
- Cancer info and support
- Online Community
- Cost of living
- Volunteering
- Healthcare professionals
- Ask an Expert
- Cancer types forums
- Replies 8 replies
- Subscribers 249 subscribers
- Views 1593 views
- Users 0 members are here
- Breast cancer
- chemotherapy
- radiotherapy

More from this forum
Flying after Radiotherapy
- 249 subscribers
Hi folks, after a long haul of chemotherapy for Triple Negative BC, I'm about to start Radiotherapy. Looking forward to planning a holiday and I'm wondering if anyone can give advice on how soon after Radiotherapy I might feel up to flying? I know this is a 'how long is a piece of string' question but generally, have people experienced extreme tiredness to the point that they are in bed all day for weeks after etc?
- Add a reply You need to log in to reply
Everyone is different of course but I flew I think a week after radiotherapy, might of been 2, (was in 2013) but I was absolutely fine to fly, I coped very well with radiotherapy and had some tiredness but not extreme, some scabbing. You must keep the area out of the sun though, all of the time, I wore a t shirt in the pool for example, you’ll really burn otherwise x
If you are planning an overseas trip it might be a good idea to checkout travel insurance. I had been planning a trip about the same stage as you. Didn't go in the end, as still having maintenance doses of H&P every three weeks and GP advised against it due to covid and all the complications around travel. He was worried I might have a delayed return and miss a treatment. There was an issue re travel insurance if it was less than a month after treatment was completed and there were questions about whether any area exposed to RT needed dressings (which I did need). Better safe than sorry.
The radiotherapy carries on working after you finish treatment and the maximum effects are felt 10 to 14 days after completion.
Everyone is different of course with regards to tiredness and skin reaction.
You may enjoy your holiday more if you leave it a month after you finish treatment as your skin will be healing.
As Anna said you must keep the area out of the sun. Wear high factor suntan cream and a T shirt in the pool.
Hope you have a lovely time
I'm also thinking about this. In fact it's the only thing keeping me going after having 4 holidays postponed or cancelled over the past 18 months.I'm very careful in the sun anyway and tend to sit in the shade a lot.
Ive done a 'dummy insurance search' and even going through Compare the Market and stating I've got ongoing herceptin injections it still comes out affordable.
Good luck with your holiday plans, if anything this has taught me life is very short and you need to grab any opportunity (as long as it's safe and okayed by your dr)
Thanks xraygirl, much appreciated
Thanks Anna of somewhere not too sunny so should be ok
I will have a look at travel insurance, definitely want to make sure I'm covered!
Hi Jacala, yes, I agree, planning to get away is keeping me focused. I will never be so happy to get on a Ryanair flight and eat their rubbish food!
- Cancer groups
- Cancer blogs
- Ask an expert
- Cancer news
- Text:Cancer information and support> Destination:https://www.macmillan.org.uk/cancerdashinformationdashanddashsupport|_|eventCategory|-|Internal links clicks> Content menu footer|_|eventLabel|-|Source:https://www.macmillan.org.uk/errordash404|" title="Cancer information and support" data-gtm-added="true">Cancer information and support
- Text:Cost of living> Destination:https://www.macmillan.org.uk/cancerdashinformationdashanddashsupport/getdashhelp/costdashofdashliving|_|eventCategory|-|Internal links clicks> Content menu footer|_|eventLabel|-|Source:https://www.macmillan.org.uk/errordash404|" title="Cost of living" data-gtm-added="true">Cost of living
- Text:Online Community> Destination:https://community.macmillan.org.uk/|_|eventCategory|-|Internal links clicks> Content menu footer|_|eventLabel|-|Source:https://www.macmillan.org.uk/errordash404|" title="Online Community" data-gtm-added="true">Online Community
- Text:In your area> Destination:https://www.macmillan.org.uk/indashyourdasharea/choosedashlocation.html|_|eventCategory|-|Internal links clicks> Content menu footer|_|eventLabel|-|Source:https://www.macmillan.org.uk/errordash404|" title="In your area" rel="noopener noreferrer" target="_blank" data-gtm-added="true">In your area
- Text:Fundraise> Destination:https://www.macmillan.org.uk/fundraise|_|eventCategory|-|Internal links clicks> Content menu footer|_|eventLabel|-|Source:https://www.macmillan.org.uk/errordash404|" title="Fundraise" data-gtm-added="true">Fundraise
- Text:Donate> Destination:https://www.macmillan.org.uk/donate|_|eventCategory|-|Internal links clicks> Content menu footer|_|eventLabel|-|Source:https://www.macmillan.org.uk/errordash404|" title="Donate" data-gtm-added="true">Donate
- Text:Advocacy> Destination:https://www.macmillan.org.uk/advocacy|_|eventCategory|-|Internal links clicks> Content menu footer|_|eventLabel|-|Source:https://www.macmillan.org.uk/errordash404|" title="Advocacy" data-gtm-added="true">Advocacy
- Text:Volunteering> Destination:https://www.macmillan.org.uk/volunteering|_|eventCategory|-|Internal links clicks> Content menu footer|_|eventLabel|-|Source:https://www.macmillan.org.uk/errordash404|" title="Volunteering" data-gtm-added="true">Volunteering
- Text:Healthcare professionals> Destination:https://www.macmillan.org.uk/healthcaredashprofessionals|_|eventCategory|-|Internal links clicks> Content menu footer|_|eventLabel|-|Source:https://www.macmillan.org.uk/errordash404|" title="Healthcare professionals" data-gtm-added="true">Healthcare professionals
- Text:Shop> Destination:https://shop.macmillan.org.uk|_|eventCategory|-|Internal links clicks> Content menu footer|_|eventLabel|-|Source:https://www.macmillan.org.uk/errordash404|" title="Shop" rel="noopener noreferrer" target="_blank" data-gtm-added="true">Shop
- Text:About us> Destination:https://www.macmillan.org.uk/aboutdashus|_|eventCategory|-|Internal links clicks> Content menu footer|_|eventLabel|-|Source:https://www.macmillan.org.uk/errordash404|" title="About us" data-gtm-added="true">About us
- Text:Contact us> Destination:https://www.macmillan.org.uk/aboutdashus/contactdashus|_|eventCategory|-|Internal links clicks>Content menu footer|_|eventLabel|-|Source:https://www.macmillan.org.uk/errordash404|" data-variantitemid="{48A92B7C-0598-4C2F-BA59-B36795C84A66}" title="Contact us" data-variantfieldname="Link" data-gtm-added="true">Contact us
- Text:Jobs and careers> Destination:https://jobs.macmillan.org.uk/jobs/|_|eventCategory|-|Internal links clicks>Content menu footer|_|eventLabel|-|Source:https://www.macmillan.org.uk/errordash404|" data-variantitemid="{2DA0DF53-ED0B-4E24-9EE3-471C7F34C11B}" title="Jobs and careers" data-variantfieldname="Link" data-gtm-added="true">Jobs and careers
- Text:What we do> Destination:https://www.macmillan.org.uk/aboutdashus/whatdashwedashdo|_|eventCategory|-|Internal links clicks>Content menu footer|_|eventLabel|-|Source:https://www.macmillan.org.uk/errordash404|" data-variantitemid="{753BACBC-CB7C-42AD-A90C-161B4525280C}" title="What we do" data-variantfieldname="Link" data-gtm-added="true">What we do
- Text:Our organisation> Destination:https://www.macmillan.org.uk/aboutdashus/organisation|_|eventCategory|-|Internal links clicks>Content menu footer|_|eventLabel|-|Source:https://www.macmillan.org.uk/errordash404|" data-variantitemid="{8F884D8C-468D-4A89-8183-9A3841561F55}" title="Our organisation" data-variantfieldname="Link" data-gtm-added="true">Our organisation
- Text:Corporate partners> Destination:https://www.macmillan.org.uk/aboutdashus/workingdashwithdashus/corporatedashpartners|_|eventCategory|-|Internal links clicks>Content menu footer|_|eventLabel|-|Source:https://www.macmillan.org.uk/errordash404|" data-variantitemid="{CEB79931-7C7D-4E8A-8BF0-B4C9CEBADFFE}" title="Corporate partners" data-variantfieldname="Link" data-gtm-added="true">Corporate partners
- Text:Press office> Destination:https://www.macmillan.org.uk/aboutdashus/pressdashoffice|_|eventCategory|-|Internal links clicks>Content menu footer|_|eventLabel|-|Source:https://www.macmillan.org.uk/errordash404|" data-variantitemid="{7A96D5D4-DFC0-472D-A41B-44916E612BBB}" title="Press office" data-variantfieldname="Link" data-gtm-added="true">Press office
Whatever cancer throws your way, we’re right there with you.
We’re here to provide physical, financial and emotional support.
- Terms and conditions
- Privacy policy
- About our information
- Accessibility
© Macmillan Cancer Support 2024 © Macmillan Cancer Support, registered charity in England and Wales (261017), Scotland (SC039907) and the Isle of Man (604). Also operating in Northern Ireland. A company limited by guarantee, registered in England and Wales company number 2400969. Isle of Man company number 4694F. Registered office: 89 Albert Embankment, London SE1 7UQ. VAT no: 668265007
Log in to our secure, personalized website to manage your care (formerly myMDAnderson).
Request an Appointment
If you are ready to make an appointment, select a button on the right. If you have questions about MD Anderson’s appointment process, our information page may be the best place to start.
- Donate Today

- Clinical Trials
- Our Doctors
Traveling with cancer: 7 questions to ask your doctor
August 11, 2023
BY Cynthia DeMarco
Some elements of travel are the same for everyone. Clothing and toiletries, for instance, are generally a packing staple. Many people bring prescription drugs for chronic conditions , too.
But what if you have cancer? Are there any specific travel considerations you should keep in mind? We went to neuro-oncologist Ashley Aaroe, M.D. , for advice.
Here are seven questions she recommends asking your care team before a trip.
1. Is it safe for me to travel?
This is the most important question to ask because some cancer treatments can leave patients more susceptible to blood clots and infections . This is particularly true if you’re immunocompromised due to chemotherapy or just had a stem cell transplant .
“Most people can tolerate the changes in cabin pressure and oxygen levels during a flight without developing any medical issues,” notes Aaroe. “But people with certain sensitivities might feel those adjustments more acutely.”
If you have a brain tumor , for instance, you might be more prone to seizures or brain swelling. And, if you’re anemic , you might be more susceptible to dizziness or fainting.
“You also don’t know what the people around you might have going on, in terms of respiratory and gastrointestinal infections,” adds Aaroe. “Cruise ships in particular are frequently in the news for outbreaks of gastrointestinal viruses that can spread like wildfire once they’ve gained a foothold.”
2. Is there a ‘best time’ for me to travel?
If you’re receiving chemotherapy, there may be certain periods during which you’re at the highest risk of developing anemia or an infection, or times when you might be expected to have more side effects. So, if you’ve already been cleared to travel, ask your doctor what your best options are in terms of timing.
“Patients taking the oral chemotherapy drug temozolomide usually see their blood counts reach their lowest points about 21 days into each cycle,” says Aaroe. “Most won’t have any significant issues as a result. But those who do may want to weigh this in their travel plans. Patients usually also prefer not to travel during the period that they are actively receiving chemotherapy, due to nausea and fatigue. ”
3. Will I need any vaccinations?
In addition to COVID-19 , your travel destination may have its own set of exposure risks. The Zika virus, for instance, is still prevalent in many Central and South American countries. Ebola continues to circulate on the African continent. And tuberculosis remains an issue worldwide, despite global efforts to eradicate it.
Be sure you’re up to date on all your vaccinations before you leave. And ask your doctor which others you might need — and how far in advance — to give you the most protection.
“When I was about 13, my family moved to China for a few years,” recalls Aaroe. “I got so many shots before we left that I literally couldn’t move my arm for a few days. But I also didn’t get sick with any of those illnesses while we were there. Vaccinations work.”
4. What should I carry with me at all times in the event of an emergency?
It’s always a good idea to bring extra medication on a trip, just in case you should face unexpected delays or accidentally drop a pill down the sink.
But be sure to carry both fast-acting and regular medications with you. That way, you won’t ever have to miss a dose due to an extended layover. You also won’t run the risk of not having access to any of the specialized medications you need.
“Many brain tumor patients take an oral medication daily to prevent or control their seizures,” Aaroe explains. “But there are also several fast-acting therapies — such as lorazepam, intranasal sprays and even suppositories — that can stop seizures in the moment when administered. And those are substances that a standard first-aid kit may not contain.”
The most important item to bring with you is a summary of your condition and guidance on what to do if you should become incapacitated. This is especially important if you’re traveling alone, but could also come in handy in an emergency, especially if it’s difficult for your caregiver to relay your history to a flight attendant or a tour guide.
Include clear instructions in your health summary, such as:
- give me this amount of that medication if X happens, followed 15 minutes later by this much of that one
- call this person right away at a particular phone number, or
- take me to the nearest hospital immediately and show them these documents
“One of my patients had his summary translated into several other languages, including the main language spoken at his destination,” noted Aaroe. “That was a very prudent and proactive thing to do.”
Also, consider bringing:
- a doctor’s authorization confirming that you’ve been cleared to travel
- notes from your last doctor's visit
- digital images of your most recent scans on a DVD or thumb drive
“A picture is worth a thousand words,” adds Aaroe. “And MRIs are thousands of pictures. So, if you bring along copies of your latest scans and something happens, doctors will be able to compare them directly to your current scans and see if anything has changed.”
It’s also a good idea to make sure you’ve downloaded the myChart app on your mobile device before traveling – and that you remember how to log in. That way, you’ll be able to pull up any notes or medical records needed and communicate with your care team while you’re away.
5. Will I need any special documentation for my medications?
“Some medications are easier to travel with than others,” Aaroe notes. “If you’re taking opiates or methadone for cancer-related pain , for instance, you might need a doctor’s note in some countries explaining why you’re receiving those things.”
Most airports have services available to help you with these issues, especially if you call in advance. But it will probably still take you a little more time to get through security, so plan accordingly.
6. Is there anything special I should do during a flight to minimize my risk of problems?
Any time you’re sitting for a prolonged period — whether it’s in a plane, train or car — your risk of developing blood clots in your legs increases. These clots — also known as deep vein thrombosis (DVT) — can be fatal if they break loose and travel to your lungs.
So, ask your oncologist if you should wear compression hose while traveling or do anything else to reduce your risk of DVT.
“The Centers for Disease Control (CDC) recommends getting up and moving around every 2 to 3 hours while driving or flying,” Aaroe notes. “Even if you’re sitting down, there are exercises you can do to improve your circulation. You can raise and lower your heels, for instance, roll your ankles around, or tighten and release your leg muscles.”
Call your doctor immediately upon arrival if you show any symptoms of DVT. These include:
- swelling in the legs
- pain or tenderness
- difficulty breathing
- chest pain
- fast heart rate
- lightheadedness
7. Should I warn anyone about my condition or wait until something happens?
No one is obligated to divulge their medical history to anyone, but whether you alert a flight attendant or tour guide is entirely up to you. It all depends on the situation and your comfort level.
“There’s no one-size-fits-all approach,” says Aaroe. “I don’t think it’s strictly necessary to tell anyone, as long as your medical summary is handy and accessible if something happens. But ask your doctor to be sure. Travel is perfectly safe for cancer patients most of the time, and we want you to enjoy your life. But you never know exactly what might happen, so it’s good to be prepared.”
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
You never know exactly what might happen, so it’s good to be prepared.
Ashley Aaroe, M.D.
Share Your Story
Coronavirus precautions, help #endcancer, donate blood.
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
An Overview of Flying With Cancer
Air travel with cancer.
- Medications and Devices
- Getting Around
- Reducing Blood Clots
- Oxygen Needs
Air Pressure Changes
Infection concerns, cancer fatigue, travel insurance.
Flying on commercial airlines is usually very safe for people with cancer who are stable, reasonably healed from any surgeries, and do not have a very low white blood cell count or platelet level due to chemotherapy . That said, it's important for anyone with cancer to talk to an oncologist before scheduling any air travel to discuss potential concerns about oxygen levels or pressure changes during flight, or the need for preventive measures against blood clots. Here we will look at these concerns, common questions people have about medications or medical devices while flying, and general measures that can help you prepare for seamless travel.
Flying with cancer can sometimes have significant benefits. In some cases, people may need to fly to the cancer center where they will be treated. But pleasure trips are encouraged by many oncologists as a great way to cope with the rigors of treatment and to reconnect with family and/or friends outside of the clinic or hospital setting.
Many people wonder about the best time to travel during treatment, and the answer will be different for everyone.
Air travel should be avoided if at all possible for at least two weeks after surgery for a number of reasons (and much longer in some situations such as after brain surgery). In general, any incisions should be well healed and any drains removed.
With chemotherapy, the best time to fly will depend on the particular chemotherapy regimen you are on, as well as other factors such as side effects you are experiencing and more. With some protocols, the chemotherapy nadir (when blood counts are at their lowest) occurs around 10 days to 14 days after an infusion, and an oncologist may recommend travel either earlier or later for this reason. A low white blood cell count can increase infection risk, a low red blood cell count (anemia) can make you more tired, and a low platelet count (thrombocytopenia) can increase the risk of bleeding. With high dose chemotherapy, such as with some leukemias, air travel may be discouraged throughout the duration of treatment.
General Information
The Air Carrier Access Act of 1986 prohibits discrimination on domestic flights in the United States on the basis of disability. While there are some "horror stories" that spread through the news regarding transportation security administration (TSA) agents and "pat downs," TSA agents should typically be ready to assist those with disabilities due to cancer with courtesy and respect. TSA recommends calling their helpline 72 hours before travel to discuss the screening process.
- You may call TSA Cares at 1-855-787-2227 for information on what to expect at the security checkpoint.
- You may also request a passenger support specialist. These TSA specialists are trained in assisting people with disabilities of all kinds.
Medications and Medical Devices
Many people with cancer will need to travel with medications or medical devices. In addition to making sure that you have an adequate supply of medications (with at least a few extra days worth in case of delays or changes due to weather), there are several other things you should consider.
Oral Medications
Carry all medications on board in a carry-on rather than checking them with your luggage. This includes any medications you use for side effects such as anti-nausea drugs or pain medications. Keep all medications in their original containers. Though it's recommended that you bring enough medications for your entire trip plus unexpected delays, many insurance companies have a limit on the number of pills you will be prescribed at one time. If this is an issue, talk with the pharmacist responsible for prescribing your medications.
Medications that cannot go through the X-ray machine are allowed, but you will need to talk to the TSA agent and this may require a pat down.
If you have medications in liquid form, containers containing more than 3 ounces are allowed but you will need to remove the medication from your bag and mention it to the TSA agent before going through security.
Medications and Travel Outside the U.S.
Keep in mind that drug approval varies among countries and that your particular medication may not be available where you are traveling.
It's also very important to make sure that your medication is legal in the countries you are visiting.
For example, drugs containing pseudoephedrine (such as Sudafed) are illegal in Japan. Amphetamines such as Adderall are illegal in Japan and Saudi Arabia. Narcotics may be illegal or restricted, for example, codeine is illegal in Greece and Hong Kong. Some countries (such as Costa Rica) require that you have a healthcare provider's note describing the medications and only bring enough for your stay. When traveling overseas, make sure to check out the laws, as exceptions are not made, even for people with cancer.
Traveling With Syringes
If needed for a medical condition, you may carry syringes and injectable medications on board the plane. It’s advisable to carry a healthcare provider's letter indicating the necessity of carrying these medications since some checkpoints may require a healthcare provider's recommendation (on letterhead stationery).
Medical Marijuana/CBD Oil
Though marijuana is now legal in many states, it is still illegal under TSA law (and federal law) even with a healthcare provider's note, and could be risky. This is true for CBD oil as well. While the TSA does not search for marijuana, if detected they defer to local law enforcement. People with cancer should not travel with medical marijuana outside of the United States.
Chemotherapy Ports/PIC Lines/Ostomy Ports
If you have a port, ostomy, or other medical device, you will need to tell the TSA agent before going through screening. In some cases, a pat down may be required.
Head Coverings
Most of the time you will be allowed to wear a wig, scarf, or other head covering as you go through security as these are considered medical items, but may be subject to a pat down. You can request a private screening if you would like.
Breast Prostheses
Breast prostheses do not need to be removed, though you will need to tell the TSA agent before screening and rarely a pat down will be required.
Getting Around in the Airport and Boarding
Most airports provide transportation services beyond the security checkpoint. Check with the airports you will be visiting to see what services are available.
Advance Seating
Airlines usually announce advance seating for people with disabilities along with first class passengers. If you need assistance with boarding, this option may be helpful. That said, if you are able to move around it may be a good idea to instead move around and board towards the end of boarding, especially if you have a long flight. Prolonged sitting raises the risk of developing blood clots.
Reducing the Risk of Blood Clots
Air travel as well as cancer itself raise the risk of blood clots (deep vein thrombosis and pulmonary embolism) and the risk is higher when the two are combined. Cancer treatments such as surgery and chemotherapy increase the risks further . Thankfully, many of these clots can be prevented by taking a few precautionary measures:
- Get up and walk around often—at least one time per hour
- Exercise your legs while sitting. On overseas flights, it's now common for passengers to be shown a video on leg exercises which may reduce the risk of clots when performed in flight. You can exercise your legs by tightening and then releasing your calf muscles or turning your foot in a circle. You can also exercise your legs by lifting your heel repeatedly with your toes on the floor, then lifting your toes several times with your heels on the floor.
- Choose an aisle seat when possible
- Avoid drinking alcohol as it can lead to dehydration and makes platelets (the factors in the blood that cause clotting) stickier.
- Avoid crossing your legs
- Ask a healthcare provider about the use of compression stockings
- Talk to a healthcare provider about other measures if you are at a high risk of developing blood clots. They may recommend taking aspirin or a one-time injection of low molecular weight heparin.
If you've had blood clots in the past, it's crucial to talk to a healthcare provider about whether you should fly, and if so, what other measures you should take.
Oxygen Needs at Increased Altitudes
Flying results in a statistically significant decrease in oxygen saturation in the blood.
Even though cabins are pressurized on commercial flights, oxygen levels are similar to being at an elevation of 5,000 to 8,000 feet.
Oxygen levels may be lower than this on small planes. For those who are healthy, the body accommodates to this lower oxygen saturation quite well. But for those who have compromised lung function due to respiratory ailments, COPD , lung cancer , or lung metastases from other cancers , this can pose a problem.
If you suffer from a respiratory condition you may require supplemental oxygen for flying even if you do not require oxygen on the ground. Talk to a healthcare provider before flying. They may be able to make recommendations or offer tests to determine if you will require oxygen in flight. While commercial airliners carry oxygen, this is reserved for emergencies.
Estimating Your Need for Oxygen When Flying
For people who have COPD and cancer, or who aren't certain whether oxygen may be required, a healthcare provider may be able to make a prediction based on specific tests. Researchers have developed a pre-flight algorithm that can be used to predict whether or not you may need in-flight oxygen. Since it's been found that people with respiratory disease tend to underestimate their potential need for oxygen when flying, this is a helpful approach for making the decision more objective.
Traveling With Oxygen
Some airlines—but not all—allow portable oxygen to be carried on board the aircraft. According to TSA, if you are able to disconnect from oxygen it's recommended that you check your oxygen as checked baggage.
While checking your oxygen is the ideal method of transport, if you require oxygen when on the ground it's likely that you will require oxygen to an even a greater degree while flying.
If you plan on using portable oxygen in flight it's important to call the airline ahead of time to understand any restrictions. It's also necessary to check with the manufacturer of your oxygen concentrator to see if it is approved for flying.
Delta airlines does allow approved portable oxygen containers with advance notification (but not devices that contain liquid oxygen). A POC approval form must be received by the airline at least 48 hours prior to flying, and if approved will need to be carried with you when you fly. Several other restrictions also apply. The FAA requires that the battery time is 150% of your cumulative flight times. If you need to rent oxygen, OxygenToGo personnel can help you with this process, but you will need to plan well ahead of your flight.
As airlines differ in their regulations, it is important to check with your airline before flying, leave plenty of time to purchase or rent an approved oxygen device if needed and to receive a healthcare provider’s statement that you require in-flight oxygen.
Just as scuba divers may experience problems due to air pressure under water, changes in air pressure as a result of the increased elevation in flight can potentially cause problems for some people.
It's estimated that gasses in body cavities can expand up to 30% with flying on a commercial airline.
For this reason, healthcare providers recommend not flying for a period of time after certain procedures. For example, it's advisable not to fly for 10 days after a colonoscopy, for two weeks to four weeks after chest surgery, and up to six weeks after brain surgery.
After surgery in general, a wait time—usually around 2 weeks—is recommended as the pressure created by changes in altitude could result in incisions breaking open.
Talk with a healthcare provider if you have a brain tumor or brain metastases as air travel could create brain swelling. Most people with brain tumors can travel by air safely, though symptoms may worsen. In some cases, oncologists may recommend steroids or anti-seizure drugs prior to flying.
Changes in air pressure can also cause swelling in the hands and feet. People with lymphedema , such as after breast cancer surgery, should talk to their healthcare providers before flying as to recommendations. Overall, wearing loose-fitting clothing and staying well hydrated is important in minimizing discomfort at an increased altitude.
Air travel significantly increases the risk of contracting a respiratory infection ranging from the flu, to SARS, to dengue fever aboard aircraft has been noted. A 2018 study quantified this risk to a degree, at least for infections spread by respiratory droplets that are propelled short distances. The relative risk of contracting an infection is roughly 80% for people seated within one row (a row in front or row behind) or within two seats on each side of a passenger who is ill with a cold or flu virus. This risk drops to less than 3% for those further away. The risk can also vary depending on movement up or down the aisle, with the greatest risk conferred by ill flight attendants.
Fortunately, the absolute risk is much lower (about one passenger infected for each ill passenger that boards the plane) and there are some things you can do to avoid exposure. Carrying hand sanitizer is one (of course, less than three ounces) that can be used to wipe down the tray table, seatbelt buckle, and bathroom doors. If you note someone coughing or sneezing, you could also let the flight attendant know that you are a cancer passenger and have him or her ask if anyone is willing to trade seats with you. Wearing a mask is also an option.
Flying During Chemotherapy (Between Chemotherapy Infusions)
If your white blood cell count is low due to chemotherapy or your cancer itself, talk to a healthcare provider about whether or not you should wear a mask. Also, ask them for recommendations about the right mask since some may offer more protection against germs than others. Chemotherapy-induced neutropenia a low level of the type of white blood cells called neutrophils that fight infections) can be a challenge when traveling in many ways.
There are many "hidden" risks of infection when you leave home, and it's helpful to learn about ways to prevent infections if possible whether traveling by air or not.
Vaccinations
Vaccinations may be required for travel to certain regions of the world. Live vaccines, such as the MMR, yellow fever vaccine, and oral typhoid can be dangerous for those who are immunocompromised. In contrast, some immunizations may be recommended, such as the injectable flu vaccine. It's important to note that even if immunizations are considered okay, they may be less effective or ineffective for people undergoing treatment for cancer.
When you think about your upcoming trip you may picture yourself traveling as you did before cancer. Yet cancer fatigue , whether it is the fatigue the majority of people experience during treatment or that annoying fatigue that persists long after treatment is done, may leave you exhausted unless you plan for extra rest during your journey. You may find it helpful to write down the activities you wish to take part in at your destination, and then prioritize them as:
- Something you really want to do
- Something you would like to do if you have time
- Something that is optional
If you list out your planned activities in this way you will be more likely to participate in the activities you most wish to do, and will hopefully feel less guilty when you need to take a day or two and just rest.
Many airlines, as well as companies such as Expedia and Travelocity, offer travel insurance when you purchase your airline tickets. This is often a small price to pay relative to the cost of your ticket, but the coverage can vary. Some cover only the cost of your ticket, and documentation by a healthcare provider of a medical reason for the change or cancellation may be required. Others offer services in addition to reimbursing your ticket cost, such as emergency medical care at your destination. Make sure to read the fine print.
A Word From Verywell
Once you've thought through the physical issues related to flying, you may have concerns about the financial issues. If you are traveling by air for treatment, you may be able to get some assistance. Several organizations provide free air travel for those with cancer who need to travel for medical treatment.
Remember that flying is only one part of your journey. Take the time to think through lodging, transportation, and other issues ahead of time so you are prepared to enjoy your time away.
Moore DC. Drug-induced neutropenia: a focus on rituximab-induced late-onset neutropenia . P T . 2016;41(12):765-768.
Transportation Security Administration. Disabilities and medical conditions .
Transportation Security Administration. Medical marijuana .
Stoller JK. Patient education: Supplemental oxygen on commercial airlines (Beyond the Basics) . UpToDate .
Edvardsen A, Akerø A, Christensen CC, Ryg M, Skjønsberg OH. Air travel and chronic obstructive pulmonary disease: a new algorithm for pre-flight evaluation . Thorax . 2012;67(11):964-9. doi:10.1136/thoraxjnl-2012-201855
OxygenToGo. Delta air lines process .
Delta. POC approval and battery approval request .
Bagshaw M, Illig P. The aircraft cabin environment . Travel Medicine . 2019;429-436. doi:10.1016/B978-0-323-54696-6.00047-1
Perdue C, Noble S. Foreign travel for advanced cancer patients: a guide for healthcare professionals . Postgrad Med J . 2007;83(981):437-444. doi:10.1136/pgmj.2006.054593
Phillips M, Saria M, Eisenberg A, Kelly DF, Barkhoudarian G. Safety of commercial airflight in patients with brain tumors: a case series . J Neurooncol . 2018;139(3):617-623. doi:10.1007/s11060-018-2905-6
Breastcancer.org. Lymphedema .
Mangili A, Gendreau MA. Transmission of infectious diseases during commercial air travel . The Lancet . 2005;365(9463):989-996. doi:10.1016/s0140-6736(05)71089-8
Hertzberg VS, Weiss H, Elon L, Si W, Norris SL. Behaviors, movements, and transmission of droplet-mediated respiratory diseases during transcontinental airline flights . Proc Natl Acad Sci USA . 2018;115(14):3623-3627. doi:10.1073/pnas.1711611115
Lustberg MB. Management of neutropenia in cancer patients . Clin Adv Hematol Oncol . 2012;10(12):825-6.
Ariza-heredia EJ, Chemaly RF. Practical review of immunizations in adult patients with cancer . Hum Vaccin Immunother . 2015;11(11):2606-14. doi:10.1080/21645515.2015.1062189
Josephs L, et al. Managing patients with stable respiratory disease planning air travel: A primary care summary of the British Thoracic Society recommendations . Prim Care Respir J . 2013;22(2):234-8. doi:10.4104/pcrj.2013.00046
Thibeault C, Evans A. AsMA medical guidelines for air travel: Airline special services . Aerosp Med Hum Perf . 2015;86(7):657-8. doi:10.3357/AMHP.4224.2015
Transportation Security Administration. TSA Travel Tips - traveling with medications .
By Lynne Eldridge, MD Lynne Eldrige, MD, is a lung cancer physician, patient advocate, and award-winning author of "Avoiding Cancer One Day at a Time."

Holiday travel tips for cancer patients
This page adheres to our medical and editorial policy and guidelines .

For the past four years, public health concerns have put a damper on holiday travel for many people, especially cancer patients and others at risk of becoming seriously ill from airborne viruses.
Last winter a “tripledemic”— the flu, COVID-19 and the respiratory syncytial virus (RSV)—resulted in a spike in hospitalizations and deaths throughout the United States. Some experts are saying the virus trifecta could occur again in 2023.
And if traveling with cancer wasn’t stressful enough, the Transportation Security Administration (TSA) announced recently that it anticipates the 2023 holiday travel season to be the busiest ever. More than 30 million people traveled by air for Thanksgiving. And about 40 percent more American adults are expected to travel for Christmas, Hanukkah, Kwanzaa and other winter holidays this year. That’s likely to mean flight delays and crowded airports, including restrooms and restaurants, where viruses are easy to catch.
So, should cancer patients avoid travel during the holidays, or are there common-sense measures they can take to travel safely?
“Things are a lot better this year,” says Suji Mathew , MD, Infectious Disease Physician and Chief of Medicine at City of Hope ® Cancer Center Atlanta . “We’re definitely in a better place, thanks to vaccines and treatments available. But cancer patients, because they’re immunocompromised , should just be more vigilant.”
Before planning your out-of-town celebrations with family and friends, it’s wise to protect yourself using the travel safety tips covered in this article, which include:
Considerations when traveling with cancer
Planning travel around cancer treatment, how soon after chemotherapy can you travel, what cancer patients should bring while traveling.
- When to avoid travel when you have cancer
If you’ve been diagnosed with cancer and are interested in a second opinion on your diagnosis and treatment plan, call us or chat online with a member of our team.
It’s important for cancer patients, especially those receiving treatment and/or taking drugs that suppress immunity, to consider the risks of becoming infected with one of the many common viruses. Viruses may be contracted through the air we breathe, water we drink, foods we eat and surfaces we touch. Before you travel, be informed by reading up on the following travel safety precautions.
Protect yourself against infection
Before traveling in the U.S., the Centers for Disease Control and Prevention (CDC) urge everyone who is eligible for the flu, COVID-19 and RSV vaccines to get vaccinated. (Note that all three vaccines are free to the public, regardless of health insurance status.)
If you’re traveling outside the U.S., your destination may have its own exposure risks. Popular destinations, including Europe, still have outbreaks of measles and other vaccine-preventable diseases. Before you travel, check the CDC’s travel health information page for your destination to see a list of the vaccines and/or medicines you may need.
At least one month before traveling internationally, see your health care provider to get the vaccines and/or medicines you need for your specific destination, CDC experts advise.

Choose a safe method of travel
“Many patients have to or prefer to fly,” says Jeffrey Metts , MD, MPH, Chief of Staff at City of Hope Cancer Center Atlanta. But those who opt for car or RV travel have a lower risk of being exposed to viruses. “Traveling by car or RV is going to be safer than going through an airport, assuming that you’re in a small group and no one traveling with you is infected.”
Patients undergoing cancer treatments and those who have cancers that make them more likely to be immune-compromised are at higher risk if they’re infected, Dr. Metts says. Examples include blood cancers , such as leukemia or lymphoma , and certain types of pancreatic cancer .
However, if you must or prefer to travel by air, consider the following air travel health safety precautions.
Travel safely by air
- Keep disinfectant wipes and hand sanitizer handy. Even though airlines follow deep-cleaning procedures between flights, it’s still a good practice to wipe down your own area.
- Wear comfortable clothing, such as pants and a long-sleeved shirt for increased protection. Remove your clothes as soon as possible after you get to your destination and wash them before wearing them again.
- Clean your hands frequently with soap and water or hand sanitizer, especially after touching surfaces around your seat and before eating or drinking.
- For those with lymphedema , wear compression sleeves and loose clothing, and move around as much as is comfortably possible to help prevent swelling due to changes in cabin pressure.
- Get up once an hour to improve circulation, drink lots of bottled water, and skip alcoholic or caffeinated beverages. Staying hydrated and mobile may help prevent blood clots, which can develop during long flights and are a risk for patients with specific types of cancers as well as those undergoing chemotherapy or who had surgery
Take advantage of TSA services
- Request a wheelchair in the airport if you’re not able to do a lot of walking.
- Ask to board the plane early or have assistance when boarding.
- If you need assistance during airport security screening, call TSA Cares 72 hours before your flight. The helpline (855-787-2227) is designed to help travelers with disabilities, medical conditions and other special circumstances.
- If you don’t call ahead and don’t want to discuss your medical condition in front of strangers, use TSA notification cards .
- Before screening, let a TSA officer know if you have an external medical device, such as a port or ostomy bag, and where it’s located. Also, let the TSA officer know if you’d like a caregiver to accompany you during screening.
- Breast prostheses and mastectomy bras are considered medically necessary and may be worn during screening. Patients will not be asked to remove them.
- TSA has standardized screening procedures for various medical conditions and disabilities, including allowing a passenger with an ostomy bag to perform his or her own pat-down. The passenger’s hands would then be tested for traces of explosives. The passenger may still be required to undergo a standard pat-down on areas of the body that are not connected to the ostomy bag. TSA provides information specific to various situations .
Cancer treatments shouldn’t prevent you from traveling this holiday season, but planning ahead is key. Talk to your care team about your upcoming appointments, including those scheduled for CT scans and other diagnostic imaging tests used to evaluate whether and to what extent your treatment is working.
In some cases, doctors and patients may be able to discuss adjustments in treatment regimens to allow for holiday travel. Don’t put off treatment solely because of the holidays and without talking to your care team. Missing an appointment may cause an interruption in your treatment plan, allowing cancer to progress.
If you’re not experiencing side effects from chemotherapy treatments or are able to manage them, it may be fine to travel. Make sure you’re cleared for travel by your oncology team. To determine if travel is appropriate for you, your doctor may need to know details about your trip, including your method of travel, where you’ll be staying and if you’ll have access to medical supplies, pharmacies and medical care.
If you plan to fly, ask your doctor what precautions to take while aboard the plane, such as wearing compression sleeves or socks, since chemotherapy may put you at greater risk of developing blood clots.
It’s also important to consider the timing of your trip. Find out from your doctor when your white blood cell count is likely to be the lowest, since this is when you’re most at risk for infection. This usually occurs between seven and 12 days after you finish each chemotherapy dose and may last up to a week.
Avoid traveling on days you’re most likely to experience side effects , such as fatigue or nausea . This may vary by a few days with each treatment, so keep notes and book your departure dates accordingly.
Traveling during the busy holiday season can be a hassle when you’re not dealing with cancer. Taking a few extra steps will help ensure you’re feeling your festive best this season.
Many of the things you’ll want to pack for your trip are obvious, like your prescription medications and over-the-counter drugs you take regularly. But when traveling with cancer, you’ll want to anticipate items you may need if you become ill. Also, your body may be more sensitive to sunlight, bug bites and changes to your diet, so plan ahead by adding the items listed below to your packing list.
Prescriptions in their original bottles. If possible, bring at least an extra two-week’s supply of each medicine you take. You never know if your trip may get extended for unanticipated reasons.
Over-the-counter medications. Be sure to include drugs you use for pain relief as well as stomach issues including diarrhea and constipation.
Your medical records. Paper copies or a patient portal app on your phone will give you quick, accurate information if you need to go to a hospital or see a doctor while on vacation. The records should include your medication list, with dosages, and the surgeries you’ve had.
Health insurance cards. Carry the originals and also carry pictures of them on your phone (in case they’re misplaced or your wallet is stolen) of all health insurance cards (your regular plan and/or supplemental travel health insurance plan).
Emergency contact information containing the street addresses, phone numbers and e-mail addresses of the following: family member or close contact, your health care provider(s) at home, lodging at your destination, hospitals or clinics (including emergency services) at your destination, U.S, embassy or consulate in the destination country or countries.
Food and beverages. To be sure you stay hydrated and nourished, carry bottled water and crackers or energy bars. Hard candies or lozenges may also help relieve common treatment-related side effects like nausea, mouth sores and dry mouth .
Sunscreen, a hat and protective clothing . Patients undergoing chemotherapy or radiation treatment may have increased sensitivity to the sun and sunburn susceptibility, so if you’re traveling to a tropical climate, bring what you need to protect your skin.
Infection protection . Use insect repellent to avoid mosquito bites that can lead to infection. Also bring a first aid kit to treat cuts and scrapes right away, especially in hot, humid climates.
When to avoid traveling when you have cancer
At times during your cancer treatment it may not be not safe to travel. For example, if you’ve had surgery, you may need to wait several weeks before flying. Consult with your doctor for recommendations since different types of surgery have different air travel restrictions.
Also, flying may not be safe for patients with some types of cancers or who are receiving certain cancer treatments, since changes in pressure and oxygen levels in the airplane cabin may cause serious side effects. Again, it’s best to talk to your doctor.
Naturally, don’t travel if you’re feeling sick—a headache, stuffy nose, sore throat or fever are all signs you may have a virus, such as the flu, RSV or COVID-19 .
If you’re feeling well and your doctor approves, don’t hesitate to travel to spend the holidays with loved ones. Creating new memories may give you the lift you’ve been longing for this season. Just be sure to guard your health by adding these holiday travel precautions to your checklist.
Related Articles
How soon can you go on holiday after radiotherapy?
I am after some much needed advice…
how soon after radiotherapy is it safe to go abroad?
i am due to finish radiotherapy on Thursday 18th August, after what will be 9 months of enduring a lumpectomy on both breasts, 6 rounds of chemotherapy and what will be 30 sessions of radiotherapy. Therefore I absolutely desperate to go on holiday for a much needed rest and recuperation!
We are looking today at the last week of August, first week of September, is this to soon?
any advice would be greatly received ?
Hi Sunflower Dinkle,
I have moved your post to the Radiotherapy Board in order to give users more of a chance to see it and respond.
In the meantime you can always look at our page on travelling abroad with breast cancer and call our helpline at 0808 800 6000 who will be able to talk to you about going abroad after radiotherapy. The opening hours are below.
Monday-Friday, 9am-5pm Late opening Wednesday 9am-7pm, Saturday, 9am-1pm
Best wishes,
Hi Sunflower. I’m due to finish on 9/8 and have just booked flights to go to our home in Spain on 17/8. My skin is sore and irritated but not broken and I have plenty of high necked tops in my wardrobe I can wear. I’m only going for a long weekend but I’m desperately in need of a warm break. I’ll be good and stay out of the direct sun (can’t imagine wanting to sit in the sun anyway as I’m fried enough!), but I just need a few days to relax, sleep without an alarm clock programmed to wake me and the sound of the sea which I find soooo relaxing. Not sure if any of that helps but do what feels right for you would be my best advice but be careful in the sun - your skin around the radiotherapy site will be very sensitive and may be sore. Take care. Hugs.
Hi Ladies, I went abroad last year a couple of weeks after finishing rads and was totally fine, I used factor 50 on my radiated skin and and wore a bikini without any problems, the rest was just what we needed after the previous stressful months so I would say go and enjoy yourselves, God knows you deserve it! Xx
Notification
Holiday after radiotherapy.
my husband has completed 31 out of 37 sessions if radiotherapy for T3 N0 m0 Gleason 7 (3+4) psa 16 prostate cancer in the anterior lobe ( it took a long time to find) they thought it was T2c after scans but it’s just at the top edge so are treating him as T3.
he is tolerating the radiotherapy well and will be glad not to have to do the 3 hour round trip soon. Staff have been great.
he finishes 12th November and wants to go on holiday in March 2019 and I am wondering if this would him Enough time to recover.
hormone therapy was stopped just as he started radiotherapy ( he had been on prostap/casodex for a year and psa was undetectable prior to radiotherapy)
no long haul holiday maybe just the Canary Islands.
Many thanks for reading
Edited by member 03 Nov 2018 at 10:04 | Reason: Spelling!
Thanks Mr Angry
He was on prostap for a year but it didn't bring his psa down as low as they would have liked so they added casodex for a 3 months prior to radiotherapy and his psa was undetectable before he started radiotherapy. His Oncologist Consultant stopped the prostap and casodex the day before he started 37 sessions of radiotherapy. He tolerated the prostap well but like you had some big flushes (mostly at night). He is still getting the flushes as its still in his system. We are slightly nervous that the hormone therapy has stopped but our Oncology consultant said his psa was under 20 and his Gleason was 3+4 and he had been HT for a year so he was in that grey middle ground area. 6 radio sessions to go then it will be the "pre psa anxiety" for the next few years at least.
My Husband is 63 and had bowel cancer 13 years ago - he got the all clear and cured of bowel cancer at 10 years and unfortunately we only had a short breather before prostate cancer was diagnosed. Life is a very peculiar rollercoaster that is for sure.
Edited by member 03 Nov 2018 at 14:48 | Reason: addition
Hi Very Jenny,
I agree with lynn, my husband finished TH 37 sessions in February and we went on holiday in May, a much needed break. We chose to go on a short flight and went to Puerto Pollensa in Majorca. The weather then was ideal, bright,sunny and just the right temperature. We really enjoyed our holiday, although he was a bit unwell for a few days, I think I panicked a little as I have done every time he has shown any signs of illness ever since he was diagnosed! We didn't do all the things we planned, preferring to just relax and unwind, but when we got home and reflected we felt we had had a very good holiday!
To make up for the four lost days when he didn't want to go out, we had a short break in Rutland a few weeks later so I got two holidays!
My advice is that a good holiday after the radiotherapy is important for both of you, I kind of feel the whole process is exhausting for both of you, and you need to get away from the situation, and may be reconnect with each other without the pressure of daily trips to hospital and waiting to learn results.
Hormone treatment is on going to my husband, probably for 3 years in total, and while the effects of that are more problematic than the radiotherapy, he does seem to be coping much better now, so we are dating to begin to feel hopeful for the future.
Have a good holiday!
A holiday will do you good in many ways. My oh had 33 sessions at the start of the pc journey and was tired for a few weeks afterwards with some breathlessness on exertion such as hills but it soon calmed down and we walked as much as we could to get him back to fitness, also some rowing on a machine.
The thing to do is rest when you need to, sleep when you need to and get back to a new normal. The psa anxiety is something you learn to accept over time. Just enjoy every moment together.
Thank you so much for replying mikesmum and gillyj we really appreciate it and will follow all the advice that has been given! It’s just reassuring to know there are people and their partners out there who are willing to help and support others xxx Thank you 😊
Edited by member 03 Nov 2018 at 20:40 | Reason: Their not there!
Hi VeryJenny,
I flew to Calgary in Canada (almost 9 hours flying time) on July 6th having finished salvage radiotherapy April 27th. I got travel insurance without any major issues covering all my health issues. I was still on HT too.
My wife and I had a great time.
Book a holiday soon!
we have booked the holiday!
We live in Dunblane and the drive to the Beatson Glasgow every day for 33 days (today) with 4 to go has been quite tiring although my husband hasn’t complained once. So we have a holiday to look forward to now!
seeing oncologist middle of January so fingers crossed The scores on the doors will be ok!
thanks for replying
Great, enjoy the hol.
I went to India and Nepal two weeks after my radiotherapy had finished. Went with loads of pads and pull up adult nappies. They were mainly for security. I had no major issues. My doctor was fine with me going.
In October, 3 months post radiotherapy, i did have symptoms of radiation proctitus/pelvic radiation disease. Basically lost all bowel control.
The moral of the story is that some things are pot luck. I love travelling (going to Antarctica this weekend) and I keep my travel insurance company up to date with any issues I have, take my pads and my meds and keep going. I'm not wreckless, but I'm determined not to let PCa take seeing the world away from me.
Some great advice as usual on this thread. My Onco is scheduling Radiotherapy for the whole of April 2019, my wife is planning to retire from work at the end of June so I'm planning a special holiday for her following retirement
The gist of the comments here are it is sensible to take a 2 month break after Radiotherapy to regain strength and get yourself ship shape so realistically the earliest i should be looking to book anything is July or maybe August?
Edited by member 14 Dec 2018 at 11:30 | Reason: new
Originally Posted by: Online Community Member
One of the main issue is skincare- your midriff may already be a bit sunburnt so if you are planning on going somewhere hot, factor in that you will need to use high SPF and will probably not be laid shirtless by the pool for hours. John is very dark skinned so the RT didn't cause him any real soreness but 5 years on he still needs to wear factor 50 round his belly and hips. Blond and pale skinned men can actually find their skin burns towards the end of RT.
Edited by member 14 Dec 2018 at 21:55 | Reason: Not specified
Finished RT april 2014, flew to south carolina may 2014 for a holiday, ran 100 kilonetre ultramarathon in june 2014, go for it 😁
T4n1m1a still running ultramarathons, got back from Cambodia having run 220 kilometres last week, 4 years after diagnosis then chemo, RT, if you want to do it and feel ok why wait?
Dream like you have forever, live like you only have today Avatar is me doing the 600 mile Camino de Santiago May 2019
Originally Posted by: Online Community Member In October, 3 months post radiotherapy, i did have symptoms of radiation proctitus/pelvic radiation disease. Basically lost all bowel control.
How long did your problems last for, Ulsterman?
Join the online community now.
Click through to become a member and gain access to support, information and real time replies.
For the best browsing experience please enable JavaScript. Instructions for Microsoft Edge and Internet Explorer , other browsers

- About cancer
- Get involved
- Our research
- Funding for researchers
- Cancer types
- Cancer in general
- Causes of cancer
- Coping with cancer
- Health professionals
- Do your own fundraising
- By cancer type
- By cancer subject
- Our funding schemes
- Applying for funding
- Managing your research grant
- How we deliver our research
- Find a shop
- Shop online
- Our eBay shop
- Our organisation
- Current jobs
- Cancer news

Having external radiotherapy
Your appointments for external radiotherapy will be in the radiotherapy department or proton beam therapy centre. External radiotherapy doesn't hurt although laying on the radiotherapy couch can be uncomfortable.
How often you have external radiotherapy
You have radiotherapy as a course of treatment and usually as an outpatient. This means travelling each day to the radiotherapy department at your nearest cancer centre or unit. This may be further away than your local hospital. You usually go to the hospital for treatment once a day, from Monday to Friday, with a break at weekends.
You might have a shorter course of treatment or a single treatment if you are having radiotherapy to control symptoms.
The treatment room
Radiotherapy machines are very big and could make you feel nervous when you see them for the first time. The machine might be fixed in one position or able to rotate around your body to give treatment from different directions. The machine doesn't touch you at any point.

Before each treatment session
The radiographers help you to get onto the treatment couch. They help position you on any equipment you are using for the treatment. Because your position is so important, the radiographers may take a little while to get you ready. You can help by trying to relax as much as possible during this time.
The radiographers line up the radiotherapy machine using the marks on your body. Once you are in the right position, they leave the room. This is so they are not exposed to the radiation.
Having external radiotherapy treatment
You need to lie very still. Your radiographers might take images (x-rays or scans) before your treatment to make sure that you're in the right position. The machine makes whirring and beeping sounds. You won’t feel anything when you have the treatment.
Your radiographers watch you carefully. They can see and hear you on a CCTV screen in the next room. They can talk to you over an intercom and might ask you to hold your breath or take shallow breaths at times. You can also talk to them through the intercom or raise your hand if you need to stop or if you're uncomfortable.
You will be alone for a few minutes or up to 15 minutes, depending on the type of treatment you are having. Some treatments, such as total body radiotherapy can take up to an hour.
The short video below shows how you have radiotherapy:
Content not working due to cookie settings.
Dan (radiographer) : Before your treatment starts your doctor will need to work out exactly where the treatment needs to go and also which parts need to be avoided by the treatment. To have radiotherapy you lie in the same position as you did for your planning scans. We then line up the machine based on your tattoo marks. It is really important that you stay very, very still when you are having treatment it is also important to let the radiographers know right at the beginning if you are not comfortable so they can adjust your position.
Radiographer : Ok all done, we’ll be back in a couple of minutes.
Dan (radiographer) : We leave the room and control the room from a separate room This is so we aren’t exposed to radiation. Treatment takes a few minutes and you will be able to talk to us using an intercom. We can see and hear you while you are having your treatment and will check that you are ok. When your treatment starts you won’t feel anything; you may hear the machine as it moves around you giving the treatment from different angles. Because we are aiming to give the same treatment to the same part of the body everyday then the treatment process is exactly the same everyday so you shouldn’t notice any difference. You’ll see someone from the team caring for you once a week while you are having treatment they’ll ask how you are and about any side effects.
Patient : They get you from one sitting area to another and then take you into the room where you undress to the waist and then lie down and line you up by either moving you or asking you to shuffle a little and they check the dimensions and they talk to one another and they say I am fine this side how are you ...yes fine...ok, stay where you are Jeff and that was it. There were a few little clicks and lights go on and off and you can see a green laser beam which line sup with certain things on your body uh so no, no real noise and no discomfort.
You won't be radioactive
This type of radiotherapy won't make you radioactive. It's safe to be around other people, including pregnant women and children.
Travelling to radiotherapy appointments
You might have to travel a long way each day for your radiotherapy. It depends on where your nearest cancer centre is. This can make you very tired, especially if you have side effects from the treatment.
You can ask the radiographers for an appointment time to suit you. They will do their best, but some departments might be very busy. Some radiotherapy departments are open from 7am till 9pm.
Car parking can be difficult at hospitals. You can ask the radiotherapy staff if they can give you:
- a hospital parking permit for free parking
- advice on discounted parking
- tips on free places to park nearby
The radiotherapy staff can usually help to arrange transport for you if you need help with travelling. This usually has to be agreed with your radiotherapy doctor. It is only for people that would struggle using public transport and have no access to a car. It might not always be at convenient times.
Some hospitals have their own drivers and local charities might offer hospital transport. So do ask if any help is available in your area.
Staying near the hospital
There are places you can stay if you find it difficult to get to the hospital. These include:
- the hospital ward (if you are too unwell to travel)
- a hostel ward in the hospital or nearby
- accommodation close to the hospital
Paying for travel costs
You might be able get a grant towards your travel expenses. People on low incomes can sometimes claim the costs from the Department for Work and Pensions.
Ask the hospital social worker or staff in the radiotherapy clinic about grants and how you can claim.
Money might be set aside to help with your travel costs if you are taking part in a clinical trial. Although this is not common. You can ask the staff in the radiotherapy department about that.
Related links
What is external radiotherapy.
External radiotherapy uses radiotherapy machines to aim radiation beams at a cancer. This destroys the cancer cells. There are different types of external radiotherapy.
General side effects of radiotherapy
Radiotherapy can cause some general side effects, such as tiredness and skin reactions.
Planning radiotherapy
Your radiotherapy treatment plan is individual to you. You have a CT scan or MRI scan, to create your radiotherapy plan.
Radiotherapy main page
Find out about cancer treatment with radiotherapy, including external radiotherapy, internal radiotherapy, side effects, radiotherapy for symptoms and follow up after treatment.
Your cancer type
Search for the cancer type you want to find out about. Each section has detailed information about symptoms, diagnosis, treatment, research and coping with cancer.
It’s a worrying time for many people and we want to be there for you whenever - and wherever - you need us. Cancer Chat is our fully moderated forum where you can talk to others affected by cancer, share experiences, and get support. Cancer Chat is free to join and available 24 hours a day.
Visit the Cancer Chat forum
About Cancer generously supported by Dangoor Education since 2010.

Find a clinical trial
Search our clinical trials database for all cancer trials and studies recruiting in the UK
Cancer Chat forum
Talk to other people affected by cancer
Nurse helpline 0808 800 4040
Questions about cancer? Call freephone 9 to 5 Monday to Friday or email us
Air travel after ablation?: We spend a... - Atrial Fibrillati...
Atrial fibrillation support, air travel after ablation.
We spend a lot of time away in the winter & my hubby so looks forward to it.I have an ablation scheduled and wondered how advisable it is to fly asap after published 4 weeks.And although I am very much a person who needs to organize my life I know AF doesn't allow this and will see how things are and book last minute.
I am quite expecting it may not work or not even happen as told only 50% chance .
Just looking for people's thoughts & maybe experience.
After ablation, it is common for patients to be advised to take a few weeks to rest and recover before air travel. The timeline for recovery can vary based on the individual and the specifics of the procedure, but generally, it's recommended to wait AT LEAST 4 weeks before flying.
However, it's important to keep in mind that we are all different and every person's recovery time is also different. Before making any travel plans, I think it's best to check with your doctor to discuss this matter. Personally, I would wait at least a few months before flying after an ablation - that's just me though and you may be fine. You'll likely pay more for a last-minute booking but your health comes first. I wish you a successful recovery. Soak up some sun for me if you do get away.
I was told to wait a couple of weeks, but best to check with your ep, as they know what is involved in your specific procedure, as well as your medical history. But if you do plan on flying close to the permission date they give you, think about traveler's insurance in case you have complications that would delay flying safely.
I flew 5 days after ablation, my EP said he would prefer I waited 2 weeks but that some of his patients flew day or two following with no complications.
I think it’s so individual and you really won’t know till it’s done how you will be so I’d agree with getting good insurance if you book anything prior to having ablation - ifvyou are waiting for a procedure you may find it difficult to be honest. I flew because I was living in Spain at the time so had to return home.
Thanks CDreamer.Impossible to get insurance for existing illnesses for 15 months as waiting for Cv then awaiting ablation.Main worry for me is if something happens on the plane.I sometimes wonder if having a holiday home is worth it anymore . Usually too hot for me from May onwards so can only do 90 days between end of Oct & Apr.
Keep hoping I can get AF sorted & spend more time there.
Keep saying this time next year I will be better.
It’s not impossible but it is difficult and may be expensive so depends upon how deep your pocket is and how much you want to go. What I did when just going to our Spanish holiday home was to take out annual medical insurance locally, didn’t bother about the cost of the flight, that worked.
I’ve been in AF on planes several time and it’s really no big deal - as long as you have plan, don’t stress and stay really well hydrated and don’t tell any of the crew! Stressing about it is the worst and most likely to bring on an episode. I worried more about getting through the airport and the long queues as I can’t stand.
I guess it can wait & something tells me the need to have this conversation is to stop me worrying about the ablation.Think a point in time after the ablation.Scheduled for 22nd.Hope saying the date doesn't jinx it.
Travel insurance maybe be an issue depending on your age and any pre-existing conditions and where you're travelling to usually ok with in the EU area.. long haul is another matter, best get travel advice from your consultant also how quickly you start recovery it will vary from person to person, I had a wound in my groin for a number of weeks after so was grounded for around a month
I was advised after my recent ablation not to go away for 1 to 2 months in case of complications.
Not what you're looking for?
You may also like..., air travel after ablation procedure.
Waking gasping for air after ablation for wpw
travel after ablations
Ablation and travel advice
Ablation and travel
Related Posts
Moderation team
Popular Posts
Content on HealthUnlocked does not replace the relationship between you and doctors or other healthcare professionals nor the advice you receive from them.
Never delay seeking advice or dialling emergency services because of something that you have read on HealthUnlocked.
How to watch an eclipse, safely
A solar eclipse will be visible in a path across North America on Monday, April 8, 2024, from Mexico to the US and Canada. This is a rare opportunity to watch the moon block out the sun. After this event, the next total solar eclipse over the U.S. will not happen for another 20 years.
But it’s important to remember that the rays of the sun can be destructive to your vision, so keep your eyes safe when viewing the eclipse with these tips from the National Eye Institute, a part of the National Institutes of Health (NIH) and the largest funder of vision research.
“Watching an eclipse can be fun, but never look directly at the sun. You can seriously damage the retina and even be permanently blinded,” said Chantal Cousineau-Krieger, M.D., a staff ophthalmologist at NEI’s Consult Service. The retina is the light-sensitive tissue in the back of the eye that sends signals to your brain, enabling vision.
The sun emits high levels of ultraviolet (UV) radiation, which can cause damage to the cells of the eyes' surface and the back of the eye. In addition to UV radiation, the sun also emits infrared radiation, which can generate heat. Direct exposure to intense sunlight can cause thermal damage to the eyes, leading to inflammation, tissue damage, and discomfort.
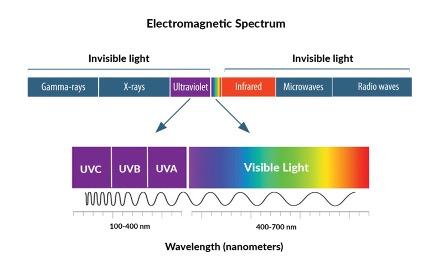
Both UV and infrared radiation are not visible to the human eye, but can be perceived as heat, which can damage eye tissue. Credit: The National Eye Institute (NEI/NIH)
The main risks associated with watching a solar eclipse (or looking directly at the sun any time) include:
Solar Retinopathy: a condition where the light-sensitive cells in the retina are damaged. This is caused by the sun's intense light, and it can result in a permanent loss of vision. Symptoms include blurred vision, sensitivity to light, dark spots or “blind spots” in your central vision, changes in color perception (or difficulty in distinguishing between colors), or a sensation of pressure in the eye.
It's important to note that the symptoms of solar retinopathy may not appear immediately after sun exposure and can develop gradually over hours or days. In some cases, the symptoms may resolve on their own, but in more severe cases, they may persist or worsen over time.
If you experience any of these symptoms after viewing a solar eclipse or being exposed to intense sunlight, it's essential to seek medical attention from an eye care professional promptly. Early diagnosis and treatment can help prevent further damage to the retina and preserve vision.
Photokeratitis: also known as "sunburned eyes" or "welder's flash," can occur from exposure to intense ultraviolet (UV) radiation from the sun. Symptoms may include pain, redness, tearing, and a feeling of sand in the eyes. While this condition is usually temporary, it can be quite uncomfortable. In some cases, photokeratitis may cause involuntary twitching or spasms of the eyelids (blepharospasm). These spasms may occur as a protective mechanism in response to eye irritation.
Repeated episodes of photokeratitis can increase the risk of long-term eye damage, including cataracts and pterygium, an abnormal growth of tissue on the conjunctiva (the clear membrane that covers the white of the eye) and the cornea (the clear front surface of the eye). If you experience symptoms of photokeratitis after exposure to UV light, it's essential to seek medical attention from an eye care professional for evaluation and treatment.
Macular Edema: Prolonged exposure to the sun, especially during an eclipse, can contribute to macular edema, a condition where the central part of the retina swells, leading to vision distortion and potential permanent damage.
Macular edema can reduce contrast sensitivity, making it challenging to distinguish between objects of similar colors or shades. Colors may appear less vibrant, and details may be harder to discern.
Symptoms of macular edema may also develop gradually over time, and some individuals may not experience noticeable symptoms until the condition progresses. If you experience any changes in your vision, especially central vision, it's essential to see an eye doctor to prevent further vision loss.
Protect your eyes
A solar eclipse can be viewed safely by looking through special-purpose solar filters. These filters must meet an international standard, indicated by ISO 12312-2 certification. They must have the manufacturer’s name and address printed somewhere in the product, and not be older than three years or have any scratches on the lenses.

Make sure you pretect your eyes while watching an eclipse. In order, from left to right: Binoculars filters, viewing glasses and cards and ohoto camera filters should always be used for total or partial eclipse viewing. Credit: The American Astronomical Society (AAS)
Never look at the sun through binoculars, photo cameras, telescopes or any optical device using eclipse glasses or handheld filters. The sun will burn through them and damage your eyes. There are special filters that can be attached to the front of optical equipment if you choose to watch the eclipse that way.
“While UV-blocking sunglasses are important to keep your eyes healthy, even very dark glasses cannot protect your eyes from damage caused by looking directly at the sun,” Cousineau-Krieger said. Regular sunglasses, damaged solar filters, or peeking between your fingers or through a pinhole to watch a solar eclipse is not safe.
The only safe way to watch a solar eclipse without a filter is by turning your back to the sun and watching a projection. “Devices such as pinhole projectors allow you to watch an indirect image, which is safe and still exciting,” explained Cousineau-Krieger.
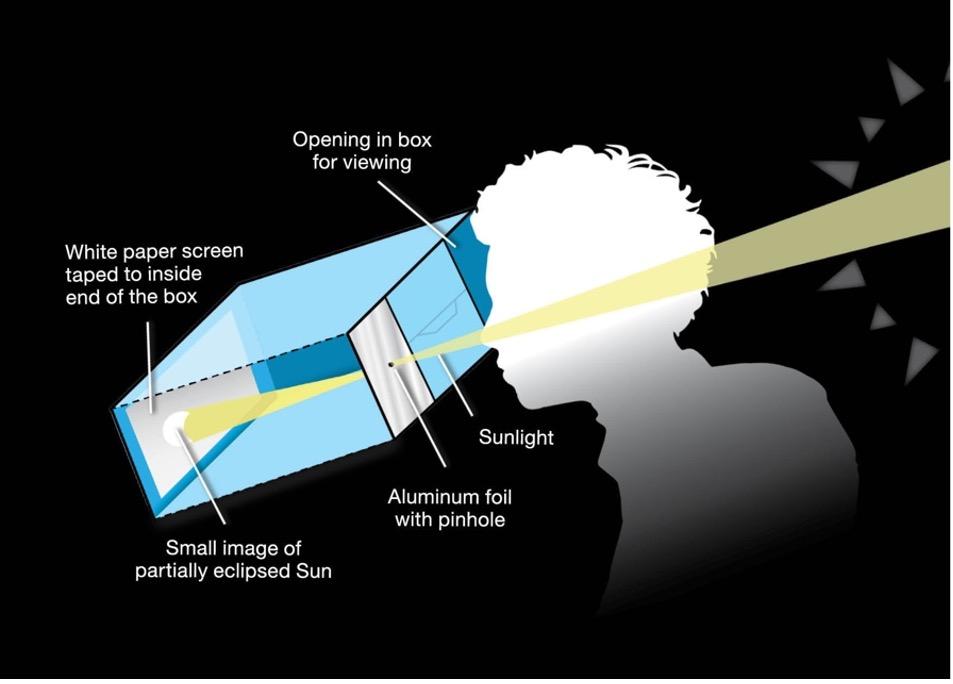
Using a pinhole projector is a safe and easy way to experience a solar eclipse without the risk of eye damage from direct sunlight. It's suitable for individuals of all ages and requires minimal materials to construct. Image source: NASA
To learn more about solar eclipses and how to watch them safely visit:
- https://science.nasa.gov/eclipses/safety/
- https://www.aao.org/eye-health/tips-prevention/solar-eclipse-eye-safety
- https://eclipse.aas.org/eye-safety
- https://eclipse2024.org/eclipse_cities/statemap.html

IMAGES
COMMENTS
WallyDug! The radiotherapy carries on working after you finish treatment and the maximum effects are felt 10 to 14 days after completion. Everyone is different of course with regards to tiredness and skin reaction. You may enjoy your holiday more if you leave it a month after you finish treatment as your skin will be healing.
Or you may be more sensitive to the sun after having radiotherapy or certain cancer drugs. There could also be practical issues to think about, such as: whether you'll have the facilities you need if you get tired easily; will you need wheelchair access. You also need to think about when to travel. There are times when you shouldn't travel ...
It's OK to get away and do something fun even while you're in the very serious process of cancer treatment. "People who are undergoing cancer treatment need vacations just as do people who ...
Cancer treatments, like radiotherapy and chemotherapy, can sometimes cause short-term physical problems. Some treatments can also make your skin more sensitive to the sun. These effects can limit the amount of travelling you can do - or the type of activities you do while you're away. If you want to travel abroad, it can also be more ...
Travel is perfectly safe for cancer patients most of the time, and we want you to enjoy your life. But you never know exactly what might happen, so it's good to be prepared.". Request an appointment at MD Anderson online or by calling 1-877-632-6789. Some elements of travel are the same for everyone.
Getting Around. Reducing Blood Clots. Oxygen Needs. Air Pressure Changes. Infection Concerns. Cancer Fatigue. Travel Insurance. Flying on commercial airlines is usually very safe for people with cancer who are stable, reasonably healed from any surgeries, and do not have a very low white blood cell count or platelet level due to chemotherapy.
Most people who have cancer can travel without problems. But there are times when it's best not to travel. ... Doctors usually say avoid going abroad for at least 6 months after a bone marrow or stem cell transplant. Most people need to have regular check ups. You might also need blood transfusions during this time. Once your blood counts have ...
It's possible to walk around in most forms of travel, except by car. And even then you can stop for regular breaks. ... Your doctor might advise you against going abroad for the first 6 to 12 months after intensive treatment. ... Radiotherapy can also make the skin where you had treatment sensitive to the sun for many years. Keep the skin ...
Travel safely by air. Keep disinfectant wipes and hand sanitizer handy. Even though airlines follow deep-cleaning procedures between flights, it's still a good practice to wipe down your own area. Wear comfortable clothing, such as pants and a long-sleeved shirt for increased protection.
When you have radiotherapy you are not radioactive in any way unless you are having internal radiotherapy (where they insert radioactive materials for slow release) so will be perfectly safe to see anyone. Its like having an xray. As soon as the xray has been done, the harmful bit has gone. There is lots about safety etc on Cancer Research website.
Most importantly, when scheduling a vacation after treatment, do not schedule it too close to your last day of treatment. Often times treatments may end later than originally expected due to radiation machine downtime or delays in treatment due to side effects. If you are planning on vacationing prior to your treatments, be prepared.
Travel insurance is likely to be more expensive after a diagnosis of prostate cancer - even if you're not having treatment or if the cancer is under control. Insurance is worked out by averages and risks. Because insurers think you're more likely to need medical assistance on your trip, they charge more. Most men with prostate cancer can find ...
External radiation therapy is given from an outside source, involves a beam of radiation aimed at a part of the body, and affects cells in your body only for a moment. Because there's no radiation source inside your body, you are not radioactive at any time during or after treatment. Internal radiation therapy (brachytherapy)
Lines open: Monday to Friday - 9am to 4pm; Saturday - 9am to 1pm. It can be difficult to talk to someone in person about breast cancer concerns. Explore other ways you can ask a question. Find out more about travelling when you have breast cancer, including travel insurance, medication, prostheses and vaccinations.
In the meantime you can always look at our page on travelling abroad with breast cancer and call our helpline at 0808 800 6000 who will be able to talk to you about going abroad after radiotherapy. The opening hours are below. Monday-Friday, 9am-5pm. Late opening Wednesday 9am-7pm, Saturday, 9am-1pm. Best wishes, Lizzy. JayG 3 August 2016 18:01 3.
I went to India and Nepal two weeks after my radiotherapy had finished. Went with loads of pads and pull up adult nappies. They were mainly for security. I had no major issues. My doctor was fine with me going. In October, 3 months post radiotherapy, i did have symptoms of radiation proctitus/pelvic radiation disease. Basically lost all bowel ...
Travel and prostate cancer. Going on holiday can be a great way to relax and get away from things. Having prostate cancer shouldn't stop you from travelling but you may need to plan and make special arrangements to help you enjoy your trip. On this page, we give tips on preparing for your trip, arranging travel insurance and how to look after ...
The following questions and answers may help you find the right insurance. Lifestyle Specialist urses 0800 074 8383 prostatecanceruk.org 6. If you're travelling outside of Europe, you'll need worldwide cover which can be more expensive than European cover. This is because medical treatment usually costs more in non-EU countries.
How often you have external radiotherapy. You have radiotherapy as a course of treatment and usually as an outpatient. This means travelling each day to the radiotherapy department at your nearest cancer centre or unit. This may be further away than your local hospital. You usually go to the hospital for treatment once a day, from Monday to ...
Hi KKtaz. After ablation, it is common for patients to be advised to take a few weeks to rest and recover before air travel. The timeline for recovery can vary based on the individual and the specifics of the procedure, but generally, it's recommended to wait AT LEAST 4 weeks before flying. However, it's important to keep in mind that we are ...
The only safe way to watch a solar eclipse without a filter is by turning your back to the sun and watching a projection. "Devices such as pinhole projectors allow you to watch an indirect image, which is safe and still exciting," explained Cousineau-Krieger. Using a pinhole projector is a safe and easy way to experience a solar eclipse ...