

Chart, Code, and Bill for E&M Office Visits
- See 6 Related Articles
- Share this article
Upon completion of encounters, a clinician selects billing codes. They often select an “Evaluation and Management” or E&M code, either for new or established patients. This is sometimes called the “office visit” code. E&M code selection is based on medical decision making and the amount of time spent.
This article collects resources and guidelines for E&M office visits, with some tips on implementation in PCC EHR.
On January 1st, 2021, the guidelines for coding and billing an office visit changed significantly.
Procedure Code Guidance: The procedure code recommendations in this article are intended only as examples. You should consult the AMA’s CPT Coding Guide and work with your insurance payers to verify what codes you should use on claims. Your practice updates and maintains your procedure list, codes, and prices in the Procedures table in the Table Editor on your PCC system.
- 1 Why is E&M Code Selection Important to a Pediatric Practice?
- 2.1 Select a Code Based on Medical Decision Making
- 2.2 Select a Code Based on Time
- 3 PCC’s 2021 E&M Coding Tool
- 4 Watch PCC 2021 E&M Coding Videos
- 5 Configure PCC EHR to Support Your Clinicians and Billers for E&M Level Selection in 2021
- 6 Additional Resources and Guides
- 7.1 Questions and Answers
Why is E&M Code Selection Important to a Pediatric Practice?
E&M services make up the bulk of the work you do as a pediatrician. They represent the cognitive work, information gathering, and decision making that goes into a patient encounter. A pediatrician’s time with patients is going to be classified as E&M more than often than with other medical specialties. Because most of the work you do falls under the umbrella of E&M, it’s vital that you code those services correctly. Many pediatricians under-code their encounters, resulting in significant lost revenue for their practice.
Coding your E&M services correctly is not only a matter of revenue. The requirements for documenting each level are also intended to provide appropriate and adequate information for continuity of care.
How Do I Select an E&M Code in 2021?
For encounters that occur after December 31st, 2020, a clinician no longer uses history or physical exam performed during the encounter as criteria for code selection. Instead, they select a code based on either medical decision making or time spent practicing care for the patient on the day of the visit.
Here’s a brief explanation of how you select a billing code level for an “evaluation and management” or “Office Visit” after January 1st, 2021. These guidelines apply to common visit billing codes, such as 99212, 99213, 99214, or 99215, as well as to the selection of codes 99202 through 99205.
Select a Code Based on Medical Decision Making
You can base your visit level code on medical decision making, which is comprised of three elements:
Problems Addressed: The number of problems you addressed for the patient during the day of the encounter.
Items Reviewed: The tests, chart information, and other data you reviewed in relation to the problems addressed today.
Risk: The level of risk presented to the patient.
Select a Code Based on Time
You can base your visit level code selection on the total time that the rendering clinician spent on the patient that day. That can include the time the pediatrician spent before, during, and after the actual encounter.
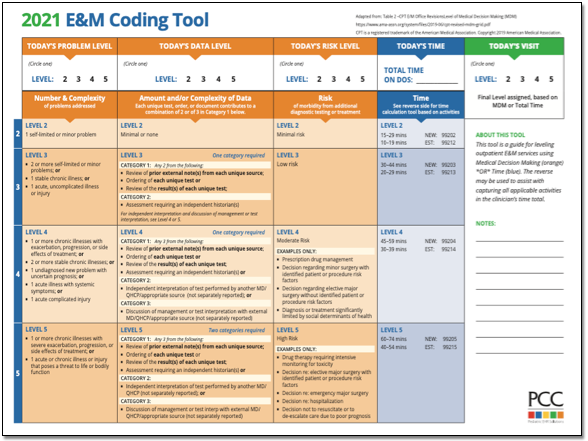
PCC’s 2021 E&M Coding Tool
PCC’s Jan Blanchard (CPC, CPEDC) developed a printable guide to E&M Coding in 2021.
Watch PCC 2021 E&M Coding Videos
You can get a quick understanding of how to level your E&M visits in 2021 by watching these videos:
- 2021 Evaluation and Management Updates: What changed? This 15 minute video explains the new way of selecting E&M codes in context with how you coded sick office visits before.
- PCC’s 2021 E&M FAQ&A: Frequently asked questions, and a live Q&A about 2021 E&M leveling.
- The Impact of 2021 E&M Coding Changes on Pediatrics: Learn about the E&M coding changes in context, and then hear PCC’s ideas about how these changes will affect the business of pediatrics.
- Pediatric Management Institute’s September COVID-19 Webinar: During the September 2020 session of the PMI’s ongoing webinar series, The Business Impact Of COVID19 On Pediatric Practices , this topic is covered along with other current topics. This recorded live webinar includes some additional Q&A.
- Attend a 2021 E&M Coding Workshop: Join PCC's Jan and come prepared with at least one complex (99214, 99215, 99205) E&M encounter note for review and/or analysis. Registration is required for this workshop and will be hosted on Zoom so that you, Jan, and your colleagues can collaborate effectively. ( Watch the Last Session )
- Attend a PCC Web Lab: PCC’s Jan Blanchard (CPC, CPEDC) hosts monthly web labs on pediatric practice management, billing, and coding.
- Watch Recorded Web Labs and More
Configure PCC EHR to Support Your Clinicians and Billers for E&M Level Selection in 2021
Your practice can add fields to your chart note protocols in order to track time spent before, during, and after the encounter by the clinician. You can also track the number of problems addressed, items reviewed for the problems, and the level of risk present.
As an example, this sample chart note protocol includes components designed to quickly note problems, time and risk.
For help customizing your protocols, check out Configure Chart Note Protocols , and get in touch with PCC Support for assistance.
Additional Resources and Guides
PCC has developed helpful blog posts that cover how to get started, frequently asked questions, and more.
Evaluate Your Practice's E&M Habits and Patterns: Your Practice Vitals Dashboard , available from within PCC EHR, provides a number of metrics, tools and recommendations related to E&M coding included on the “E&M Coding Distribution” measure.
Confessions of a Pediatric Practice Management Consultant: PCC’s Chip Hart runs a blog and podcast, covering many topics related to practice management, including E&M coding. You can find it here .
- E&M 2021 Updates: Preparing Your Pediatric Practice
- E&M Updates in 2021: Frequently Asked Questions
- AAP FAQ: E&M 2021 coding questions and answers by the American Academy of Pediatrics.
- AAP MDM Grid: A direct link to the AAP’s chart which illustrates levels of medical decision making. It includes several useful examples. (AAP hosts this file here .)
- MDM Tracker: An online tool for selecting visit level based on medical decision making in 2021.
Questions and Answers on Interpreting E&M 2021 Guidelines
PCC’s Jan Blanchard works with pediatric practices to help them interpret coding guidelines. Read below to see a selection of the 2021 E&M questions she’s received along with answers based on her current interpretation of the guidelines. As with any new way of doing things, this is a work-in-progress and will be updated as we learn more. These Q&As were updated on 2021-01-08 .
Questions and Answers
- Where can I find PCC’s 2021 MDM Tool? Here it is: PCC’s 2021 E&M Coding Tool .
- Where can I find the online MDM calculator Chip Hart shared? You can find it on the Confessions of a Pediatric Practice Management Consultant blog post entitled “Free E&M Medical Decision Making Calculator” .
CPT defines systemic symptoms this way: “Acute illness with systemic symptoms: An illness that causes systemic symptoms and has a high risk of morbidity without treatment. For systemic general symptoms, such as fever, body aches, or fatigue in a minor illness that may be treated to alleviate symptoms, shorten the course of illness, or to prevent complications, see the definitions for self-limited or minor problem or acute, uncomplicated illness or injury. Systemic symptoms may not be general but may be single system. Examples may include pyelonephritis, pneumonitis, or colitis.” (p12-14 2021 CPT Manual)
Fever had become a mainstay of complexity expression in E&M documentation. In 2021, not all fevers meet the definition of a systemic symptom. AMA says that in cases where the fever is a “general symptom in a minor illness”, it is *not* systemic. So using it to express visit complexity becomes a case-by-case determination for 2021. Things like age and other risks will be determining factors that clinicians will have to consider when they decide this point.
Furthermore, the AAP has interpreted the AMA’s position to be that you may not consider tests performed in your office in your MDM level determination. This interpretation is under review.
Maybe. “Problems” are the units of determination for MDM. So, if you treat three problems in a visit, but there are five ICDs listed, the ICDs do not inherently support higher complexity leveling. Some ICDs are reported because they represent circumstances and/or problems which complicate care but which are not specifically addressed at that visit. Documenting the role that those existing problems play in your thinking could support assigning higher Problem values to what *is* addressed.
- Can I really get credit every time a parent or guardian contributes history to a visit? Maybe. If you feel confident that the contribution they made is required for appropriate care to be rendered, yes. Document the reason for their perspective being necessary if it is not obvious. For example, little ones who can’t speak for themselves obviously require someone to give their history. But for teens, the necessity of another perspective in, say, behavioral or social concerns where objective input is valuable, document a statement to that effect and take the independent historian point(s).
Per the Elements of Medical Decision Making grid published by AMA in CPT® Evaluation and Management (E/M) Office or Other Outpatient (99202-99215) and Prolonged Services (99354, 99355, 99356, 99XXX) Code and Guideline Changes, an example of Moderate risk of morbidity from additional diagnostic testing or treatment is “Diagnosis or treatment significantly limited by social determinants of health”. I interpret these references to suggest that any SDoH which significantly limits the patient’s ability to carry out the clinician’s plan meets the Level 4 risk requirement.
According to the U.S. Department of Health, Social Determinants of Health are economic and social conditions that influence the health of people and communities. Their examples include:
- Safe housing, transportation, and neighborhoods
- Racism, discrimination, and violence
- Education, job opportunities, and income
- Access to nutritious foods and physical activity opportunities
- Polluted air and water
- Language and literacy skills
Some of these may be reported using ICD codes found in “Persons with potential health hazards related to socioeconomic and psychosocial circumstances Z55-Z65”
- Z55 Problems related to education and literacy
- Z56 Problems related to employment and unemployment
- Z57 Occupational exposure to risk factors
- Z59 Problems related to housing and economic circumstances
- Z60 Problems related to social environment
- Z62 Problems related to upbringing
- Z63 Other problems related to primary support group, including family circumstances
- Z64 Problems related to certain psychosocial circumstances
- Z65 Problems related to other psychosocial circumstances
The new MDM focus on visit leveling represents less subjectivity in discerning which parts of a service were part of the well care and which were part of the sick care.
- Do I need to document in the note the exact amount of time spent on each activity, or is it ok to just document total time? Full day totals are permissible, but I would feel better seeing at least time segments. Rough estimates for segments would do, but to expect that human brains can recreate a day’s worth of timed detail accurately for work that gets interrupted and broken up and then wrapped up after everyone else has gone home is a stretch which can be avoided.
- Is there still a Level 1 visit for nurse-only visits? Yes, for established patients only, a Level 1 nurse visit can be reported using 99211. New patient level 1 code 99201 expires on 12/31/20 and is not reportable thereafter. This is due to the identical MDM requirements for both 99201 and 99202. By 2021 standards, 99201 becomes redundant to 99202.
- If I continue to chart after hours, can I add that time for the purposes of leveling the visit? Yes. Caveat: The only after hours charting time (or any other clinical activity time) you may include in your billed time is the time spent *on the date of service*. If you chart any part of yesterday’s visit today, you may bill by time but you cannot include the time you spent today in the total you use for choosing your level. For example, if on Monday you see an established patient and spend 5 minutes reviewing records, 10 minutes in a visit, 5 minutes on a results call Monday night and 10 minutes charting on Tuesday morning, you may only bill a level 3 visit using Monday time: 5+10+5=20 minutes; Tuesday’s 10 minutes cannot count toward the leveling.
Discussions around this continue, but currently you should not expect to level using data points for test and labs you bill.
- Are a CBC and differential counted as more than 1 lab? Or for example COVID-19/Flu/RSV combo - is that 1 test or 4 tests? It depends on the number of CPTs. If CBC and differential are one CPT, it is one data point for either ordering or reviewing. If the COVID-19/Flu/RSV combo is one CPT, one point is its data value.
- Could I count one of several screenings towards data reviewed and bill for the other and not be double-dipping? This is not in the spirit of the requirement, but is still under discussion. Billing effects are impossible to explore here. The sheer variety of payers and policies means the outcome can not be predicted. Furthermore, carrier behavior makes predictions of future claim determinations little more than a guessing game.
- Do I get credit if some historians are in office and others participate over facetime, phone, etc., for the same visit? Yes. There is no cumulative credit for historians, but if someone other than the patient is required to participate that requirement is met.
- If you use a formal screen for SDoH that is scored and payable, then you can’t count that screening towards MDM, correct? Currently, that is correct.
Also, the question of whether in-house tests and labs may be used for data credit remains unanswered. I am undecided on this as yet and will count on the clinicians with whom I review encounters to help me arrive at a position on this point in future.
- We do our huddle and "run the schedule" (i.e. review referrals, lab results, vaccines, and consult notes) the day *before*, not the day of! Can we count that time when leveling each of those encounters? No. Currently, the only “billable” time is that spent by the clinician for that patient on the service date.
CPT 2021 is light on guidance on this point. “Undiagnosed new problem with uncertain prognosis: A problem in the differential diagnosis that represents a condition likely to result in a high risk of morbidity without treatment. An example may be a lump in the breast…” The AAP offered an additional example of a potentially malignant lesion in the Feb 2020 issue of the Coding Newsletter.
- If we bill for one Vanderbilt, could we then claim MDM credit for the ones from other sources? My sense of this is that doing so is *not* in the spirit of the guideline. Additionally, performing a service and not billing for it will run afoul of many insurance contracts. Also, please see above for information about Data credit for in-house labs and tests.
Example: Rash (insect bite) + been a little constipated (give some prune juice), been having stomach aches (few questions to make sure it’s nothing worrisome, asked to schedule another visit to evaluate further)…
Yes, but MDM is based on significance, not the number of problems. The total number of problems does not necessarily increase the credit you can claim for complexity in the Number and Complexity of Problems Addressed element. Rather, the most complex problem addressed (Minimal, Low, Moderate, High) in a given encounter typically represents the level of “problems addressed” which should be used for leveling. Exceptions include self-limited, minor problems (1 = Minimal while 2 = Low) and stable chronic illnesses (1 = Low, 2 = Moderate).
- Can concussion be considered an acute complicated injury - a head injury that gave other systemic symptoms? Described that way, absolutely. Be sure to familiarize yourself with the AMA’s definition of Systemic Symptoms.
From the AMA: “Trained clinicians apply common language usage meanings to terms such as high, medium, low, or minimal risk and do not require quantification for these definitions (though quantification may be provided when evidence-based medicine has established probabilities). For the purposes of MDM, level of risk is based upon consequences of the problem(s) addressed at the encounter when appropriately treated. Risk also includes MDM related to the need to initiate or forego further testing, treatment, and/or hospitalization.”
From the AMA: “… decision about hospitalization includes consideration of alternative levels of care…Examples may include a psychiatric patient with a sufficient degree of support in the outpatient setting or the decision to not hospitalize a patient with advanced dementia with an acute condition that would generally warrant inpatient care, but for whom the goal is palliative treatment.”
For example, if PCC EHR automatically records your time with a chart open, you would be required to close and reopen every chart every time you were interrupted while charting in order for it to be accurate. If you had to actively click a button to stop and start a timer, it would be an ever-present timer that required their attention. Users shared this would be distracting at best and annoying at worst. Most users were happier to state their own estimates of how much time was spent, either in total or in segments to be used for totaling when they were sure services were complete for the whole day.
Related Articles
- Here are some related articles in Other Pediatric Practice Resources > Coding and Documentation :
How to Code for Immunizations and Administration
ICD-10 Training Resources
Diagnostic Code Sets (SNOMED-CT, ICD-10, ICD-9) in PCC’s Software and Services
CPT II in PCC
PCC’s Billing Drop-In Sessions
2021 Evaluation & Management Workshop (11-17)
Advertisement
2021 E/M coding and documentation rules
Billing, Coding & Payments | Advocacy Resources | January 15, 2021
New rules for reporting outpatient office evaluation and management (E/M) services took effect Jan. 1. The coding and documentation revisions, adopted by the American Medical Association’s CPT Editorial Panel and approved by the Centers for Medicare and Medicaid Services (CMS) substantially simplify code selection and documentation.
With the exception of 99201, which was deleted, the E/M outpatient visit code numbers remain as follows:
- 99202-99205: New Patient Office Visits
- 99211-99215: Established Patient Office Visits

Code selection – Medical Decision Making (MDM) or Time
- Medical decision making (MDM)
Although you should still perform a medically appropriate history and/or physical exam, it/they do not determine the level of service.
Coding based on MDM
The four levels of MDM remain the same: straightforward, low, medium, and high. The three core elements have remained essentially the same and they are:
Number and complexity of problem(s)
- A problem is the disease, condition, illness, symptom, or other matter addressed at the encounter with or without a diagnosis being established.
- Multiple new or established conditions may be addressed at the same encounter and may affect medical decision making.
- Each symptom is not necessarily a problem. Symptoms may cluster around a specific diagnosis or conditions.
- The final diagnosis for a condition does not, in itself, determine the complexity or risk.
- Multiple problems of lower severity may, in the aggregate, create a higher risk due to interaction.
Amount and/or complexity of data to be reviewed and analyzed. Data includes:
- Tests, documents, orders, or independent historians
- Independent interpretation of tests
- Discussion of management or test interpretation with external physician or health care professional.
Risk of complications and/or morbidity or mortality of patient management decisions made at visit:
- Includes possible management decisions selected and those not selected.
- An example of moderate risk might include prescription drug management or a diagnosis or treatment significantly limited by social determinants of health.
- An example of high risk might include drug therapy requiring intensive monitoring for toxicity.
To qualify for a level of MDM, two of the three elements for that level of decision making must be met. The College’s matrix on MDM provides more detail on how to determine the level of MDM and code selection.
Documentation Tip:
When coding based on MDM, physician notes should address the elements on which the MDM determination is based. Note that while you should document any history and/or physical exam performed, this is no longer a basis for code selection. There is no need to review a certain number of systems, or check boxes.
Coding based on time
The biggest change in E/M coding and documentation is that code selection for outpatient office visits can now be based entirely on time spent on the day of the encounter even if counselling and coordination of care do not dominate the encounter. Clinical staff time does not count. Time includes:
- All time spent by the physician or qualified health professional (QHP) for the patient on the date of the encounter including:
♦ Preparing to see the patient (e.g., review of tests).
♦ Obtaining and/or reviewing separately obtained history.
♦ Performing a medically appropriate examination and/or evaluation.
♦ Counseling and educating patient/family/caregiver.
♦ Ordering medications, tests, or procedures.
♦ Referring and communicating with other health care professionals (if not separately reported).
♦ Documenting clinical information in the patient’s health record.
♦ Independently interpreting results (not separately reported) and communicating to patient/family/caregiver.
♦ Care coordination (not separately reported).
- Time is defined in increments.
- If time exceeds level 5, the add-on prolonged service code can be used.
Time for determining visit level
Note: For CPT Code 99211, which describes visits that do not require the presence of a physician, time is not used.
Documentation tips:
- Complete charting and follow-up on the day of the encounter. Only time spent on the day of the encounter can be counted.
- On the day of the visit, keep track of and document time spent on getting ready for the patient encounter and follow-up work afterwards, such as care coordination.
- Only provider time counts – not nurse or medical assistant time. But provider time spent reviewing nurse, medical assistant or scribe documentation does count.
Coding tips:
- To determine whether to code based on MDM or time, compare visit level based on time with level based on MDM and use the highest level that can be documented using either method.
- You may find new and/or complex patient visits are best coded based on time, especially patients that require a fair amount of counseling, care coordination, chart reviews and/or reviewing test results.
- Many follow-up visits may be best coded based on medical decision making, since they may still involve medical complexity and risk but may not require a great deal of time.
When to Use the Prolonged Service Codes
There are some important changes in coding for prolonged services. First, the prolonged service code may only be used when coding based on time and only with the level 5 visit codes (99205, 99215). Second, the new codes describe shorter time increments of 15 minutes.
CPT Code 99417 should be used when billing payers other than Medicare. This code, which should only be billed with 99205 or 99215, describes an additional 15 minutes beyond the minimum time of the office visit code. It can be billed in multiple units for each additional 15 minutes of time. Additional time less than 15 minutes should not be reported.
HCPCS Code G2212 was created by CMS and is specific to Medicare . It should be reported for each additional 15 minutes of prolonged service beyond the maximum time for CPT Codes 99205 or 99215. See tables below:
Additional resources:
Webinar: New Outpatient E/M Coding Rules for 2021
ACAAI Coding Toolkit
College Matrix on MDM
The College’s Advocacy Council will continue to provide information on the new codes and coding for 2021 – we have you covered.


CPT code 95165 – What’s a dose for Medicare billing?
Medicare defines a dose, for billing purposes only, as 1cc of extract and does not cover dilutions. Medicare reimbursement…

Coding Conundrum – E/M plus Testing
Recently we received a query from a member about coding an oral challenge and an office visit on the…

2024 G2211 Add-On Code
If you bill G2211, it is important that you document the reason for billing the code. Supporting documentation must…
Privacy Overview
Disclaimer » Advertising
- HealthyChildren.org
- Previous Article
- Next Article
EXAMPLE: MDM FOR LEVEL 5 OFFICE E/M
Example: time-based code selection, more to come, office e/m 2021: level 5 visits.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- CME Quiz Close Quiz
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
American Academy of Pediatrics; Office E/M 2021: Level 5 Visits. AAP Pediatric Coding Newsletter November 2020; 16 (2): 5–7. 10.1542/pcco_book199_document002
Download citation file:
- Ris (Zotero)
- Reference Manager
This article provides information and examples of the changes that will be implemented for office and other outpatient evaluation and management (E/M) codes provided on or after January 1, 2021. Previous articles in this series, which began in the January 2020 AAP Pediatric Coding Newsletter ™ , have addressed
The reason for the changes (ie, simplification of code selection and reduction of documentation burden)
A basic overview of what is changing (ie, code selection based on medical decision-making [MDM] or on a physician’s or qualified health care professional’s [QHP’s] total time on the day of service)
More in-depth reviews of the use of time and MDM, including each element of MDM
Nonphysician E/M visits ( 99211 )
Level 2–4 visits
To view all AAP Pediatric Coding Newsletter content related to E/M 2021, visit https://coding.aap.org and click on “Coding Resources.”
Please note that information provided in this article is based on the instructions published by the American Medical Association at the time of publication. Changes or corrections may occur prior to official release of Current Procedural Terminology ( CPT ® ) 2021 .
In this issue, we explore example scenarios that might be reported with codes at level 5 of the office E/M services ( 99205 and 99215 ) for dates of service on and after January 1, 2021.
As previously noted, for each level of office E/M service, the MDM is the same for new or established patients. For level 5 codes selected based on MDM, 2 of 3 elements must be met or exceeded to support a high level of MDM.
Table 1 shows the elements of MDM to support high-complexity MDM.
High-Complexity Medical Decision-making
Abbreviation: QHP, qualified health care professional.
Examples included in italic text are not included in Current Procedural Terminology ® and are intended only to illustrate how the preceding bullet point might be met. The elements of medical decision-making (MDM) may vary across individual patient services, and code selection for each service should reflect the extent of MDM by the physician or other QHP.
A drug that requires intensive monitoring is a therapeutic agent that has the potential to cause serious morbidity or death. Monitoring for therapeutic effect is not equivalent to monitoring for toxicity or other adverse effect. Drug therapy requiring intensive monitoring for toxicity may be by a laboratory test, a physiologic test, or imaging. The monitoring affects the level of MDM in an encounter in which it is considered in the management of the patient (eg, monitoring of ototoxicity via audiometry findings).
When selecting a code based on the physician’s or QHP’s total time spent directed to care of the individual patient, on the date of the encounter, 60 to 74 minutes is required to report 99205 and 40 to 54 minutes to support 99215 . Total time includes face-to-face and non–face-to-face time (eg, time spent entering information into the medical record) directed to the care of the individual patient on the date of a visit.
A 6-year-old is seen by his primary care pediatrician due to his parents’ concerns of recent bed-wetting and new complaints of abdominal pain. History obtained from the parents indicates that the child has been thirsty but not eating as usual for 2 days. Complaints of abdominal pain began the night before this visit. The child has lost 8 pounds since his last visit 2 months ago. After examination, urinalysis, and review of multiple laboratory findings (eg, blood glucose, blood gases, complete blood cell count, blood urea nitrogen with creatinine), the pediatrician diagnoses new onset type 1 diabetes with ketoacidosis and orders intravenous fluids and immediate hospitalization. The pediatrician calls a pediatric endocrinologist, who agrees to assume management of the patient in the hospital. Code 99215 is reported.
Each of the 3 elements of MDM support a level 5 service, though only 2 of 3 are required ( Table 2 ). If the pediatrician in this example ordered the urinalysis and a comprehensive metabolic panel ( 80053 ) in lieu of multiple individual laboratory tests, the amount and complexity of data reviewed and analyzed would be moderate rather than extensive, but the problems addressed and risk of the management would still be high, supporting a level 5 visit.
Medical Decision-making for Level 5 Office Evaluation and Management
Category 2 of the data reviewed and analyzed is the independent interpretation of a test performed by another physician/other QHP. Any 2 of 3 categories is sufficient to support an extensive amount and/or complexity of data reviewed and analyzed.
A decision regarding hospitalization that results in a decision to not admit the patient but to closely monitor on an outpatient basis supports a high risk of complications and/or morbidity or mortality.
An 8-year-old patient is referred to a pediatrician for follow-up care after an observation stay that resulted in a new diagnosis of asthma. Prior to the visit, the pediatrician’s clinical staff obtain health records from the hospital and a local health clinic where the child has received primary care, including immunizations, which were brought up to date at the beginning of the last school year.
At the visit, the child is accompanied by his paternal grandmother, who has been the only caregiver for the past 4 months. Whereabouts of the child’s mother are unknown, and his father is deceased. The grandmother voices intent to become her grandchild’s permanent guardian and requests education on asthma control and assistance in helping the child cope with grief. The grandmother also notes that the child attends a summer camp program 3 days of the week when she works. The staff of the summer camp have expressed concern that the child wanders away from activities if not constantly watched and is alternately withdrawn from and aggressive toward the other children and counselors.
After examination and reviewing the child’s asthma control test, the pediatrician discusses and answers questions from the grand-mother about asthma management, control medications, and quick relief medications. After a general psychosocial assessment tool is completed and scored, the physician talks briefly with the patient and then counsels the patient and grandmother about seeing a clinical social worker for counseling and assistance with access to community resources, as needed. The grandmother agrees to an appointment with the social worker. A follow-up appointment for recheck of asthma control is scheduled. The physician’s total time on the date of the visit is 65 minutes, including preservice record review, the face-to-face visit, and post-visit care coordination including writing a referral letter to the social worker, a prior authorization for counseling services, and documentation of the encounter. Code 99205 is reported based on time.
Had the patient in this example been established to the pediatrician, the total time of 65 minutes would support prolonged service in addition to code 99215 . One unit of prolonged service 99417 is reported for each full 15-minute period beyond the minimum time required to support the office E/M service. See Table 3 for time requirements for new and established patients. CPT does not place a limit on the number of units reported per encounter for code 99417 .
At the time of publication, CPT and the Centers for Medicare & Medicaid Services were in conflict with regard to when prolonged services ( 99417 ) begin. We have presented the timing from CPT as part of this newsletter. For more information or to check for a resolution, please visit www.aap.org/coding .
Code 99417 is reported only with codes 99205 and 99215 and only when the office E/M code was selected based on time .
Codes 99354 and 99355 (direct prolonged services in an out-patient setting) will no longer be reported for prolonged service on the date of an office E/M service provided in 2021.
Time Requirements for Code 99417
Abbreviations: E/M, evaluation and management; QHP, qualified health care professional.
As we draw closer to 2021, watch for additional information and examples in future issues of AAP Pediatric Coding Newsletter . You can also find more information on coding for office E/M services in Chapter 7 of Coding for Pediatrics 2021 and Pediatric Office-Based Evaluation and Management Coding: 2021 Revisions .
Recipient(s) will receive an email with a link to 'Office E/M 2021: Level 5 Visits' and will not need an account to access the content.
Subject: Office E/M 2021: Level 5 Visits
(Optional message may have a maximum of 1000 characters.)
Citing articles via
Email alerts.
Advertising Disclaimer »
Affiliations
- CEU Quizzes
- Coding Hotline
- Online ISSN 1934-5143
- Print ISSN 1934-5135
- Pediatrics Open Science
- Hospital Pediatrics
- Pediatrics in Review
- AAP Grand Rounds
- Latest News
- Pediatric Care Online
- Red Book Online
- Pediatric Patient Education
- AAP Toolkits
- AAP Pediatric Coding Newsletter
First 1,000 Days Knowledge Center
Institutions/librarians, group practices, licensing/permissions, integrations, advertising.
- Privacy Statement | Accessibility Statement | Terms of Use | Support Center | Contact Us
- © Copyright American Academy of Pediatrics
This Feature Is Available To Subscribers Only
Sign In or Create an Account
- ACS Foundation
- Diversity, Equity, and Inclusion
- ACS Archives
- Careers at ACS
- Federal Legislation
- State Legislation
- Regulatory Issues
- Get Involved
- SurgeonsPAC
- About ACS Quality Programs
- Accreditation & Verification Programs
- Data & Registries
- Standards & Staging
- Membership & Community
- Practice Management
- Professional Growth
- News & Publications
- Information for Patients and Family
- Preparing for Your Surgery
- Recovering from Your Surgery
- Jobs for Surgeons
- Become a Member
- Media Center
Our top priority is providing value to members. Your Member Services team is here to ensure you maximize your ACS member benefits, participate in College activities, and engage with your ACS colleagues. It's all here.
- Membership Benefits
- Find a Surgeon
- Find a Hospital or Facility
- Quality Programs
- Education Programs
- Member Benefits
- E/M Coding and Billing Res...
- Office/Outpatient E/M Visi...
Office/Outpatient E/M Codes
2021 e/m office/outpatient visit cpt codes.
The tables below highlight the changes to the office/outpatient E/M code descriptors effective in 2021.
More details about these office/outpatient E/M changes can be found at CPT® Evaluation and Management (E/M) Office or Other Outpatient (99202-99215) and Prolonged Services (99354, 99355, 99356, 99XXX) Code and Guideline Changes.
All specific references to CPT codes and descriptions are © 2023 American Medical Association. All rights reserved. CPT and CodeManager are registered trademarks of the American Medical Association.
Download the Office E/M Coding Changes Guide (PDF)

Reporting Level 5 E/M Code 99205
by Meghann Drella | Published on Jun 27, 2014 | Medical Coding

Documentation Requirements for CPT Code 99205
What is high risk diagnosis, common mistakes to avoid in billing cpt code 99205.
CPT code 99205 is a high-level evaluation and management code used for the evaluation and management of new patients, for both office and outpatient visits. CPT code 99205 can be selected for new patient visits lasting 60+ minutes on the date of encounter. The total time required for reporting 99205 is 60-74 minutes. Reporting CPT code 99205 accurately is often difficult for coders. This is where a professional medical coding company can support.

Free up your team for what matters most. Get a quote for our medical coding services !
Call (800) 670-2809
Code99205 requires 3 key components:
- High-level medical decision-making: The evaluation and management of a patient demand intricate decision-making processes. This involves properly analyzing and interpreting medical records, diagnostic tests, and relevant information to formulate an accurate diagnosis and treatment plan.
- Thorough medical history or examination: Proper assessment of a patient’s condition necessitates a comprehensive history or examination. This involves gathering details about the patient’s medical background, current symptoms, past treatments, and any other crucial factors influencing their healthcare.
- Session duration typically ranging from 60-74 minutes: CPT code 99205 denotes an extended duration of service compared to other evaluation and management codes. The session duration encompasses both face-to-face and non-face-to-face time dedicated to the patient encounter.
While the new patient codes (99201–99205) require that all three key components (history, exam and medical decision making) be satisfied, the established patient codes (99211–99215) require that only two components of the three key be satisfied.
The terms “high complexity/high severity” signifies that the patient’s risk of death/morbidity is high – extreme and/or the patient has a moderate – high risk of death without treatment or a high probability of severe, prolonged, functional impairment. So to justify the use of 99205, the patient’s condition, whether acute or chronic must pose an immediate threat to life or physical function.
High risk diagnosis may be:
- Sudden change to neurological status such as weakness/sensory loss, TIA (Transient Ischemic Attack), seizure
- Chronic illnesses with severe progression, worsening or side effects of treatment
- Acute/chronic injury or illnesses that pose a threat to physical function or life itself such as acute MI, multiple trauma, pulmonary embolus
Avoiding common mistakes are crucial when billing CPT Code 99205. Ensure accurate reimbursement and compliance with professional coding guidelines.
Here are some common mistakes to avoid:
- Insufficient documentation: One of the most common mistakes is not providing enough documentation to support the level of service billed. Ensure that the documentation includes a detailed history of present illness, comprehensive review of systems, comprehensive examination of multiple organ systems, and medical decision making of high complexity.
- Overbilling: Billing for a level of service higher than warranted by the patient encounter can lead to overbilling and potential audits. Make sure the documentation accurately reflects the complexity of the patient’s condition and the level of service provided.
- Under coding: Conversely, under coding occurs when providers bill for a lower level of service than warranted by the patient encounter. Ensure that the documentation accurately reflects the complexity of the patient’s condition to avoid under coding and potential loss of revenue.
- Lack of medical necessity: Ensure that the documentation clearly demonstrates the medical necessity of the services provided. Medical necessity is essential for justifying the level of service billed and ensuring reimbursement.
- Failure to document time spent: CPT code 99205 requires encounter time. So, keep track of the time you spend with the patient. Failure to document the total time spent with the patient and the specific amount of time spent on counseling or coordination of care can lead to billing errors and potential denials.
- Mixing-up patient status: This code is specifically designated for new patients, so it’s crucial to differentiate it from established patient codes to ensure accurate billing and documentation. Familiarizing the distinct criteria for each code can streamline the process and prevent any potential errors in reimbursement.
By avoiding these common mistakes and ensuring accurate documentation, healthcare providers can bill CPT Code 99205 appropriately, leading to accurate reimbursement and compliance with coding guidelines. Modifiers used for 99205 depend on specific billing circumstances. For example, modifier “-25” is of use, if a significant and separately identifiable service is provided on the same day. Billing 99205 with other codes depends on the services provided and payer rules. Proper use of modifiers and adherence to billing guidelines are essential when billing for multiple services.
Maximize your reimbursement and minimize errors with our customized coding services.
Get a Free Trial!

Meghann Drella possesses a profound understanding of ICD-10-CM and CPT requirements and procedures, actively participating in continuing education to stay abreast of any industry changes.
More from This Author
Facebook Twitter LinkedIn
Related Posts
- Proven Strategies to Maximize Cash Flow in Medical Practices
- Importance of Accurate and Compliant Coding in Minimizing Denials
- Optimizing Cost Efficiency: The Advantages of Outsourcing Medical Billing
- Appointment Scheduling
- Dental Insurance Verification
- Healthcare News
- Insurance Credentialing
- Insurance Verification and Authorizations
- Medical Billing
- Medical Coding
- Medical Outsourcing
- Specialty Billing
- Specialty Coding
Connection denied by Geolocation Setting.
Reason: Blocked country: Russia
The connection was denied because this country is blocked in the Geolocation settings.
Please contact your administrator for assistance.


Getting clear on the new coding rules can help you eliminate bloated documentation and improve reimbursement to reflect the value of your visits.
THOMAS WEIDA, MD, FAAFP, AND JANE WEIDA, MD, FAAFP
Fam Pract Manag. 2022;29(1):26-31
Author disclosures: no relevant financial relationships.

In 2021, significant changes were adopted for the documentation guidelines for outpatient evaluation and management (E/M) visit codes. Most notably, medical decision making or time became primary drivers of visit level selection, rather than the number of history and physical exam bullets.
In this article, we review the context for these changes, describe them briefly, and offer a quick reference tool to help physicians apply the new rules in practice.
The revisions to the E/M outpatient visit codes reduced administrative burden by eliminating bullet points for the history and physical exam elements.
Code level selection is now simplified — based on either medical decision making or total time.
The authors' one-page coding reference tool can help simplify the new rules.
HOW WE GOT HERE
In the 2019 Medicare physician fee schedule final rule, released in November 2018, the Centers for Medicare & Medicaid Services (CMS) adopted revisions to the outpatient E/M codes in order to reduce administrative burden. (See https://www.cms.gov/newsroom/fact-sheets/final-policy-payment-and-quality-provisions-changes-medicare-physician-fee-schedule-calendar-year .) Originally scheduled for implementation in 2021, these changes would have combined visit levels 2–4 into a blended payment rate (e.g., one rate for 99202-99204 and one rate for 99212-99214), among other changes.
In response, the American Medical Association (AMA) convened a joint CPT Editorial Board and Relative Value Scale Update Committee (RUC) workgroup to build on the changes and propose some alternatives. The workgroup's goals were to decrease administrative burden, payer audits, and unnecessary medical record documentation while ensuring that payment of E/M services is resource-based.
The workgroup approved significant revisions to the outpatient office visit E/M codes. Code 99201 was deleted. The history and/or physical examination and the counting of bullets were eliminated as components for code selection (although history and/or physical examination documentation should still be performed as medically appropriate). Medical decision making (MDM) or time could be used for code level selection. Changes were made to the code descriptors for 99202-99205 and 99211-99215, the definition of medical decision making, and the calculation of time, and a shorter prolonged services add-on code was created. CMS adopted these new E/M coding guidelines. As a result of the changes to medical decision making and time-based coding, the RUC revised the 2021 relative value units (RVUs) for office visit E/M codes. Most of the values increased, yielding an overall increase of more than 10%.
CODING BASED ON MEDICAL DECISION MAKING
For outpatient E/M coding, medical decision making now has three components:
Number and complexity of problems addressed at the encounter,
Amount and/or complexity of data to be reviewed and analyzed,
Risk of complications and/or morbidity or mortality of patient management.
There are four levels of decision making for each of these components: straightforward, low complexity, moderate complexity, and high complexity.
To determine the level of code for a visit, two of the three components must meet or exceed that level of coding. ( See the table .) For example, if the patient has multiple problems addressed at the encounter, but the data is limited and the risk of complications is low, then the level of medical decision making would be low. New patient codes 99202-99205 and established patient codes 99212-99215 use the same components and levels of decision making for code selection.
Determining medical decision making usually starts with identifying the number and complexity of problems addressed and then determining the data or risk components that support that medical decision making. If a second component does not meet or exceed the problem component, then a lower level of decision making is appropriate. The set of tables below illustrate the essential concepts of these code levels. Each level has specific criteria for each component.
Straightforward medical decision making: Codes 99202 and 99212 include one self-limited or minor problem with minimal or no data and minimal risk.
An example of a 99202 or 99212 is an otherwise healthy patient with cough and congestion due to the common cold.
Low complexity medical decision making: Codes 99203 and 99213 include two or more self-limited or minor problems, one stable chronic illness, or one acute uncomplicated illness or injury.
The data component requires one of two categories to establish the level. Category 1 data requires at least two items in any combination of the following: each unique source's prior external notes reviewed, each unique test result reviewed, or each unique test ordered. Tests include imaging, laboratory, psychometric, or physiologic data. A clinical lab panel, such as a complete blood count, is a single test. Of note, if a test is ordered, the review of that test is included with the ordering, even if the review is done at a subsequent visit. Tests ordered outside of an encounter may be counted in the encounter in which they are analyzed. Category 2 data includes significant history given by an independent historian. Parents giving the history for their child is a typical example.
The risk component is low. There is low risk of morbidity from additional diagnostic testing or treatment.
An example of a 99203 or 99213 is a sinus infection treated with an antibiotic. Although the prescription makes the risk component moderate, the one acute uncomplicated illness is a low-complexity problem, and there are no data points.
Moderate complexity medical decision making: Codes 99204 and 99214 include two or more stable chronic illnesses, one or more chronic illnesses with exacerbation, progression, or side effects of treatment, one undiagnosed new problem with uncertain prognosis, one acute illness with systemic symptoms, or one acute complicated injury. A patient who is not at a treatment goal, such as a patient with poorly controlled diabetes, is not stable. Systemic general symptoms such as fever or fatigue in a minor illness (e.g., a cold with fever) do not raise the complexity to moderate. More appropriate would be fever with pyelonephritis, pneumonitis, or colitis.
The data component requires one of three categories to establish the level. Category 1 data requires at least three items in any combination of the following: each unique source's prior external notes reviewed, each unique test result reviewed, each unique test ordered, or independent historian involvement. Physicians cannot count tests that they or someone of the same specialty and same group practice are interpreting and reporting separately (e.g., electrocardiogram, X-ray, or spirometry). Category 2 data includes the independent interpretation of a test performed by another physician/other qualified health care professional (QHP) (not separately reported). For instance, if a chest X-ray was ordered and the ordering clinician included the interpretation in the visit documentation, this would qualify for data point Category 2. However, if the ordering clinician bills separately for the interpretation of the X-ray, then that cannot be used as an element in this category and would be an element for Category 1. Category 3 data includes discussion of management or test interpretation with an external physician/QHP (not separately reported).
The risk component may include prescription drug management, a decision for minor surgery with patient or procedure risk factors, a decision for elective major surgery without patient or procedure risk factors, or social determinants of health (SDOH) that significantly limit diagnostic or treatment options, such as food or housing insecurity. For prescription drug management, renewing pre-existing chronic medications would qualify. Documentation that the physician is managing the patient for the condition for which the medications are being prescribed would help establish validity in the use of this criterion for MDM.
An example of a 99204 or 99214 is a patient being seen for follow-up of hypertension and diabetes, which are well-controlled. An example using SDOH would be a patient with chronic knee pain and a positive anterior drawer test who needs imaging of the knee but cannot afford this care. Documenting that the patient cannot afford to obtain an MRI of the knee at this time, which significantly limits your ability to confirm the diagnosis and recommend treatment, adds to the risk component.
High complexity medical decision making: Codes 99205 and 99215 include one or more chronic illnesses with a severe exacerbation, progression, or side effects of treatment, or one acute or chronic illness or injury that poses a threat to life or bodily function.
The data component requires two of three categories to establish the level. These data categories are the same as those for 99204 and 99214, and they follow the same rules.
The risk component may include drug therapy requiring intensive monitoring for toxicity. Decisions regarding elective major surgery with patient or procedure risk, emergency major surgery, hospitalization, or “do not resuscitate” orders are also high risk. Intensive prescription drug monitoring is typically supported by a laboratory test, physiologic test, or imaging, and is done to evaluate for complications of the treatment. It may be short-term or long-term. Long-term monitoring is at least quarterly. An example would be monitoring for cytopenia during antineoplastic therapy. Monitoring the therapeutic effect of a treatment, such as glucose monitoring during insulin therapy, is not considered intensive prescription drug monitoring.
An example of a 99205 or 99215 is a patient with severe exacerbation of chronic heart failure who is admitted to the hospital.
CODING OUTPATIENT E/M VISITS
Time-based coding.
An alternative method to determine the appropriate visit level is time-based coding. A major change is that total time now includes both face-to-face and non-face-to-face services personally performed by the physician/QHP on the day of the visit. Additionally, time-based coding is no longer restricted to counseling services. Instead, it includes the following:
Preparing to see the patient (e.g., reviewing external test results),
Obtaining and/or reviewing separately obtained history,
Performing a medically appropriate examination and/or evaluation,
Counseling and educating the patient, family, or caregiver,
Ordering medications, tests, or procedures,
Referring and communicating with other health care professionals (when not separately reported),
Documenting clinical information in the electronic or other health record,
Independently interpreting results (not separately reported with a CPT code) and communicating results to the patient, family, or caregiver.
Care coordination (not separately reported with a CPT code).
Time spent by clinical staff cannot count toward total time. However, time spent by another physician/QHP (not a resident physician) in the same group can be included. If a nurse practitioner performs the initial intake and the physician provides the assessment and plan, both of those times can be counted, although only one person's time can be counted while they are discussing the case with each other. The visit should be billed under the clinician who provided the substantive portion (more than half) of the time, although both clinicians need to be identified in the medical record. Time spent must be documented in the note. It is advisable to specifically document the time spent and the activities performed both face-to-face and non-face-to-face.
The amount of total time required for each level of coding changed under the new time-based coding guidelines. (See the “Total time ” table.)
PROLONGED VISIT CODES
When time on the date of service extends beyond the times for codes 99205 or 99215, prolonged visit codes can be used. The AMA CPT committee developed code 99417 for prolonged visits, and Medicare developed code G2212. These are added in 15-minute increments in addition to codes 99205 or 99215. Code G2212 can be added once the maximum time for 99205 or 99215 has been surpassed by a full 15 minutes, whereas code 99417 can be added once the minimum time for 99205 or 99215 has been surpassed by a full 15 minutes. Less than 15 minutes is not reportable. Multiple units can be reported. Prolonged visit codes cannot be used with the shorter E/M levels, i.e., 99202-99204 and 99212-99214. (See “Prolonged services ” tables.) Clinicians should consult with individual payers to determine which code to use — G2212 or 99417.
SIMPLIFIED CODING AND DOCUMENTATION
The revisions to the outpatient E/M visit codes reduced administrative burden by eliminating bullet points for the history and physical exam elements. Only medically appropriate documentation is required. Code level selection is simplified — based on either medical decision making or total time. By applying these changes, primary care clinicians can eliminate bloated documentation and improve reimbursement reflecting the value of the visit.
Continue Reading

More in FPM
More in pubmed.
Copyright © 2022 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
An official website of the United States government
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
CMS Newsroom
Search cms.gov.
- Physician Fee Schedule
- Local Coverage Determination
- Medically Unlikely Edits
Evaluation & Management Visits
This page contains guidance regarding documentation and payment under the Medicare Physician Fee Schedule for evaluation and management (E/M) visits.
- Physician Fee Schedule (PFS) Payment for Office/Outpatient Evaluation and Management (E/M) Visits – Fact Sheet (PDF) - Updated 01/14/2021
- Evaluation and Management (E/M) Visit Frequently Asked Questions (FAQs) (PDF)
- Evaluation and Management Services MLN Publication
- FAQs: Split (or Shared) Visits and Critical Care Services (PDF) : Posted 4/7/2022

IMAGES
VIDEO
COMMENTS
Summary. To summarize, here are the three common reasons to code a level 5 office visit: Total time. ≥ 40 minutes for established patients; ≥ 60 minutes for new patients. Pre-op visit. Major ...
Effective January 1, 2021. Shorter prolonged services code to capture each 15 minutes of critical physician/other QHP work beyond the time captured by the office or other outpatient service E/M code. Used only when the office/other outpatient code is selected using time. For use only with 99205, 99215.
Let's take a dive into the components of a level 5 office visit based on the 2021 guidelines! #medicalcoding #medicalcoderE&M Guidelines for 2021 - https://w...
Yes, for established patients only, a Level 1 nurse visit can be reported using 99211. New patient level 1 code 99201 expires on 12/31/20 and is not reportable thereafter. This is due to the identical MDM requirements for both 99201 and 99202. By 2021 standards, 99201 becomes redundant to 99202.
The biggest change in E/M coding and documentation is that code selection for outpatient office visits ... the prolonged service code may only be used when coding based on time and only with the level 5 visit codes (99205, 99215). Second, the new codes describe shorter time increments of 15 minutes. CPT Code 99417 should be used when billing ...
Changes or corrections may occur prior to official release of Current Procedural Terminology ( CPT ®) 2021. In this issue, we explore example scenarios that might be reported with codes at level 5 of the office E/M services ( 99205 and 99215) for dates of service on and after January 1, 2021. As previously noted, for each level of office E/M ...
Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and low level of medical decision making. When using time for code selection, 30-44 minutes of total time is spent on the date of the encounter. 99204. Office or other outpatient visit for the ...
Medicare was going to pay another single rate for established patient codes 99212, 99213, and 99214. Level-5 visits (99205, 99215) would have separate rates to reflect the increased complexity those codes represent. ... Medicare created a new HCPCS Level II code for use in place of CPT ® code +99417 when billing Medicare for prolonged office ...
CPT code 99205 is a high-level evaluation and management code used for the evaluation and management of new patients, for both office and outpatient visits. CPT code 99205 can be selected for new patient visits lasting 60+ minutes on the date of encounter. The total time required for reporting 99205 is 60-74 minutes.
• Prolonged total time on the date of office or other outpatient services • 15-minute increments after the total time of the highest-level service (ie, 99205 or 99215) has been exceeded • Only use when the office or other outpatient service has been selected using time alone as the basis
Internists selected the 99215 level of care for only about 4.86% of established office patients in 2020. The Medicare allowable reimbursement for this level of care is $183.19. Effective January 1, 2021, this level of care requires high complexity MDM or a total of 40 - 54 minutes spent before, during and after the visit on the date of the ...
You should continue to use the CMS 1995 and/or 1997 Documentation Guidelines for Evaluation and Management Services for all E/M categories except office/other outpatient services (99202-99215). Use the 2021 CPT® documentation guidelines for office visits (99202-99215), only. 3. Do you have to document both total time and medical decision ...
Split (or Shared) E/M Services. CPT Codes 99202-99205, 99212-99215, 99221-99223, 99231-99239, 99281-99285, & 99291-99292. A split (or shared) service is an E/M visit where both a physician and NPP in the same group each personally perform part of a visit that each 1 could otherwise bill if provided by only 1 of them.
To determine the level of code for a visit, two of the three components must meet or exceed that level of coding. (See the table.)For example, if the patient has multiple problems addressed at the ...
Evaluation & Management Visits. This page contains guidance regarding documentation and payment under the Medicare Physician Fee Schedule for evaluation and management (E/M) visits. Physician Fee Schedule (PFS) Payment for Office/Outpatient Evaluation and Management (E/M) Visits - Fact Sheet (PDF) - Updated 01/14/2021.
Level 5, new patient evaluation and management (E/M) code 99205 Office or other outpatient visit for the evaluation and management of a new patient, which requires these 3 key components: A comprehensive history; A comprehensive examination; Medical decision making of high complexity.Counseling and/or coordination of care with other physicians, other qualified health care professionals, or ...
For example, 99202 Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and straightforward medical decision making … has a current time range of 15-29 minutes. Beginning Jan. 1, 2024, the provider must meet or exceed 15 minutes of total service time before you can bill this code by time.
Level 5 visits are the most complex cases and require more time or very complex decision-making. ... In 2004, the most common claim was level 3. However, in 2021, level 4 and 5 billing codes made up the majority of emergency department claims. The share of claims billed at level 4 rose from 25 percent in 2004 to 35 percent in 2021 ...