additional file 1 for full list of grouped ICD-10 codes). We excluded two common diagnosis groups for methodological reasons. We chose not to analyze prevention and screening visits because this was too broad and diverse a clinical category to interpret differences in ordering by visit-level variables. We also did not analyze visits with a primary diagnosis of COVID-19 or related ICD-10 codes, because these patients were triaged toward specific clinical pathways largely independent of clinician choice and the guidelines for management changed multiple times during the course of our study period.
Statistical analysis
Within each diagnosis group, we used multivariate logistic regression to examine the association between visit type (video vs. telephone) and clinician orders, adjusting for the sociodemographic, comorbidity and visit-level variables mentioned previously. We included an identifier for patients with repeat encounters for the same primary diagnosis and adjusted for this in our models. We reported adjusted rates calculated by marginal standardization with 95% confidence intervals (CI) [ 15 ].
This study was approved by the KPNC Institutional Review Board, and because it only involved retrospective data analysis, the requirement for written informed consent was waived for all patient participants.
During our study period, there were 809,146 completed adult primary care telemedicine encounters within KPNC. Of these encounters, 482,740 (59.7%) were telephone visits and 326,406 (40.3%) were video visits. There were 273,301 encounters with primary diagnoses included in the final diagnosis group analyses among 172,040 patients. The proportion of each visit type within this sample was comparable to all telemedicine encounters, with 122,051 (58.5%) telephone visits and 86,676 (41.5%) video visits. There were 209,106 (76.5%) encounters completed with a patient’s personal PCP, compared to 64,195 (23.5%) completed with another clinician (Table 1 ).
The most frequent diagnosis category in our study was Skin and Soft Tissue (18.0%), followed by Musculoskeletal Pain (17.1%), Back Pain (14.8%), General Gastrointestinal (13.4%), Hypertension & Diabetes (13.2%), Mental Health (10.4%), Upper Respiratory (7.2%), and Abdominal Pain (5.9%) (Table 1 ). Skin and Soft Tissue was the only group with more video (59.7%) than telephone visits, while the other seven groups included majority telephone encounters. Mental Health conditions had the highest proportion of telephone (71.1%) of any group (Fig. 2 ).

Proportions of telephone and video visits, by diagnosis group. Notes: Percentages shown are within group proportions. Abbreviations: HTN, Hypertension; DM, Diabetes; GI, Gastrointestinal; MSK, Musculoskeletal
Orders for medications were frequently associated with encounters for Upper Respiratory (59.9%), Mental Health (56.7%), Hypertension & Diabetes (47.1%), General Gastrointestinal (42.8%), and Skin & Soft Tissue (44.7%) conditions, though these groups generated comparatively few imaging orders (2.3%, 1.0%, 4.4%, 3.5%, and 1.6%, respectively). An imaging study was ordered during 36.9% of visits for Musculoskeletal Pain compared to only 18.8% of visits for Back Pain. The majority of diagnosis groups had very low rates (less than 3%) of orders for an antibiotic medicine, with the exception of Upper Respiratory (32.6%) and Skin & Soft Tissue (15.7%) conditions.
After adjustment, overall we found video visits were significantly associated with higher rate of clinician orders across each order type assessed, with 2.1% higher rate of a medication order (46.6% vs. 44.5%), 2.3% higher rate of a lab order (19.5% vs. 17.2%), 2.4% higher rate of an imaging order (17.3% vs. 14.9%), and 2.3% higher rate of an antibiotic order (7.5% vs. 5.2%) during video visits compared to telephone visits ( p < 0.05 for each). Within the diagnosis groups we observed a similar trend. Compared to telephone visits for the same conditions, there were significantly higher rates of medication orders during video visits for Skin & Soft Tissue (45.3% vs. 36.3%) and Musculoskeletal Pain (25.1% vs. 22.4%) conditions, significantly higher rates of lab orders during video visits for Musculoskeletal Pain (15.6% vs. 12.6%), Hypertension & Diabetes (37.8% vs. 30.0%), Back Pain (12.3% vs. 8.5%), Abdominal Pain (53.8% vs. 46.8%), General Gastrointestinal (36.3% vs. 30.0%), and Mental Health (15.1% vs. 8.4%) conditions, significantly higher rates of imaging orders during video visits for Musculoskeletal Pain (47.4% vs. 42.9%), Hypertension & Diabetes (9.6% vs. 4.6%), Back Pain (27.8% vs. 23.2%), and Abdominal Pain (28.4% vs. 22.5%) conditions, and significantly higher rates of antibiotic orders during video visits for Skin & Soft Tissue (17.0% vs. 13.6%) conditions ( p < 0.05 for each, Fig. 3 ).
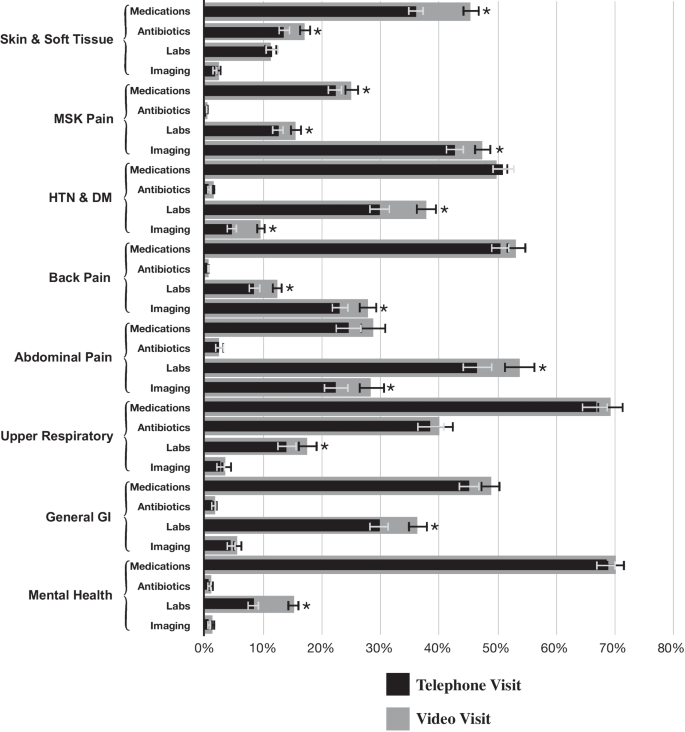
Predicted probabilities of clinician orders for common primary care diagnoses, by visit type. Notes: Percentages shown are predicted probabilities, adjusted for all patient and encounter covariates. Error bars show 95% confidence intervals, and asterisks (*) represent two-sided p < 0.05. Abbreviations: HTN, Hypertension; DM, Diabetes; GI, Gastrointestinal; MSK, Musculoskeletal
In this study, we present cross-sectional observations on a large cohort of adults accessing care via telemedicine for common primary care conditions during the COVID-19 pandemic. We found video visits were consistently associated with a higher rate of orders compared to telephone visits.
The largest observed difference in rate of orders between video and telephone telemedicine across all diagnosis groups and order types was for medication orders for Skin & Soft Tissue conditions; the diagnosis of dermatologic disease depends on visualizing the patient, so this was a predictable finding. Despite the relatively high rate of antibiotic prescriptions, we did not observe a significant ordering difference between video and telephone visits for Upper Respiratory conditions. This is somewhat reassuring given prior research suggesting an increase in inappropriate antibiotic ordering during telemedicine encounters [ 6 ]. With the exception of difference in medication orders for Skin & Soft Tissue and Musculoskeletal Pain, all of the other statistically significant differences in order rate were for lab and imaging orders, which are for the diagnosis or management of disease rather than for treatment. The reasons why video visits may result in additional work-up of disease compared to telephone and the appropriateness of these ordering differences remain unknown and warrant further investigation.
Patient choice of visit type by diagnosis group also offers insights. The group with the highest proportion of video visits was Skin & Soft Tissue, while Mental Health had the highest proportion of telephone visits; again, this is consistent with the type of information required to diagnose and manage these conditions, and it seems patients in our study population understood this when scheduling visits. Musculoskeletal Pain diagnoses had the second highest proportion of video visits of any group, and the musculoskeletal physical exam has also been shown to translate well to remote video visits [ 16 ].
To our knowledge, this is one of the only studies investigating the association between video and telephone telemedicine visit type and clinical orders and is certainly the largest in sample size. Given the magnitude, even the modest differences in clinical orders we observed in our cohort represent thousands of medications, labs or imaging studies. Our data do not indicate whether the ordering differences observed were appropriate or not, for example, whether clinicians ordered more medications than indicated during video visits or, alternatively, fewer than indicated during telephone visits; that is outside of the scope of this analysis and should be investigated further in future research. Also, given the period of our study, directly contrasting our findings to orders associated with in-person primary care visits was not feasible, though a prior study by our group on patient encounters between January 2016 and May 2018 found comparable rates of medication, lab and imaging orders [ 17 ].
As just alluded to, it should be emphasized that this study occurred during the COVID-19 pandemic, a public health emergency. In order to maintain access to care and prevent exposure to the coronavirus, in March of 2020, the Centers for Medicare & Medicaid Services (CMS) broadened reimbursement for telemedicine [ 18 ]. This expanded coverage has been extended through the end of 2021, but it is not yet clear what telehealth services will be reimbursed long-term, in-particular whether CMS will continue to reimburse for telephone visits at the same rate as video visits [ 19 , 20 ]. In our study, we did observe differences in clinical behavior between video and telephone visits for common primary care diagnoses, though many of the differences were relatively small, and for some order types and diagnosis groups, there were no differences between the two visit modalities. These findings may help inform policymakers when deciding on the future of telemedicine reimbursement.
Limitations
Our study has several limitations. First, the visits in our dataset were self-scheduled by the patients. This raises the possibility that the differences we observed in order rate by visit type were not due to differences in telecommunication modality, but, rather, because of differences in clinical severity between patients who chose video versus telephone visits. While we adjusted for a large variety of patient and clinical variables and attempted to compare ordering within diagnostic groups with limited ranges of severity, we cannot exclude the possibility of this confounder.
Additionally, our data contain a substantial subset of individual patients with multiple telemedicine encounters. While this is not unexpected given the duration of our study, we know that the rate of clinician orders is likely impacted by repeat visits for the same condition, for example, a subsequent visit monitoring the effect of a new prescription may generate different orders than a follow-up visit to discuss the results of a recent lab or imaging study. We adjust for repeat visits for the same ICD-10 diagnosis in our models, but it is possible that due to coding variability we did not fully capture these longer term episodes of care. Lastly, as with any retrospective data study, the observed associations cannot be used to attribute causation.
In this study of remote visits for common primary care conditions, we found a subtle but statistically significantly higher in the rate of medication, antibiotic, lab and imaging orders during video visits compared to telephone visits. There was some nuance within diagnosis groups, but the overall trend was consistent. Video visits offer clinicians visual information about their patients while telephone visits do not, and there are many diagnoses and triaging decisions that rely on such visual information.
Physician prescribing behavior is difficult to study; it is a complex behavior dependent on multiple inputs, including personal and patient characteristics, medical experience, health care organization, reimbursement model, trends in scientific literature, as well as the modality by which providers and patients interact.
This study was an initial attempt to examine how different forms of telemedicine may impact clinical behavior in remote primary care. Future research focused on more narrow clinical areas should further explore the specific orders (e.g. abdominal CT scans, blood chemistries, opioid pain relievers) that comprise the differences between video and telephone visits within relevant diagnosis groups. This would allow for a better understanding of whether the ordering differences observed are appropriate and/or guideline concordant.
We found that video telemedicine visits appear to generate more clinical actions than telephone visits, particularly in clinical areas where visual information is likely to be particularly useful. Further examination of clinical usefulness of video communication between patients and physicians is needed to best utilize telemedicine beyond the pandemic period for ongoing primary care practice.
Availability of data and materials
The datasets generated and analyzed during the current study are not publicly available as they contain protected health information and individual privacy could be compromised, but can be made available in a de-identified manner from the corresponding author on reasonable request.
Abbreviations
Kaiser Permanente Northern California
Electronic health record
Socioeconomic status
Federal Communications Commission
Primary care provider
International Classification of Diseases
Medical Dictionary for Regulatory Activities
Musculoskeletal
Gastrointestinal
Hypertension
Confidence intervals
Ackerman MJ, Filart R, Burgess LP, Lee I, Poropatich RK. Developing next-generation telehealth tools and technologies: Patients, systems, and data perspectives. Telemedicine e-Health. 2010;16(1):93–5. https://doi.org/10.1089/tmj.2009.0153 .
Article PubMed PubMed Central Google Scholar
WHO. Telemedicine: Opportunities and developments in member states: Report on the second global survey on ehealth. WHO Press 12/06/2020 2010.
Dorsey ER, Topol EJ. State of telehealth. N Engl J Med. 2016;375(2):154–61. https://doi.org/10.1056/nejmra1601705 .
Article PubMed Google Scholar
Mehrotra A, Paone S, Martich GD, Albert SM, Shevchik GJ. A comparison of care at e-visits and physician office visits for sinusitis and urinary tract infection. JAMA Intern Med. 2013;173(1):72. https://doi.org/10.1001/2013.jamainternmed.305.Accessed2020-12-14T23:44:07 .
Moth G, Huibers L, Christensen MB, Vedsted P. Drug prescription by telephone consultation in danish out-of-hours primary care: a population-based study of frequency and associations with clinical severity and diagnosis. BMC Fam Pract. 2014;15(1):142. https://doi.org/10.1186/1471-2296-15-142.Accessed2020-12-14T23:38:34 .
Ray KN, Shi Z, Gidengil CA, Poon SJ, Uscher-Pines L, Mehrotra A. Antibiotic prescribing during pediatric direct-to-consumer telemedicine visits. Pediatrics. 2019;143(5). doi: https://doi.org/10.1542/peds.2018-2491 .
Jain T, Lu RJ, Mehrotra A. Prescriptions on demand the growth of direct-to-consumer telemedicine companies. JAMA September. 2019;10:925–925. https://doi.org/10.1001/jama.2019.9889 .
Article Google Scholar
Liu S, Edson B, Gianforcaro R, Saif K. Multivariate analysis of physicians' practicing behaviors in an urgent care telemedicine intervention. AMIA Annual Symposium proceedings AMIA Symposium. 2019;2019:1139–1148. /pmc/articles/PMC7153110/?report=abstract. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7153110/ .
Schoenfeld AJ, Davies JM, Marafino BJ, et al. Variation in quality of urgent health care provided during commercial virtual visits. JAMA Intern Med. 2016;176(5):635. https://doi.org/10.1001/jamainternmed.2015.8248.Accessed2020-12-14T23:36:50 .
Resneck JS, Abrouk M, Steuer M, et al. Choice, transparency, coordination, and quality among direct-to-consumer telemedicine websites and apps treating skin disease. JAMA Dermatol. 2016;152(7):768. https://doi.org/10.1001/jamadermatol.2016.1774.Accessed2020-12-14T20:24:14 .
Mann DM, Chen J, Chunara R, Testa PA, Nov O, Mann D. Covid-19 transforms health care through telemedicine: evidence from the field. J Am Med Inform Assoc. 2020;Advanced Abstract. doi: https://doi.org/10.1093/jamia/ocaa072/5824298 .
Pappas Y, Vseteckova J, Mastellos N, Greenfield G, Randhawa G. Diagnosis and decision-making in telemedicine. J Patient Exp. 2019;6(4):296–304. https://doi.org/10.1177/2374373518803617 .
Reed ME, Huang J, Graetz I, et al. Patient characteristics associated with choosing a telemedicine visit vs office visit with the same primary care clinicians. JAMA Netw Open. 2020;3(6):e205873–e205873. https://doi.org/10.1001/jamanetworkopen.2020.5873 .
Warrens MJ. Inequalities between multi-rater kappas. Adv Data Anal Classif. 2010;4(4):271–86. https://doi.org/10.1007/s11634-010-0073-4.Accessed2021-05-08T05:53:09 .
Muller CJ, Maclehose RF. Estimating predicted probabilities from logistic regression: different methods correspond to different target populations. Int J Epidemiol. 2014;43(3):962–70. https://doi.org/10.1093/ije/dyu029 .
Tenforde AS, Iaccarino MA, Borgstrom H, et al. Telemedicine during covid-19 for outpatient sports and musculoskeletal medicine physicians. PM&R. 2020;12(9):926–32. https://doi.org/10.1002/pmrj.12422 .
Reed ME, Huang J, Graetz I, et al. Treatment and follow-up care associated with patient-scheduled primary care telemedicine and in-person visits in a large integrated health system. JAMA Netw Open. 2021;4(11):e2132793. https://doi.org/10.1001/jamanetworkopen.2021.32793 .
Services CfMM. Medicare telemedicine health care provider fact sheet. 2020; https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet .
Koma W, Cubanski J, Neuman T. Medicare and telehealth: Coverage and use during the covid-19 pandemic and options for the future. Kaiser Family Foundation. 2021. https://www.kff.org/medicare/issue-brief/medicare-and-telehealth-coverage-and-use-during-the-covid-19-pandemic-and-options-for-the-future/ .
Uscher-Pines L, Sousa J, Jones M, et al. Telehealth use among safety-net organizations in california during the covid-19 pandemic. JAMA. 2021. https://doi.org/10.1001/jama.2021.0282 .
Download references
Acknowledgements
Thank you to Dr. Anke Hemmerling for advising during study design, data analysis, and manuscript preparation. Thank you to Dr. David Lee and Dr. Neha Luthar for helping to validate our diagnosis groups.
Funding was provided in part from the Agency for Healthcare Research and Quality grant ID #: 1R01HS025189-01A1. The funding body played no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and affiliations.
Department of Medicine, Kaiser Permanente Oakland Medical Center, Oakland, CA, USA
Nathan Juergens, Anjali Gopalan & Emilie Muelly
Department of Graduate Medical Education, Kaiser Permanente Oakland Medical Center, Oakland, CA, USA
Nathan Juergens
Division of Research, Kaiser Permanente Northern California, Oakland, CA, USA
Jie Huang, Anjali Gopalan, Emilie Muelly & Mary Reed
You can also search for this author in PubMed Google Scholar
Contributions
All authors have read and approved the manuscript. NJ, JH, and MR were involved in the conception, plan and design of the study. NJ performed the statistical analysis and wrote the manuscript with input from all authors. JH performed the data acquisition and helped with statistical analyses. AG and EM helped validate the methods, interpret the data, provided clinical expertise, and worked on manuscript revisions. MR is the principle investigator and was involved in all aspects of the study. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Nathan Juergens .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Kaiser Permanente Northern California Institutional Review Board. Its local reference number is CN-18-3235_01. Consent to participate was waived by the IRB due to minimal risk to the study subjects. No administrative permissions and/or licenses were acquired by our team to access the clinical data used in the study. All study methods and procedures adhere to the principles of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:.
Diagnosis Category ICD-10 Codes.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Juergens, N., Huang, J., Gopalan, A. et al. The association between video or telephone telemedicine visit type and orders in primary care. BMC Med Inform Decis Mak 22 , 302 (2022). https://doi.org/10.1186/s12911-022-02040-z
Download citation
Received : 22 October 2021
Accepted : 02 November 2022
Published : 19 November 2022
DOI : https://doi.org/10.1186/s12911-022-02040-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Telemedicine
- Primary care
- Clinical orders
BMC Medical Informatics and Decision Making
ISSN: 1472-6947
- General enquiries: [email protected]
The Different Types Of Visits And Patient Notes

Section 1: Routine Check-Ups And Progress Visits
Key notes for routine check-ups and progress visits:, section 2: emergency department visits, key notes for emergency department visits:, section 3: surgical and procedural visits, recommended reading : ai therapy & therapist using ai for better mental health journey, section 4: specialized consultations and referrals, key notes for specialized consultations and referrals:, section 5: telehealth and virtual visits, key notes for telehealth and virtual visits:, section 6: inpatient hospitalization and discharge visits, key notes for inpatient hospitalization and discharge visits:.
Weary of documentation ? Find out how S10.AI can benefit you.
Contact S10.AI
- Experience A Live Demo
- S10 Robot EHR Voice Dictation
- S10 Robot Medical Transcribe
- S10 Robot Medical Converscribe
- Product Comparison
- Buying Guide S10.AI
- On The Radar
WORLDWIDE HEADQUARTERS
NJ, Princeton - Carnegie Center
United States.
Privacy Policy
© 2024 S10.AI, Inc. All rights reserved.

Types of Doctors and Medical Specialists: Which One Should You See?
Learn about the different types of primary care doctors and medical specialists.
This article is based on reporting that features expert sources.
Types of Medical Specialists

Getty Images
Navigating the health care system is daunting, especially when determining which type of doctors or medical specialists to see for specific health concerns. Understanding the role of your primary care physician and various medical specialists will help you make informed decisions about your health care needs.
Learn about the different types of medical specialists and when you may need a referral to visit a specialty doctor.
Key Takeaways
- There are various types of primary care doctors, including internal medicine doctors, family medicine doctors and pediatricians.
- Primary care physicians can generally take care of a majority of medical cases.
- You may need to see a specialist in certain circumstances, such as if you have a chronic or complex disease, lab results that need expert interpretation, an uncertain diagnosis or a need or want for a second opinion.
- There are various medical specialists and subspecialists who are specifically trained in the diagnosis and treatment of certain types of diseases and conditions.
Primary Care Doctors
Primary care doctors are the entry point to the medical system. They provide a comprehensive approach to care, including prevention, treatment and rehabilitation of health issues. Primary care doctors also help coordinate care when you need to see a specialist.
Having a primary care doctor allows for an ongoing patient-doctor relationship built on mutual trust.
There are different types of primary care doctors :
- Internal medicine doctors. Also called an internist , internal medicine doctors manage common and complex illnesses typically for adults and older adults.
- Family medicine doctors. Family medicine doctors provide continuous care for people of all ages, backgrounds and conditions, often caring for entire families from birth through the end of life.
- Pediatricians. Pediatricians are a type of primary care doctor specializing in the care of infants, children and adolescents. They provide primary and preventive care, including administering routine immunizations or providing acute care for common childhood illnesses , like ear infections, colds and flu and minor injuries.
Starting with a visit to your primary care physician is a great way to assess whether or not you need to see a specialist.
“Sometimes, I’ll say to the patient, ‘I can take care of that. You don’t need to go to the specialist at this point in time,’” says Dr. Theodore Strange, chair of medicine at Staten Island University Hospital, a division of Northwell Health, in New York City.
In fact, upwards of 95% of cases can be taken care of with good primary care , says Dr. David Cutler, a board-certified family medicine physician at Providence Saint John’s Health Center in Santa Monica, California. “The referral itself is the exception,” he adds.
When to See a Medical Specialist
However, there are a few reasons doctors may refer patients to a specialist, including:
- If the patient has a certain chronic or complex disease with symptoms that may need specialist testing. For example, someone with a cardiac condition may need a stress test, or an individual with a GI condition may need a specific type of endoscopy or colonoscopy.
- If you have the results of testing and need a more expert interpretation of the test to better treat the case.
- If there’s a patient with an uncertain diagnosis. A primary care physician may refer you to a specialist if they have run out of options and need an expert with more specialized medical knowledge to diagnose and treat you.
- If you need or want a second opinion .
Types of Medical Specialists You Might Need
Medical specialists have additional training and expertise in a specific area of medicine. Some even subspecialize, meaning they have even more specialized training within their specific field of medicine.
Below are several common medical specialists you might see.
Allergists-immunologist
- What is an allergist-immunologist? An allergist-immunologist diagnoses, treats and manages disorders related to the immune system, immune deficiency diseases and adverse reactions to triggers, such as drugs or food.
What do allergists-immunologists treat? Allergist-immunologists treat allergic rhinitis (hay fever), food allergies , asthma, eczema, immunodeficiency disorders and other conditions related to the immune system.
Cardiologist
- What is a cardiologist? Cardiologists deal with the prevention and treatment of disorders of the heart and vascular system.
What do cardiologists treat? Cardiologists treat cardiac issues, such as coronary artery disease , heart failure, arrhythmias and congenital heart defects.
Dermatologist
- What is a dermatologist? Dermatologists are medical specialists trained in the diagnosis and management of conditions related to the skin, hair and nails.
What do dermatologists treat? Dermatologists treat a wide range of issues, including acne, rashes, eczema, psoriasis , skin infections and skin cancer . They may also treat patients with cosmetic concerns, such as wrinkles or acne scarring.
Endocrinologist
- What is an endocrinologist? Endocrinologists are doctors who focus on disorders related to the endocrine system , which involves the glands and organs that make hormones.
- What do endocrinologists treat? Endocrinologists treat patients with endocrine conditions and disorders, such as diabetes, thyroid disorders, metabolic abnormalities and hormonal imbalances .
Gastroenterologist
- What is a gastroenterologist? Gastroenterologists , or GI doctors, manage diseases of the gastrointestinal tract, including your esophagus, stomach, bowels, liver, pancreas and gallbladder.
What do gastroenterologists treat? Gastroenterologists treat GI conditions, like cancer , hepatitis, irritable bowel syndrome, diarrhea or constipation, heartburn and ulcers.
Geriatric medicine specialist
- What is a geriatric medicine specialist? Also referred to as geriatricians , specialty doctors of geriatric medicine have specialized knowledge related to aging and training in diagnostic, therapeutic, preventive and rehabilitative care for older adults.
- What do geriatric medicine specialists treat? Geriatric physicians treat conditions that may commonly occur with aging , such as cognitive decline, mobility issues, chronic diseases and medication management. They often collaborate with other health care professionals, such as physical and occupational therapists, mental health professionals and social workers.
Hematologist
- What is a hematologist? Hematologists focus on disorders related to the blood and blood-forming tissues and organs.
What do hematologists treat? Hematologists treat blood-related conditions, such as anemia , bleeding or clotting disorders and blood cancers.
Hospice and palliative medicine specialist
- What is a hospice and palliative medicine specialist? Hospice and palliative medicine specialists provide care and support to patients and their families as the patient navigates living with a serious or terminal illness.
- What do hospice and palliative medicine specialists treat? Hospice and palliative medicine specialists aim to prevent and alleviate suffering and to focus on improving quality of life for those with serious illness. This may include addressing physical, psychological, social and spiritual needs, such as administering pain management or end-of-life care . Common conditions treated include cancer, cardiovascular diseases and chronic obstructive pulmonary diseases, or COPD .
Infectious disease specialist
- What is an infectious disease specialist? Infectious disease specialists diagnose and treat infections caused by bacteria, viruses, fungi or parasites.
- What do infectious disease specialists treat? This medical specialist treats a wide range of infectious diseases, including HIV/AIDS , antibiotic-resistant infections and tuberculosis.
- What is a geneticist? These medical specialists diagnose and treat genetic disorders or conditions. Geneticists have special training in the study of genes and heredity.
- What do geneticists treat? Clinical geneticists care for patients in a clinical or research-based setting, and many geneticists counsel patients at risk for particular genetic disorders or cancers, such as sickle cell disease or hereditary breast and ovarian cancer .
Nephrologist
- What is a nephrologist? Nephrologists are medical doctors who treat disorders of the kidney.
What do nephrologists treat? Nephrologists treat patients with kidney-related disorders , including kidney stones, chronic kidney disease and kidney failure. They often provide related medical management and may oversee dialysis, kidney transplantation and postoperative care, and managing diabetes or high blood pressure .
Neurologist
- What is a neurologist? Neurologists are specialty doctors who diagnose and treat disorders of the nervous system, including the brain, spinal cord and nerves.
What do neurologists treat? Neurologists treat a range of disorders affecting the nervous system, including epilepsy, stroke, Alzheimer’s disease and other memory disorders , Parkinson’s disease and migraines.
Obstetrician-gynecologist
- What is an OB-GYN? An obstetrician-gynecologist specializes in the medical and surgical care of women related to pregnancy and childbirth and disorders of the female reproductive system.
What do OB-GYNs treat? In addition to pregnancy and childbirth, OB-GYNs specialize in women’s health issues, such as menopause , contraception (birth control), infertility, endometriosis and polycystic ovarian syndrome, or PCOS.
- What is an oncologist? Oncologists specialize in diagnosing and treating cancer .
What do oncologists treat? Oncologists manage several aspects of cancer care throughout the course of the disease and often consult with other specialists, like surgical oncologists, to develop treatment plans and provide care. These medical doctors often subspecialize in a particular type of cancer, such as breast oncology , neuro-oncology and radiation oncologists.
Ophthalmologist
- What is an ophthalmologist? Ophthalmologists are eye doctors who are medically trained to manage all aspects of eye and vision care , including medical and surgical treatments.
What do ophthalmologists treat? General ophthalmologists treat diseases and disorders of the eye, such as cataracts, glaucoma, eye infections, diabetic retinopathy and refractive errors. They can also prescribe glasses and contact lenses.
Orthopedist
- What is an orthopedist? A general orthopedist , or orthopedic surgeon , specializes in disorders and injuries of the musculoskeletal system, including bones, joints, ligaments, tendons and muscles.
What do orthopedists treat? Orthopedists may treat congenital deformities, traumatic or sports injuries, spinal disorders and degenerative diseases, as well as perform other types of orthopedic surgery .
Otolaryngologist
- What is an otolaryngologist? Commonly referred to as ear, nose and throat doctors, or ENTs, otolaryngologists are medical and surgical specialty doctors who diagnose and treat diseases and disorders of the head and neck.
What do otolaryngologists treat? Conditions ENTs treat may include chronic sinusitis, allergic or non-allergic rhinitis, gastrointestinal reflux , tonsillitis and sleep apnea .
Physical medicine and rehabilitation physician
- What is a physical medicine and rehabilitation physician? Also referred to as physiatrists , these doctors focus on the functioning of the whole patient, rather than specific organs or systems, to manage pain and restore function.
- What do physical medicine and rehabilitation physicians treat? Physiatrists treat conditions which may limit a person’s ability to function, such as amputation, brain injury, cerebral palsy, Parkinson’s disease or a spinal cord injury.
Plastic surgeon
- What is a plastic surgeon? Plastic surgeons subspecialize in performing procedures that restore, reconstruct or replace physical defects or functions.
- What do plastic surgeons treat? Plastic surgeons handle reconstructive procedures, like cleft lip and palate repair or breast reconstruction after mastectomy, as well as cosmetic procedures, such as rhinoplasty or facelift.
- What is a podiatrist? Podiatrists treat issues of the foot, ankle and lower extremities.
- What do podiatrists treat? Podiatrists manage conditions or injuries related to the lower extremities, such as sprains and fractures, plantar fasciitis , bunions, hammertoes and foot and ankle arthritis.
Psychiatrist
- What is a psychiatrist? A psychiatrist is a medical doctor who specializes in the evaluation and treatment of mental health, emotional and behavioral health disorders. They can prescribe medication and use other medical approaches to disease.
- What do psychiatrists treat? Psychiatrists see patients with mental, addictive and emotional disorders, such as psychotic disorders, mood disorders, anxiety disorders and substance use disorders.
Psychologist
- What is a psychologist? A psychologist is a mental health professional who treats mental, emotional and behavioral issues through therapy and counseling. Unlike psychiatrists, they cannot prescribe medication in most states. (Only Idaho, Illinois, Iowa, Louisiana and New Mexico allow psychologists with additional, specialized training to prescribe from an approved list of medications for certain emotional and mental health disorders, but they often collaborate with psychiatrists and other health providers.)
- What do psychologists treat? Similar to psychiatrists, psychologists work with patients with a variety of mental health disorders . They may also see people without clinical disorders who are feeling stressed or anxious to help them cope more effectively.
Pulmonologist
- What is a pulmonologist? Pulmonologists are medical specialists of the respiratory system.
What do pulmonologists treat? Pulmonologists manage serious or chronic diseases of the lungs and airways, such as emphysema, bronchitis , pneumonia, asthma and COPD.
Rheumatologist
- What is a rheumatologist? Rheumatologists are specialized medical doctors who diagnose and treat disorders related to your joints, muscles and connective tissues.
What do rheumatologists treat? Rheumatologists treat musculoskeletal diseases and systemic autoimmune conditions – referred to as rheumatic diseases – such as rheumatoid arthritis , osteoarthritis, lupus, fibromyalgia and gout .
Sleep medicine specialist
- What is a sleep medicine specialist? These medical specialists manage clinical sleep-related disorders and promote healthy sleeping habits.
What do sleep medicine specialists treat? Sleep medicine specialists use clinical assessment and physiologic testing to diagnose, manage and prevent sleep disorders , such as insomnia, narcolepsy, parasomnias, circadian rhythm disorders and sleep-related breathing disorders, like obstructive sleep apnea.

General surgeon
What is a general surgeon? General surgeons are trained in diagnosis, preoperative, operative and postoperative management in the nine primary components of surgery, which consist of the:
- Abdominal and pelvic organs.
- Breasts, skin and soft tissues.
- Head and neck.
- Cardiovascular system.
- Endocrine system.
- Surgical oncology.
- Critical care and emergency surgery.
What do general surgeons treat? General surgeons can perform surgical procedures for a wide range of conditions, including appendectomies, hernia repairs and gallbladder removals.
- What is a urologist? Urologists are doctors who deal with diseases of the male reproductive organs and the male and female urinary tract.
What do urologists treat? Urologists may treat kidney stones , urinary incontinence and erectile dysfunction .
Do You Need a Referral to See Specialists?
Whether or not you need a referral to see a specialist depends on your health insurance plan , your doctor or the type of specialist you’re trying to see.
Point of service, or POS, plans and health maintenance organizations, or HMOs, often require a primary care physician to work with your insurer for pre-approval to visit a specialist. The referral also likely needs to be for a specialist within your insurance network. If you’re unsure whether or not you need a referral, check with your insurance company first. Otherwise, your plan may not cover the care and you’ll get stuck with high out-of-pocket costs.
In addition to the patient’s health insurance coverage, symptoms , medical history and diagnostic testing and results, primary care physicians will likely take these factors into consideration when making a referral:
- Accessibility . It's important for the specialist to be geographically accessible to the patient.
- Availability . Some specialists can take months to make an appointment with, so referring doctors take their availability into consideration.
- Coordination of care . When physicians are part of a broader health network, they’ll likely recommend a specialized doctor within the same network. One benefit is shared electronic medical records, which helps streamline follow-up coordination of care.
Patient preferences or needs . Doctors may discuss options with a patient, taking their particular values, personal preferences or individual needs into account to ensure the referral aligns with their goals.
The U.S. News Health team delivers accurate information about health, nutrition and fitness, as well as in-depth medical condition guides. All of our stories rely on multiple, independent sources and experts in the field, such as medical doctors and licensed nutritionists. To learn more about how we keep our content accurate and trustworthy, read our editorial guidelines .
Cutler is a board-certified family medicine physician at Providence Saint John’s Health Center in Santa Monica, California.
Strange is the chair of medicine at Staten Island University Hospital, a division of Northwell Health, in New York City.
Tags: women's health , men's health , children's health , senior health , health care , family health , doctors , patient advice
health disclaimer »
Disclaimer and a note about your health », you may also like, medicare mistakes.
Elaine Hinzey April 9, 2024

Dementia Care: Tips for Home Caregivers
Elaine K. Howley April 5, 2024

How to Find a Primary Care Doctor
Vanessa Caceres April 5, 2024

Symptoms of a Kidney Problem
Claire Wolters April 4, 2024

Allergies vs. Colds
Payton Sy April 4, 2024

Nervous Breakdowns: Signs and Symptoms
Heidi Godman and Paul Wynn April 1, 2024

Exercises for Osteoarthritis
Vanessa Caceres March 29, 2024

Symptoms of Magnesium Deficiency
Elaine K. Howley March 29, 2024

What Is the Always Hungry Solution Plan?

Best Things to Eat When Sick
Vanessa Caceres March 28, 2024


Simplified guidelines for coding and documenting evaluation and management office visits are coming next year. Learn how to apply the guidelines to some common visit types.
CAROL SELF, CPPM, CPC, EMT, KENT MOORE, AND SAMUEL L. CHURCH, MD, MPH, CPC, FAAFP
Fam Pract Manag. 2020;27(6):6-11
Author disclosures: no relevant financial affiliations disclosed.
Editor's note: In its 2021 Medicare Physician Fee Schedule, CMS released new guidance regarding coding for prolonged E/M services. This article has been updated accordingly.

The American Medical Association (AMA) has established new coding and documentation guidelines for office visit/outpatient evaluation and management (E/M) services, effective Jan. 1, 2021. The changes are designed to simplify code selection and allow physicians to spend less time documenting and more time caring for patients. Physicians and other qualified health professionals (QHPs) will be able to select the level of office visit using either medical decision making (MDM) alone or total time (excluding staff time) on the date of service. In addition, the history and physical exam will be eliminated as components of code selection, and code 99201 will be deleted (code 99211 will not change). (See “ E/M coding changes summary .”)
To follow up on the previous FPM article detailing these changes (see “ Countdown to the E/M Coding Changes ,” FPM , September/October 2020), we have applied the 2021 guidelines to some common types of family medicine visits, and we explain below how documentation using a typical SOAP (Subjective, Objective, Assessment, and Plan) note can support the chosen level of service.
In each vignette, we've arrived at a code based only on the documentation included in the note. It's possible that a more extensive note could support a higher level of service by further clarifying the physician's decision making. But we've analyzed each case through an auditor's lens and tried not to make any assumptions that aren't explicitly supported by the note.
Starting in January, physicians and other qualified health professionals will be able to select the level of office visit using either medical decision making alone or total time (excluding staff time) on the date of service.
Medical decision making is made up of three factors: problems addressed, data reviewed, and the patient's risk. The highest level reached by at least two out of three determines the overall level of the office visit.
If the visit was time-consuming, but the medical decision making did not rise to a high level, the physician or qualified health professional may want to code based on total time instead.
MEDICAL DECISION MAKING (MDM)
Starting in January, physicians will be able to select the level of visit using only medical decision making, with a revised MDM table. (See the table at https://www.ama-assn.org/system/files/2019-06/cpt-revised-mdm-grid.pdf .)
The four levels of MDM (straightforward, low, moderate, and high) will be maintained but will no longer be based on checkboxes or bullet points. The level of service will be determined by the number and complexity of problems addressed at the encounter, the amount and complexity of data reviewed and analyzed, and the patient's risk of complications and morbidity or mortality.
Here's what that looks like in practice:
STRAIGHTFORWARD MDM VIGNETTE
An established patient presents for evaluation of eye matting. The documentation is as follows:
Subjective: 16 y/o female presents with a 2-day history of bilateral eye irritation. She denies any fever or sick contacts. She started having a slight runny nose and cough this morning. She thinks the matting is a little better than yesterday. She wears daily disposable contacts but hasn't used them since her eyes have been bothering her. Her younger sibling has had similar symptoms for a few days.
Objective: Temperature 98.8, BP 105/60, P 58.
General: No distress. Does not appear ill.
HEENT: Mild bilateral conjunctival erythema without discharge. No tenderness over eye sockets. EOMI, PERRL.
Neck: No cervical lymph nodes palpated.
Lungs: Clear to auscultation.
Assessment: Viral conjunctivitis.
Plan: Reviewed likely viral nature of symptoms. Supportive and conservative treatment options reviewed, including eye cleaning instructions and contact lens precautions. Call the office if symptoms persist or worsen. Avoid use of contacts until symptoms resolve.
CPT code: 99212.
Explanation: Under the 2021 guidelines, straightforward MDM involves at least two of the following:
Minimal number and complexity of problems addressed at the encounter,
Minimal (in amount and complexity) or no data to be reviewed and analyzed,
Minimal risk of morbidity from additional diagnostic testing or treatment.
This is the lowest level of MDM and the lowest level of service physicians are likely to report if they evaluate the patient themselves (code 99211 will still be available for visits of established patients that may not require the presence of a physician).
In this fairly common scenario, the assessment and plan make it clear that the physician addressed a single, self-limited problem (“minimal” in number and complexity, per the 2021 MDM guidelines) for which no additional data was needed or ordered, and which involved minimal risk of morbidity.
Per the 2021 CPT guidelines, “For the purposes of medical decision making, level of risk is based upon consequences of the problem(s) addressed at the encounter when appropriately treated.” In this case, there is little risk of morbidity to this patient from the viral infection diagnosed by the physician.
It's possible the physician considered prescribing an antibiotic in this case, but decided against it. Options considered but not selected can be used as an element for “risk of complications,” but they should be appropriate and documented. There is no documentation in this note to indicate the physician made that decision. The documentation provided, therefore, does not support a higher level of service using MDM. But if the physician did make that decision and the ensuing conversation with the patient was time-consuming, the physician always retains the option to choose the level of service based on time instead.
LOW LEVEL OF MDM VIGNETTE
An established patient presents for follow-up for stable fatty liver. The documentation is as follows:
Subjective: 62 y/o female presents for follow-up of nonalcoholic fatty liver. She has no other complaints today and no other chronic conditions. She denies any fever, weight gain, swelling, or skin color changes. She also denies any confusion. She continues to work at her regular job and reports no difficulties there. She denies any unusual bleeding or bruising. Energy is good. Diagnosis was made three years ago, incidentally, on an ultrasound. Condition has been stable since the initial full evaluation.
Objective: BP 124/70, P 76, Temperature 98.7, BMI 26.
General: Well-appearing. Alert and oriented x 3.
Eyes: Sclera nonicteric.
Heart: Regular rate and rhythm; trace pretibial edema.
Abdomen: Soft, nontender, no ascites, liver margin not palpable.
Skin: No bruising.
Labs reviewed and analyzed: CBC normal, CMP with elevated AST (62 IU/ml) and ALT (50 IU/ml), PT/PTT normal.
Last ultrasound was 3 years ago.
Assessment: Nonalcoholic steatohepatitis, stable.
Plan: LFTs continue to be improved since initial diagnosis and 30-pound intentional weight reduction. Continue monitoring appropriate labs at 6-month intervals. Follow up in 6 months, or sooner if swelling, bruising, or confusion. Avoid alcohol. Continue weight maintenance. She is reassured her condition is stable and has no other questions or concerns, especially in light of her prior extensive education on the topic. I am arranging for hepatitis A and B vaccination. Discussed OTC medications, including vitamin E, and for now will avoid them.
CPT code: 99213
Explanation: Under the 2021 guidelines, low-level MDM involves at least two of the following:
Low number and complexity of problems addressed at the encounter,
Limited amount and/or complexity of data to be reviewed and analyzed,
Low risk of morbidity from additional diagnostic testing or treatment.
In this vignette, the patient has one stable chronic illness, which is an example of an encounter for problems low in number and complexity. The risk of complications from treatment is also low. The “Objective” section indicates review of three lab tests, which qualifies as a moderate amount and/or complexity of data reviewed and analyzed. However, the level of MDM requires meeting two of the three bullets above, so the overall level remains low for this vignette.
MODERATE LEVEL OF MDM VIGNETTE
An established patient with obesity and diabetes presents with new onset right lower quadrant pain. The documentation is as follows:
Subjective: 42 y/o female presents for evaluation of 2 days of abdominal pain. She has a history of Type 2 diabetes, controlled. Pain is moderate, 6/10 currently, and 10/10 at worst. The pain is intermittent. The pain is located in the back and right lower quadrant, mostly. She denies diarrhea or vomiting but does note some nausea. She denies fever. She denies painful or frequent urination. She is sexually active with her spouse. She has had a hysterectomy due to severe dysfunctional bleeding. She has not tried any medication for relief. No position seems to affect her pain. She has not had symptoms like this before. Home glucose checks have been in the 140s fasting. Her last A1C was 6.9% two months ago. Family history: Sister with a history of kidney stones.
Objective: BP 160/95, P 110, BMI 36.1.
General: Appears to be in mild to moderate pain. Frequently repositioning on exam table.
HEENT: Moist oral mucosa.
Abdomen: Mild right-sided tenderness. No focal or rebound tenderness. Normal bowel sounds. No CVA tenderness. No suprapubic tenderness. No guarding.
UA with microscopy: 3 + blood, no LE, 50–100 RBCs, 5–10 WBCs.
CBC, CMP, CT stone study ordered stat.
Assessment: Abdominal pain – suspect renal stone. Also consider cholecystitis, gastroparesis, gastroenteritis, appendicitis, and early small bowel obstruction.
Diabetes, type 2, controlled.
Obesity – this is a risk factor for gall-bladder problems, but still favor renal stone.
Plan: Ketorolac 60 mg given in office for pain relief. Hydrocodone/APAP prescription for pain relief. Discussed at length suspicion of renal stone. Will plan lab work and pain control and await CT stone study. Urine sent to reference lab for microscopy. Drink plenty of fluids. Urine strainer provided. Call the office if worsening or persistent symptoms. Await labs/CT for next steps of treatment plan. Will follow up with her if urology referral is indicated.
CPT code: 99214
Explanation: Under the 2021 guidelines, moderate level MDM involves at least two of the following:
Moderate number and complexity of problems addressed at the encounter,
Moderate amount and/or complexity of data to be reviewed and analyzed,
Moderate risk of morbidity from additional diagnostic testing or treatment.
In this vignette, the patient has one undiagnosed new problem with uncertain prognosis (abdominal pain) and two stable chronic conditions (diabetes and obesity). Either one (the new problem with uncertain prognosis or two stable chronic conditions) meets the definition of a moderate number and complexity of problems under the 2021 MDM guidelines. But they do not meet the threshold of a high number and complexity of problems, even when combined.
The physician reviews or orders a total of four tests, which again exceeds the requirements for a moderate amount and/or complexity of data, but doesn't meet the requirements for the high category.
The prescription drug management is an example of moderate risk of morbidity. One might argue that the risk of morbidity is high because renal failure could result from a major kidney stone obstruction. But even then the overall MDM would still remain moderate, because of the number and complexity of problems addressed and the amount and/or complexity of data involved.
HIGH LEVEL OF MDM VIGNETTE
An established patient with a new lung mass and probable lung cancer presents with a desire to initiate hospice services and forgo curative treatment attempts. The documentation is as follows:
Subjective: 92-year-old male presents for follow-up of hemoptysis, fatigue, and weight loss, along with review of his recent chest CT. He reports moderate mid-back pain, new since last week. Appetite is fair. He denies fever. He continues to have occasional cough with mixed blood in the produced sputum.
Objective: BP 135/80, P 95, Weight down 5 pounds from 2 weeks ago, BMI 18.5, O2 sat 94% on RA.
General: Frail-appearing elderly male. No distress or shortness of breath. Able to speak in full sentences.
HEENT: No palpable lymph nodes.
Lungs: Frequent coughing and diffuse coarse breath sounds.
Heart: Regular rate and rhythm.
Ext: No extremity swelling.
MSK: Moderate tenderness over multiple thoracic vertebrae.
CT shows large right-sided lung mass suspicious for malignancy, along with a moderate left-sided effusion. Lytic lesions seen in T6-8.
Assessment: Lung mass, suspect malignancy with bone metastasis.
Plan: After extensive review of the findings, the patient was informed of the likely poor prognosis of the suspected lung cancer. We reviewed his living will, and he reiterated that he did not desire life-prolonging measures and would prefer to allow the disease to run its natural course. He also declines additional testing for diagnosis/prognosis. A shared decision was made to initiate hospice services. Specifically, we discussed need for oxygen and pain control. He declines pain medications for now, but will let us know. He and his son who was accompanying him voiced agreement and understanding of the plan.
CPT code: 99215
Explanation: Under the 2021 guidelines, high level MDM involves at least two of the following:
High number and complexity of problems addressed at the encounter,
Extensive amount and/or complexity of data to be reviewed and analyzed,
High risk of morbidity from additional diagnostic testing or treatment.
In this vignette, the patient has one acute or chronic illness or injury (suspected lung cancer) that poses a threat to life or bodily function. This is an example of a high complexity problem in the 2021 MDM guidelines. The physician reviewed one test (CT), so the amount and/or complexity of data is minimal. A decision not to resuscitate, or to de-escalate care, because of poor prognosis is an example of high risk of morbidity, and the physician has clearly documented that in the plan portion of the note. Consequently, even though the amount and/or complexity of data is minimal, the overall MDM remains high because of the problem addressed and the risk involved.
Under the new guidelines, total time means all time (face-to-face and non-face-to-face) the physician or other QHP personally spends on the visit on the date of service. Examples include time spent reviewing labs or reports, obtaining or reviewing history, ordering tests and medications, and documenting clinical information in the EHR.
The AMA has also created a new add-on code, 99417, for prolonged services. It can be used when the total time exceeds that of a level 5 visit – 99205 or 99215. (See “ Total time plus prolonged services template .”)
TIME-BASED CODING VIGNETTE
An established patient presents with a three-month history of fatigue, weight loss, and intermittent fever, and new diffuse adenopathy and splenomegaly. The documentation is as follows:
Subjective: 30-year-old healthy male with no significant PMH presents with a three-month history of fatigue, weight loss, and intermittent fever. He travels for work and has been evaluated in several urgent care centers and reassured that he likely had a viral syndrome. Fevers have been as high as 101, but usually around 100.5, typically in the afternoons. Testing for flu and acute mono has been negative. He denies high-risk sexual behavior and IV drug use. He denies any sick contacts. He has not had vomiting or diarrhea. He has not had any pain. He denies cough.
Objective: BP 125/80, P 92, BMI 27.4.
General: Well-nourished male, no distress.
HEENT: No abnormal findings.
Lungs: Clear.
Heart: No murmurs. Regular rate and rhythm.
Abdomen: Soft, non-tender, moderate splenomegaly.
Skin: Multiple petechia noted.
Lymph: Multiple cervical, axillary, and inguinal lymph nodes that are enlarged, mobile, and non-tender.
Assessment: Weight loss, lymphadenopathy, and splenomegaly
Plan: Prior to the visit, I spent 15 minutes reviewing the medical records related to his recent symptoms and various urgent care visits. We reviewed the differential at length to include infectious disease and acute myelodysplastic condition. I have ordered stat blood cultures, TB test, EBV titers, echo, and CBC. The pathologist called to report concerning findings on the CBC for likely acute leukemia. I called the patient to inform him of his results and need for additional testing. I also discussed the patient with oncology and arranged a follow-up visit for tomorrow. I spent a total of 92 minutes with record review, exam, and communication with the patient, communication with other providers, and documentation of this encounter.
CPT Codes: 99215 and 99417 x 3.
Explanation: In this instance, the physician has chosen to code based on time rather than MDM. The physician has documented 92 minutes associated with the visit on the date of service, including time not spent with the patient (e.g., time spent talking with the pathologist and time spent in documentation). According to the 2021 CPT code descriptors, 40–54 minutes of total time spent on the date of the encounter represents a 99215 for an established patient.
The 2021 CPT code set also notes that for services of 55 minutes or longer, you should use the prolonged services code, 99417, which can be reported for each 15 minutes beyond the minimum total time of the primary service (99215). The difference between the 92 minutes spent by the physician and the 40-minute minimum for 99215 is 52 minutes. There are three full 15-minute units of 99417 in those 52 minutes, so the physician may report three units of 99417 in addition to 99215. CPT 2021 instructs you to not report 99417 for any time unit less than 15 minutes, so the seven remaining minutes of prolonged service is unreportable.
Note that if this had been a new patient, the physician would only be able to report two units of 99417 in addition to 99205. Though the elements of MDM do not differ between new and established patients, the total time thresholds do. The range for a level 5 new patient is 60–74 minutes.
FINAL THOUGHTS
CPT does not dictate how physicians document their patient encounters. As illustrated above, a standard SOAP note can be used to support levels of MDM (and thus levels of service) under the 2021 guidelines.
Physicians who want to further solidify their documentation in case of an audit may choose to make the elements of MDM more explicit in their documentation. This could be particularly helpful for documenting the level of risk, which is the least clearly defined part of the MDM table and potentially most problematic because of its inherent subjectivity. Stating the level of risk and giving a rationale when possible allows a physician to articulate in the note the qualifying criteria for the submitted code. For example, going back to our vignette of moderate MDM, the physician could note in the chart, “This condition poses a threat to bodily function if not addressed, due to acute kidney injury for an obstructive stone.”
It is also worth noting that much of the note in each case is for purposes other than documenting the level of service. For instance, with history and physical exam no longer required, the subjective and objective portions of the note are recorded primarily for continuity or quality of care rather than to justify the level of service. This provides some administrative simplification. What's in the note will become more about what is needed for medical care and less about payment justification under the new guidelines. That's a plus for primary care.
We hope these examples are helpful as you prepare to implement the 2021 CPT changes. You can also visit https://www.aafp.org/emcoding for more resources and information.
Continue Reading
More in FPM
More in pubmed.
Copyright © 2020 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

(818) 308-4108
5 Types of Patients and How to Deal With Them
If you work in healthcare, it means stepping into the world of handling different types of patients in hospitals, each presenting unique challenges. No two patients are the same, each demanding a specific approach. With that in mind, let’s discover some essential strategies to effectively deal with five most common patient types in medical settings, including understanding the patient type’s meaning in various contexts.
Benefits of Understanding Patient Types
By understanding patient types, healthcare providers can:
- Build rapport and trust with patients
- Improve patient satisfaction
- Enhance patient compliance with treatment plans
- Reduce the risk of medical errors
- Improve overall patient outcomes
The Compliant Patient
Compliant patients are considered the ideal. They follow their medication regimen just right, observe all appointments, and meticulously adhere to lifestyle changes suggested by their healthcare providers. While these patients seemingly make life easier, they also need specific attention.
One thing to remember is to acknowledge their efforts. Positive reinforcement can go a long way toward maintaining this type of behavior. Also, assure them they can voice their concerns if they have any. An open line of communication is pivotal in addressing any possible issues or misunderstandings.
Lastly, provide them with comprehensive explanations about their treatment plan. Remember, they want to fully participate in their healthcare management, and understanding what’s going is essential.
The Non-compliant Patient
On the flip side, we have non-compliant patients. This group can present a real challenge. They miss appointments, don’t adhere to their treatment plan, and often ignore medical advice. Moreover, their non-compliant behavior can sometimes lead to complications in their conditions.
However, with patience and understanding, these hurdles can be overcome. Start by explaining the consequences of non-compliance clearly and firmly. Lay out the potential risks and complications they might face if they don’t follow the treatment plan.
Moreover, it’s essential to establish a trusting relationship. Show them you’re on their side and you’re working together for their well-being. It also helps to determine the cause of their non-compliance; maybe a fear or misconception needs to be addressed.
The Anxious Patient
We’ve all felt anxiety at some point, especially regarding health problems. However, some patients experience it more severely, becoming nervous, restless, and even scared. Dealing with them demands lots of patience and reassurance.
Firstly, you need to validate their fears and show empathy. Remember, their fear is real, and dismissing it will only increase their anxiety level. Reassure them about the procedure, explaining it in simple, clear terms, maybe even demonstrating it if possible.
Secondly, encourage them to talk about their feelings. Sometimes, just voicing their concerns can alleviate a lot of their anxiety. Finally, remain calm yourself. Your calm demeanor can influence them, helping them to relax in the process.
The Demanding Patient
Demanding patients can be tough. They want answers now and solutions quicker. They’re often the ones who ask endless questions, demand more tests, and want immediate improvements. Managing them requires strong communication and interpersonal skills.
Set realistic expectations right from the start. Explain the treatment plan, timeline, and what they can expect. Don’t promise quick fixes if they’re not possible. It’s also crucial to maintain patience and a professional demeanor with them.
Remember, it’s never personal. Most of the time, they’re just fearful or insecure about their health, so being compassionate can help manage their demands and keep you sane!
The Demanding and Occasionally Angry Patient
Demanding patients, including the occasionally angry ones, can be challenging. They want immediate answers and quicker solutions. They often inundate you with endless questions, demand more tests, expect instant improvements, and show their anger when their expectations are unmet.
Managing such patients requires strong communication skills and patience. Whether their demands stem from fear, anxiety, or anger, it’s important to tread carefully. Start by setting realistic expectations, explaining the treatment process and timeline, and ensuring they understand that quick fixes might not be possible.
With angry patients, listen to their complaints without interrupting and acknowledge their feelings. Always speak respectfully and calmly, helping diffuse the situation. Your demeanor can profoundly impact the way they respond. The key is to remain patient in the face of their anger, taking it in stride and understanding that it is often a natural response to fear or frustration.
Never take their outbursts personally. Most of the time, they’re just fearful, insecure, or frustrated about their health or the treatment process, so showing compassion can help manage their demands and anger, keeping your professional relationship intact.
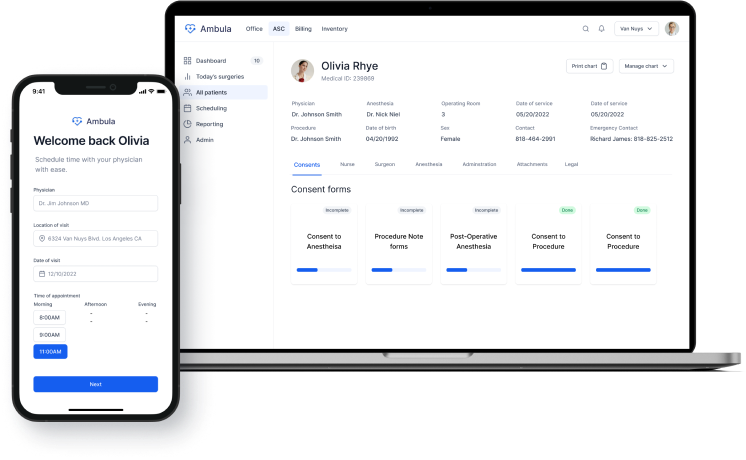
Improve patient engagement with Ambula
Create a rememberable patient experience and more patients through your practice.
The Call-light Happy Patient
Then there are the ‘call-light happy’ ones. They ring the nurse’s call bell for everything and anything. Sure, it can be frustrating. Nevertheless, understanding their condition and utilizing some practical strategies can make things easier.
Firstly, assess the reasoning behind their frequent calls. Are they bored? Or in distress? Often, they need assurance of your ongoing attention and care.
Regular check-ins could be a good solution and keep them from constantly reaching for the call light. Also, ensuring they have everything they need, including some leisure activities, can help reduce call light usage.
Types of Patients in ICU
In the ICU, patient types can vary significantly. These patients often require more intensive care and monitoring due to the severity of their conditions. Understanding the unique needs and challenges of ICU patients is crucial for providing effective care.
Importance of Communication
It’s undeniable that regardless of the type of patient, effective communication is one of the most crucial aspects of healthcare. Clearly defining treatment expectations and explaining medical matters in a language they understand can prevent miscommunication and promote adherence to treatment plans.
This is where Effective Patient Education steps in. It’s more than just giving information; it’s about making sure patients understand their condition, the importance of the treatment plan, and their role in managing their health. Remember, the goal is to empower them to make informed decisions about their healthcare.
Methods like using simple language, visual aids, written instructions, or even demonstrating procedures can make a considerable difference. Be sure to ascertain their understanding by asking them to repeat information back to you or ask any questions they may have.
The Role of Personalization
Every patient is different, and personalizing care is key to a successful provider-patient relationship. Knowing a patient’s personality type and tailoring your communication style and approach to their unique needs will create a positive impact.
From compliance-focused patients to anxious ones, a personalized approach can make all the difference in patient satisfaction .
Maintaining Professional Boundaries
Lastly, while it’s crucial to empathize and understand patients, maintaining professional boundaries is equally important. Remember, you’re their healthcare provider, not their confidante.
Balancing compassion with professionalism protects you and your patients, ensuring the best quality of care .
Tailoring Communication and Care
The most effective way to to deal with different types of patients is to tailor one’s approach to their individual needs. This means:
- Using language that is easy for the patient to understand
- Avoiding medical jargon
- Being respectful of the patient’s cultural background and beliefs
- Involving the patient in decision-making
- Providing clear and concise information about the patient’s condition and treatment plan
- Answering the patient’s questions in a patient and understanding manner
- Addressing the patient’s concerns
- Showing empathy and compassion
Healthcare isn’t a one-size-fits-all kind of job. Dealing with different personalities may be demanding, indeed. However, these challenges can be successfully navigated with understanding, empathy, effective communication, and the right strategies. This provides an invaluable part of healthcare provision – creating a positive patient experience on their recovery journey.

Keep up to date with the latest in healthcare and technology!
Subscribe to Ambula’s weekly newsletter – don’t get left behind!
Related Posts

10 Patient Medication Rights

3 ways you can identify a patient

Why Is Patient Identification Important?

Communication Strategies For Angry Patients
Elevate your practice to the next level.
Let us show you how to save 2 hours a day.
Join the modern digital health era with Ambula
Medical office software
Clinic management software
Privacy Policy
© 2024 • Ambula Health • EMR Software
Call Us (818) 308-4108
Checkout Our EMR Software Deals!
Join Our Weekly Newsletter
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMC Health Serv Res

Differences in healthcare visit frequency and type one year prior to stroke among young versus middle-aged adults
Brandi l. vollmer.
1 Department of Neurology, Vagelos College of Physicians and Surgeons, Columbia University, New York City, NY USA
2 Department of Epidemiology, Mailman School of Public Health, Columbia University, New York, NY USA
3 Department of Biostatistics, Mailman School of Public Health, Columbia University, New York, NY USA
Erin R. Kulick
4 Department of Epidemiology and Biostatistics, Temple University College of Public Health, Temple University, Philadelphia, PA USA
Mitchell S. V. Elkind
5 Division of Neurology Clinical Outcomes Research and Population Sciences, Columbia University, 710 West 168th Street, Room 642, New York, NY 10032 USA
Amelia K. Boehme
Associated data.
The datasets generated and analyzed during the current study are available in the MarketScan Commercial Claims and Encounters database.
The incidence and prevalence of stroke among the young are increasing in the US. Data on healthcare utilization prior to stroke is limited. We hypothesized those < 45 years were less likely than those 45–65 years old to utilize healthcare in the 1 year prior to stroke.
Patients 18–65 years old who had a stroke between 2008 and 2013 in MarketScan Commercial Claims and Encounters Databases were included. We used descriptive statistics and logistic regression to examine healthcare utilization and risk factors between age groups 18–44 and 45–65 years. Healthcare utilization was categorized by visit type (no visits, inpatient visits only, emergency department visits only, outpatient patient visits only, or a combination of inpatient, outpatient or emergency department visits) during the year prior to stroke hospitalization.
Of those 18–44 years old, 14.1% had no visits in the year prior to stroke compared to 11.2% of individuals aged 45–65 [OR = 1.30 (95% CI 1.25,1.35)]. Patients 18–44 years old had higher odds of having preventive care procedures associated with an outpatient visit and lower odds of having cardiovascular procedures compared to patients aged 45–65 years. Of stroke patients aged 18–45 and 45–65 years, 16.8 and 13.2% respectively had no known risk for stroke.
Conclusions
Patients aged 45–65 were less commonly seeking preventive care and appeared to be seeking care to manage existing conditions more than patients aged 18–44 years. However, as greater than 10% of both age groups had no prior risk, further exploration of potential risk factors is needed.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-021-06064-5.
With 795,000 strokes occurring in the US annually, stroke is currently the leading cause for long-term adult disability and ranked fifth in cause of death [ 1 – 5 ]. Although mortality has decreased over time, high stroke-associated morbidity continues to be a significant burden with approximately $17.5 billion per year for direct stroke costs [ 4 , 5 ]. Importantly, the incidence and prevalence of stroke among the young (18 to 44 years old) is increasing in the US, with approximately 10–14% of ischemic strokes occurring in this age group [ 6 ]. Evidence suggests this increase is not due to improved imaging techniques, but coincides with increasing traditional risk factors among those hospitalized [ 7 ].
Reducing the burden of stroke in the young population requires identification of modifiable risk factors. However, among all age groups conventional risk factors only account for 80% of risk associated with incident events, leaving a substantial proportion of risk unexplained [ 8 ]. Moreover, risk factors in the young differ from those in older populations. Previously identified stroke in the young risk factors include hypercoagulable state, nephrotic syndrome, renal disease, migraine, valvular heart disease, congenital heart disease and patent foramen ovale. Recent research has also recognized infections as a novel risk factor for stroke, particularly in young adults [ 9 – 13 ]. Vascular inflammation in response to an infection may promote coagulation, which then may increase risk of stroke, and as aging contributes to a decline in immune function, this potential mechanism of stroke may be more common in younger individuals [ 14 , 15 ]. Additionally, younger populations with high psychosocial burden or history of physical trauma or cancer events have an increased risk of stroke [ 16 – 18 ].
However, despite emerging evidence for novel risk factors, there are limited studies examining management of these conditions. Further, prior health statistics have shown, in the general population, that those aged 18–44 to have lower healthcare utilization compared to those aged 45–64 [ 19 ]. However, stroke patients are distinct from the general population due to a difference in disease burden, and disease burden plausibly influences the likelihood of utilizing healthcare systems. To date, no study has investigated healthcare system utilization prior to a stroke event, particularly in younger patients. Understanding healthcare system utilization and risk factors in this population may allow for better prevention strategies and knowledge of areas in need of further research. Therefore, through a retrospective cohort study design, we addressed this gap in knowledge though assessment of care-seeking patterns 1 year prior to stroke in young (18–44 years) compared to middle aged (45–65 years) populations. We hypothesized that a higher proportion of patients aged 18–44 with stroke had no healthcare visit in the 1 year prior to stroke than those 45–65 years. We assessed this hypothesis through examination of preceding visit types, if any, during the 1 year prior to stroke hospitalization, procedures associated with these visits, and history of risk factors at the time of stroke hospitalization, which may influence healthcare utilization.
Data source and study patients
We obtained patient data for our study from the MarketScan Commercial Claims and Encounters database, an administrative dataset containing longitudinal data for approximately 230 million de-identified patients. MarketScan contains data from patients enrolled in employee-sponsored insurance programs. Data is collected, de-identified and standardized, and includes demographic characteristics as well as International Classification of Diseases, 9th Revision (ICD-9) diagnosis and procedure codes for all inpatient, outpatient, and emergency department (ED) visits. Each patient is given a de-identified patient code to allow for linking of data and tracking over time. For this study, patients who had a stroke between 2008 and 2014 while enrolled in MarketScan and those age 65 or younger were included for analysis. Our study was limited to the period between 2008 and 2014 because of licensing and cost constraints related to obtaining access to MarketScan data at our institution. We categorized patients by their age at first stroke, 18–44 and 45–65 years. This study was approved by the institutional review board at Columbia University Medical Center; the need for review was waived as data used were publicly available and did not contain direct personal identifiers.
Outcome measures
We selected patients with ischemic strokes and intracerebral hemorrhagic strokes defined using ICD-9 codes 433.× 1 (where “x” can vary by specify arterial distribution), 434.00, 434 (excluding 434.× 0 with exception of 434.00), 436 and 431. Subarachnoid hemorrhagic strokes were excluded from this analysis as they are largely dependent on experiencing trauma or aneurysm, rather than risk factors examined in our study [ 20 ].
Exposure measures
Additional Table 1 presents ICD-9 codes used for identification of healthcare utilization types and risk factors. Age groups were defined as 18–44 years and 45–65 years at time of stroke. We categorized individuals by preceding visit types during the 1 year prior to stroke hospitalization; no prior visits, ED visits only, inpatient visits only, outpatient patient visits only, and a combination of inpatient, outpatient or emergency department visits. Due to small sample sizes, detailed descriptions of patients with inpatient visits only (0.1% of total patients included in our study) and ED visits only (1.3% of total patients included in our study) are not presented. Additionally, we categorized outpatient visits based on associated MarketScan procedure group codes of interest including preventive care, vaccination, cardiovascular, neurology, chiropractic, or emergent office visit to calculate percentage of patients with at least one prior visit for these categories in the year preceding stroke. MarketScan procedure group codes are groups of related outpatient procedures, based on Current Procedural Terminology, 4th Edition, ICD-9-CM, or HCPCS procedure codes [ 21 ]. MarketScan procedure group codes for preventative care includes physical exams, counseling/guidance/risk factor reduction, and ordering of laboratory/diagnostic procedures. All immunizations were classified as vaccinations and not as preventive care. Cardiovascular procedures included, but are not limited to, EKGs and echocardiograms. Procedure group codes used for categorization of outpatient visits are presented in Additional Table 1 . For categorization of risk groups, we collected medical history at the time of stroke hospitalization using ICD-9 codes. Risk groups were categorized as 1) metabolic causes; 2) infections; 3) stroke in the young (SITY) risk factors; 4) substance use history; 5) vascular disease history; 6) trauma and/or cancer. Additional Table 2 includes detailed definitions of risk groups.
Statistical analysis
For each age group, we examined the proportions as n (%) who met criteria for each visit type, including those with ED visits only, inpatient visits only, outpatient visits, only, or had some combination of inpatient, outpatient and/or ED visits in the year prior to stroke. Additionally, we examined distributions of demographic characteristics, medical history assessed at time of stroke, and risk groups as mean [standard deviation (SD)] for continuous variables and proportions as n (%) for categorical variables by visit types prior to stroke (no visits, outpatient visits only, combination of visits). For total number of visits prior to stroke and days from last visit, we also examined median [interquartile range (IQR)]. We calculated odds ratios (ORs) and 95% confidence intervals (95% CIs) using logistic regression comparing those aged 18–44 years to those aged 45–65 years for odds of having no visit in the year prior to stroke and odds of meeting criteria for each risk group. Additionally, for those with outpatient visits only and those with a combination of visits, odds ratios (ORs) and 95% confidence intervals (95% CIs) were calculated comparing those aged 18–44 years to those aged 45–65 years to assess odds of having select procedure codes.
We identified a total of 169,358 patients with incident stroke for inclusion in this study, consisting of 24,103 patients between ages 18–44 and 145,255 ages 45–65 years. Of those 18–44 years of age, 14.1% had no visits in the year prior to stroke compared to 11.2% of individuals aged 45–65. Those aged 18–44 had 1.30 times the odds of having no visit in the year prior to stroke compared to 45–65 (95% CI 1.25,1.35) year-olds. Of those 18–44 years of age, 516 (2.1%) had only ED visits, 28 (0.1%) had only inpatient visits, 10,812 (44.9%) had only outpatient visits, and 9356 (38.8%) had some combination of inpatient, outpatient and/or ED visits in the year prior to stroke. Of those 45–65 years of age, 1649 (1.1%) had only ED visits, 113 (0.1%) only had inpatient visits, 76,226 (52.5%) only had outpatient visits and 50,969 (35.1%) had a combination of inpatient, outpatient and ED visits in the year prior to stroke.
For those 18–44 years of age, 36.9% of those with no visits, 53.3% of those with outpatient visits only and 59.1% of those with a combination of visits were female (Table (Table1). 1 ). For those 45–65 years of age, 33.3% of those with no visits, 42.6% of those with outpatient visits only and 47.5% of those with a combination of visits were female. For both age groups, those with a combination of visit types had the largest number of total visits and the shortest time since last visit prior to stroke. For those 18–44 years of age, the median time from last visit for those with at least one visit in the year prior to stroke was 6 (IQR: 1–35) days. The median time from last visit to stroke in those 18–44 years was 13 (IQR: 2–65) days for those with only outpatient visits and 3 (IQR: 1–14) days for a combination of visits. For those 45–65 years of age, the median time from last visit for those with at least one visit in the year prior to stroke was 6 (IQR: 2–27) days, 10 (IQR: 2–45) days for those with only outpatient visits and 4 (IQR: 1–12) days for a combination of visits.
Demographics and prior history assessed at time of stroke by age group and visit type
a including inpatient, outpatient and/or emergency department
b Collected at time of stroke
Compared to those aged 45–65 years, those aged 18–44 years with outpatient visits only had increased odds of having a preventive care [OR = 1.36 (95% CI: 1.30, 1.43)], chiropractic [OR = 1.28 (95% CI: 1.19, 1.38)] or emergent office [OR = 1.96 (95% CI: 1.71, 2.25)] procedure code associated with a visit and decreased odds of having a vaccination [OR = 0.61 (95% CI: 0.57, 0.65)], cardiovascular [OR = 0.40 (95% CI: 0.38, 0.42)] or neurologic [OR = 0.85 (95% CI: 0.77, 0.92)] procedure (Table (Table2). 2 ). Results were similar when examining procedures among those with a combination of visits, with the exception of neurologic procedures. For those with a combination of visits, those aged 18–44 were more likely to have a neurologic [OR = 1.08 (95% CI: 1.02, 1.15)] procedure compared to those aged 45–55 years.
Visit type by age and visit group
Note: As procedure codes are associated with inpatient, outpatient or emergency department visits, those with no visits prior to stroke had no procedure codes for analysis
b Ages 18–44 years compared to ages 45–65 years
When compared to 45–65 year-olds, those 18–44 years of age had higher odds of having SITY risk factors [OR = 1.85 (95% CI: 1.79, 1.90)], trauma or cancer [OR = 1.15 (95% CI: 1.09, 1.21)], or no known risk factors [OR = 1.33 (95% CI: 1.28, 1.38)] at the time of stroke. Those 18–44 years of age had lower odds of having metabolic syndrome [OR = 0.34 (95% CI: 0.33, 0.34)] or substance use [OR = 0.79 (95% CI: 0.76, 0.82)] compared to those 45–65 years old (Table 3 ). Odds of having infections or ischemic disease were similar between the age groups. When examining the percentage of patients who met risk group criteria by age group and visit type, those with no visits prior to stroke had the highest percentage who met the criteria for multiple risk groups for both those 18–44 years of age (47.0%) and those 45–65 year of age (55.2%) (Fig. (Fig.1 1 and Table 4 ).
Risk groups for stroke by age
SITY Stroke in the young
a Ages 18–44 years compared to ages 45–65 years

The percentages of patients who meet the criteria for each risk group by the number of risk groups for which they qualify in those a) 18–44 years old, and b) 45–65 years old
Risk groups by age and visit group
Our retrospective cohort study using MarketScan data demonstrates commercially insured individuals aged 18–44 years had greater odds of having no inpatient, outpatient or ED visit 1 year prior to stroke compared to those aged 45–65 years. Of those with outpatient or a combination of visits, younger patients had increased odds of having a preventative care visit, but lower odds of having a vaccination compared to older patients. Of all patients who had a visit, half had a visit within 6 days prior to stroke. Importantly, 16.8% of stroke patients aged 18–44 and 13.2% of those 45–65 years had no known risk factor for stroke.
Health statistics have previously shown those aged 18–44 have lower healthcare utilization, with 21.9% not having had contact with their physician within the past year compared to 13.6% of those aged 45–64 [ 19 ]. Similarly, the number of outpatient visits per 100 person-years in the general population increases with age group [ 22 ]. Therefore, although statistically significant, it may be surprising that we did not see a larger numerical difference between the percentage of young and older age groups with no visits prior to stroke (14.1% vs 11.2%). Consistent with previously described trends, there also appears to be an increase in median number of visits for the older age group for those with outpatient visits only (4 vs 7) or a combination of visits (13 vs 18). These smaller differences seen in healthcare utilization may be due to differences in study populations, as this study investigates a privately insured population who might be more likely to seek regular care. Additionally, those who have experienced a stroke may have greater morbidity and risk factors than the general population, particularly among younger age groups, hence increasing the likelihood of seeking care. However, cost of healthcare, type of insurance coverage, and length of insurance coverage may also play a role [ 23 ]. Further, prior experience could influence the degree to which someone attends preventative clinic visits, as people want to have a caring provider who they feel comfortable enough with to express their concerns [ 24 ].
In both age groups of our study, a nominally greater proportion of females had outpatient visits or a combination of visits than no visits at all (Table (Table1). 1 ). This is supportive of previous literature demonstrating greater healthcare utilization among females [ 19 , 22 ]. Interestingly, our younger age group of those who experienced stroke consisted of more females than males (53.3% vs 46.7%). While this was not expected, as men have been shown to have increased incidence rates of stroke compared to women, particularly in younger ages [ 25 ], our study did not investigate incidence rates. This difference in proportions may be due to characteristics of the population enrolled in MarketScan.
When examining procedure codes associated with an outpatient visit, those aged 18–44 years had increased odds of seeking preventive care procedures than those 45–65 years. While this may not be expected based on prior research indicating decreased healthcare utilization in younger age groups, this is likely driven by differences in comorbidities [ 22 ]. Instead of seeking preventive care, those aged 45–65 are likely seeking care to manage current conditions. This is demonstrated by increased metabolic syndrome in those 45–65 compared to 18–44 years and additionally increased cardiovascular visits in the year prior to stroke.
However, there was decreased utilization of vaccines among younger populations. While these age differences support existing literature, the percentage of patients who had a vaccine within the year prior to stroke is concerning when considering the need for an annual flu vaccine. Our study captures all types of vaccinations administered at an inpatient, outpatient or emergency department visit, including, but not limited to, the flu vaccine. However, vaccine utilization for all immunizations in our study, ranging from 11.3 to 21.5% depending on age group and visit type, are well below annual estimates of flu vaccine utilization from the CDC. For the 2018–2019 flu year, the CDC estimated a vaccination coverage of 34.9% of 18–49 year olds and 47.3% of 50–64 year olds [ 26 ]. This may in part be due to individuals receiving flu vaccinations from sources that were not captured within the MarketScan dataset, such as through a pharmacy or work program. However, a previous meta-analysis found those vaccinated against the flu had a decreased risk of developing stroke [ 27 ], thus lower vaccination rates among our study population may be expected. As it is currently unclear if vaccination is a marker for health care utilization, resulting in a reduction in stroke risk due to management of risk factors rather than the influenza vaccination itself, future studies should thoroughly examine differences in vaccination rates among those who do and do not utilize healthcare among at risk populations.
When evaluating risk groups for both age groups, results indicate those with no visits 1 year prior had the highest proportions of patients with prior risk for stroke. A higher percentage of patients with no visits prior to stroke had prior history of hypertension, alcohol abuse, drug abuse/dependence, and smoking than all other visit groups for both age groups. Likely, despite having private insurance, these patients are not reached by current clinical interventions to reduce or manage risk factors, illustrating the need for population-based prevention methods.
Not surprisingly, the greatest proportions of stroke patients for each visit type were included in multiple risk groups. Modifiable or manageable risk factors, particularly hypertension, were common suggesting a large portion of strokes may have been preventable. However, it is concerning that 16.8 and 13.2% of those aged 18–44 and 45–65 had no prior risk as seen in Table Table4. 4 . This could in part be due to limited detection of risk factors as diagnostic tools are continuously being developed, [ 28 ] Further, under reporting in this administrative dataset may occur, particularly for conditions that do not contribute to reimbursement, as for example, low prevalence of obesity was observed for both age groups (ranging from 2.7 to 3.7%). However, additional research is likely needed to identify novel risk factors, further informing stroke mechanism and areas for prevention in the younger population, as modifiable risk factors including hypertension, smoking and alcohol abuse were less common in those aged 18–44 years.
This study has some limitations. Medical history and risk factors may not be readily captured in MarketScan as it is an administrative database, thus prevalence estimates may be underestimated in our study. Additionally, assessed ICD-9 procedure codes are associated with outpatient visits. As patients may seek care through additional sources, such as through work programs or a pharmacy, our results likely underestimate procedure, particularly vaccination coverage. Finally, MarketScan is a dataset of insurance claims and does not capture un-insured individuals or individuals with insurances that do not participate in MarketScan. However, as this is a descriptive study including a large sample size representative of a national population, we believe our study can inform additional questions pertaining to healthcare utilization and risk factor prevalence among young stroke patients.
In conclusion, no prior study had investigated healthcare system utilization prior to a stroke event, particularly in younger patients, though understanding healthcare utilization in this population can inform prevention strategies, such as risk factor management. Our retrospective cohort study including a commercially insured sample aimed to address this gap and found those aged 18–44 years had increased odds of having no inpatient, outpatient or ED visits 1 year prior to stroke compared to those aged 45–65 years. Those with no prior visits accounted for 14.1 and 11.2% of 18–44 and 45–65 year-olds, respectively. This difference between age groups is smaller in our study than the general population, highlighting how our population is distinct. While older patients aged 45–65 years were less commonly seeking preventive care, they had a higher median number of visits and appeared to be seeking care to manage existing conditions more so than patients aged 18–44 years. As vaccine utilization for all immunizations in our study were low, future studies should closely examine differences in vaccination rates among those who do and do not utilize healthcare among at risk populations to determine the relationship between vaccination and stroke risk. Additionally, our study describes the need for population-based interventions to lower modifiable risk factors as a higher percentage of patients with no visits prior to stroke had prior history of hypertension, alcohol abuse, drug abuse/dependence, and smoking for both age groups. However, as greater than 10% of those aged 18–44 and 45–65 years had no known prior risk, further exploration of novel risk factors is needed.
Acknowledgements
We would like to acknowledge the Columbia University CTSA for thei help in obtaining the MarketScan data.
Abbreviations
Authors’ contributions.
BLV analyzed data, interpreted data, and was a major contributor in writing the manuscript. XC contributed to the design of work, analyzed data, and interpreted data. ERK made substantial contributions to the conception, interpretation and substantively revised the manuscript. MSVE made substantial contributions to the conception and substantively revised manuscript. AB made substantial contributions to the concept and design, aided in acquisition and interpretation of data, and substantively revised the manuscript. All authors read and approved the final manuscript.
This project was funded through internal funding via the Calderone Pilot Award, Columbia University, Mailman School of Public Health. The funding body was not involved in the design of the study, nor in the collection of data, the analysis, the interpretation or the writing of the manuscript.
Availability of data and materials
Ethics approval and consent to participate.
This study was approved by the institutional review board at Columbia University Medical Center; the need for review was waived as data used were publicly available and did not contain direct personal identifiers. Informed consent was waived as this analysis was on secondary, deidentified data. Administrative permissions were not necessary to access the data as the data was deidentified.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have influenced the work reported in this paper.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.

- Our Philosophy
- Why Independent Primary Care
- Samuel Warren, MD
- Rachel Beda, MD
- Nazlee Navabi, MD
- Janna Cuneo, ARNP
- David Roesel, MD
- Our Clinical Staff
- Read Our Newsletters
- Membership Benefits
- For Medicare Patients
- How To Register
- Testimonials and Reviews
- FOR EMPLOYERS
- Conditions We Treat
- SCHEDULE NOW
Types of Appointments
Office visit, wellness physical, pre-travel consultation, blood draw/vaccinations.
Office visits, otherwise known as focused visits, are best suited for 1-3 topics you want to discuss. Depending on the complexity of the concerns, all three topics can be taken care in one visit. However, sometimes to ensure the highest quality of care we request you come back for a follow-up visit to ensure there is enough time to address your needs.
This is the most common appointment type and is divided into levels 1 through 5 (each with its own Current Procedural Terminology (CPT) code) based on counseling time, medical risk, and decision-making criteria that are very complex. Most clinics use professional coders and/or software to help generate CPT codes for an office visit, which defends the clinic against any claim that it applies charges to different types of patients differently. Believe it or not, “down-coding” an appointment in order to charge a patient less than the calculated office visit level is penalized the same as “up-coding” in order to charge a patient more than the calculated office visit level! The legal word that describes this is “malfeasance” by unfairly favoring some patients over others. Most office visits trigger the CPT code for one of levels 3 through 5, since level 1 can’t even involve the doc and level 2 gets surpassed readily in visits of any substance.
During this visit type, we review your past medical history, family medical history, health habits, current medications, and allergies. We perform a screening physical exam. We synthesize the information into a personalized assessment of disease risk. We recommend for or against additional screening tests to screen for common cancers, and screening tests to help clarify your risk status for heart attack or stroke. We discuss the impact that lifestyle can have on your particular health future.
What is not included in a preventative screening physical? By CPT coding rules, the preventative screening physical cannot include “active management” of a medical problem or symptom unless a separate “office visit” is also coded alongside the screening physical – which will transform the appointment type into a combined visit (described below). Medication refills and dose changes can be included in the preventative screening physical, but new medications, treatment strategies, and referrals (other than screening referrals) trigger CPT codes for “office visit”.
These distinctions are important because some insurance companies waive all out-of-pocket costs for one preventative screening physical appointment per year (i.e., no copay,no co-insurance, no deductible payment). Be sure to ask your insurer if they are one such company. When you schedule a preventative screening physical – with Wise Patient or any other clinic – you should emphasize to the clinic that you are scheduling a preventative screening physical. That way we can do our part to insure the contents of the visit do not include things that would trigger an “office visit” code to be generated and billed out.
Some insurance companies do not cover travel-related appointments. In light of this shortfall, we offer a $50 self pay appointment with one of our medical assistants (no face-to-face time with the MD) who will go over the recommendations for your particular itinerary and have any prescriptions approved by one of our physicians. A physician will review the medical assistant’s recommendations and confirm they are indicated, but will not see you directly. We feel our $50 self pay price is competitive with many of the local pharmacy prices that we have seen.
If your insurance plan does cover pre-travel visits we are happy to send the claim to your insurance company at your request, just let us know!
Our Health Coaches are all certified phlebotomist. If blood work is indicated at your appointment we draw your blood right then and there. However, some tests require you be fasting so we allow patients to book blood-draw only appointments every morning at 8am. We do not offer blood draw appointments for patients who have not seen one of our physicians prior.
Please be aware that any blood tests we think are in your best interest will be sent off to an external facility (Lab Corp or Quest Diagnostics) for the test and the lab will bill your insurance accordingly. We have no control over the prices of those labs as the amount it will cost you depends on your insurance plan.
If you are a Direct Primary Care subscription patient, we offer self pay prices at a fraction of the cost that most insurance companies will charge you.
Vaccinations
We supply the influenza vaccine during the recommended time to get vaccinated (September-April). In addition, we supply the TDAP vaccine (Tetanus, Diphtheria, and Pertussis) and are happy to administer it when indicated. As a small clinic, we do not have the necessary volume to stock any other vaccines and therefore any vaccines you may need can be sent to you local pharmacy for administration.
Preventative Screening Physical CPT codes
Curious about how much your insurance company will cover? Call your insurance company and reference the following CPT codes to find out.
Office Visit CPT codes

IMAGES
VIDEO
COMMENTS
Starting in 2016, patients scheduling a primary care appointment through the patient portal must choose their visit type: office, video, or telephone visit (except for visits designated as a routine physical examination, which were offered only as office visits). Available clinicians included patients' own personal primary care clinician ...
9) Telemedicine Visits. Each visit is given a different time allotment at the time you call to schedule your appointment, and this time slot cannot be changed after you arrive in the office. It is very rare that we are able to combine visit types and thus it should not be expected. So if your concerns overlap appointment types, you will most ...
Visit Descriptions. Establish Care (New Patient): This type of appointment is for your first visit with your new health care provider after switching your health care to our practice. It is designed to include a thorough review of your past medical history. It may include blood work or other testing, if indicated.
Benefits and drawbacks of using telehealth were reported across different visit types from patient and clinician perspectives, as well as the circumstances in which telehealth was found to be suitable (or not) for each primary care visit type. As telehealth potentially becomes a long-term care delivery model, improving telehealth consultation ...
Medicare has rules for each type of visit. Ask a social worker or care manager any questions you have about Medicare. For inpatient visits: ... Patient Finance Customer Service Representatives are available to speak with you Monday-Friday from 8:00 am - 4:00 pm. Please call 212-263-1481and leave a message.
Types of telehealth services. Audio-video: A video visit is a real-time (synchronous) audio/visual interaction between the physician and the patient. A video visit can be used in place of an in ...
J Allied Health. 2001;30 (3):146-152. Download PDF: Provider Type and Management of Common Visits in Primary Care. In primary care, nurse practitioners and physician assistants do not necessarily ...
The number of primary care visits decreased from 336 million to 299 million per year. Per capita visit rates declined from 1.5 visits per person in 2008 to 1.2 visits per person in 2015: a 20% decline over the study period (−0.25 visits per person, 95% CI, -0.32 to -0.19) ( Table 1 ).
Background. Because the impact of changes in how outpatient care was delivered during the COVID‐19 pandemic is uncertain, we designed this study to examine the frequency and type of outpatient visits between March 1, 2019 to February 29, 2020 (prepandemic) and from March 1, 2020 to February 28, 2021 (pandemic) and specifically compared outcomes after virtual versus in‐person outpatient ...
We acquired patient and visit-level clinical data, including patient comorbidities, the primary encounter diagnosis (using codes from the International Classification of Diseases, Tenth Revision (ICD-10)), whether the visit was with a patient's personal primary care provider (PCP) or a different clinician, the visit type (video or telephone), KPNC medical center through which the visit occurred.
Conduct pre-visit planning two to three days prior to the patient visit: Review notes from the previous visit. The designated team member ensures that follow-up results are available for physician review. Use a registry or visit-prep checklist. The checklist helps to identify any care gaps or upcoming preventive and chronic care needs.
OPS 326.1. DESCRIPTION: This policy describes Clinica's protocol relating to oversight, timeliness and management of appointment setting as well as definitions of appointment types and appointment length. PURPOSE: The purpose of this policy is to clarify and identify the guidelines and protocol for patient appointment setting so to ensure ...
The time constraints of office visits are a concern shared by physicians and patients. Wait time and visit length can certainly affect patient satisfaction, but one study showed that what mattered ...
• Re-Schedule - Patient who requests to re-schedule the appointment with at least 24-hour notice of the appointment. • Late: Patient is considered late if he/she arriver more than 7 minutes after scheduled appointment time. • Cancellation - Patient who calls to cancel the appointment with at least 24 hours'
Effective documentation is crucial for providing quality healthcare, streamlining communication among healthcare teams, and ensuring patient safety. Section 1: Routine Check-Ups And Progress Visits. Routine check-ups and progress visits are crucial to monitoring preventive care and ongoing treatment. During routine check-ups, healthcare ...
Key Takeaways. There are various types of primary care doctors, including internal medicine doctors, family medicine doctors and pediatricians. Primary care physicians can generally take care of a ...
Learn how to apply the guidelines to some common visit types. Advertisement. ... Established patient visit New patient visit; Level 2: 99212 10-19 minutes: 99202 15-29 minutes:
There are three types of wellness visits, each of which has different requirements. To know if you are being compliant with requirements and coding correctly, know what each entails: 1. Initial Preventive Physical Examination (IPPE) or the "welcome to Medicare preventive visit" - use code G0402 Initial preventive physical examination ...
View Visit Code and Type of Admission/Visit. 1 = Emergency. 2 = Urgent. 3 = Elective. 4 = Newborn. 5 = Trauma Center. 9 = Information Not Available. Last Updated Jan 17 , 2023. View the type of admission or visit codes which depict where the patient was prior to inpatient admission.
Firstly, you need to validate their fears and show empathy. Remember, their fear is real, and dismissing it will only increase their anxiety level. Reassure them about the procedure, explaining it in simple, clear terms, maybe even demonstrating it if possible. Secondly, encourage them to talk about their feelings.
Age groups were defined as 18-44 years and 45-65 years at time of stroke. We categorized individuals by preceding visit types during the 1 year prior to stroke hospitalization; no prior visits, ED visits only, inpatient visits only, outpatient patient visits only, and a combination of inpatient, outpatient or emergency department visits.
This is the most common appointment type and is divided into levels 1 through 5 (each with its own Current Procedural Terminology (CPT) code) based on counseling time, medical risk, and decision-making criteria that are very complex. Most clinics use professional coders and/or software to help generate CPT codes for an office visit, which ...
Define visits for the purposes of the UDS. Accurately report a variety of visit types, including clinic (in-person) and virtual visits. Understand the relationship between countable visits and and other tables (i.e., Table 6A) in the UDS Report. Understand what visits or services are to be reported in the Table 5 Selected Service Detail Addendum.
a. When you build your visit types and templates, build them based on multiples of the shortest visit length. b. Example: c. Make sure the visit type default length matches template interval length. i. Example: If there is a 15 minute visit type default length, then the template has to be built with 15 minute intervals. 3.